Abstract
Study design:
Clinical and radiographic evaluation of the shoulders of tetraplegic and paraplegic patients who attend rehabilitation program.
Objectives:
The objective of this study is to establish the usefulness of radiography as a trial exam for shoulder pain in spinal cord injured patients.
Setting:
Hospital das Clinicas—UNICAMP. Campinas, Sao Paulo, Brazil.
Methods:
Thirty-two shoulders of 16 patients were evaluated by clinical exam and radiography. Patients were divided into two groups: paraplegic and tetraplegic. A control group of 16 normal volunteer subjects was selected.
Results:
Shoulder pain was reported in 88.89% of tetraplegic and 42.85% of paraplegic. The time of injury ranged from 1.5–22 years (mean 7.88 years); patients had a mean age of 34.68 years (range, 21–57 years). The acromioclavicular joint (ACJ) space ranged from 0.03–0.7 cm on the right side and 0.15–0.7 cm on the left side, with a mean of 0.37 and 0.41 cm, respectively. No correlation was found between shoulder pain and gender, age or time since injury. There was a trend to correlation between shoulder pain and type of injury with tetraplegic having a tendency to pain symptoms. On average, tetraplegic had smaller ACJ.
Conclusions:
The small number of patients in this study did not allow us to confirm the hypothesis that X-ray finding may indicate risk for shoulder pain in spinal cord injury patients. A work with a greater number of subjects could demonstrate association between shoulder pain and the reduced acromioclavicular distance, making plain radiography a trial exam for spinal cord-injured patients.
Similar content being viewed by others
Introduction
Shoulder pain is the most common painful process among spinal cord injury (SCI) patients with pain in the upper extremity (UE; 71%), followed by pain in the wrist (53%), hands (43%) and elbows (35%).1 The high incidence of shoulder pain in this population is due to the greater strain placed on the joint because they use their UE in daily activities (DA). On the other hand, persons with severe high SCI have no muscle support or sensation around their shoulders and, therefore, may be prone to injuries.2
Campbell and Koris3 described several etiologies for shoulder pain in these patients including capsular contracture or capsulitis, rotator cuff (RC) tears, anterior instability, RC impingement, osteoarthrosis and osteonecrosis for the acute pain group. The chronic pain group presented as causes: anterior instability, multidirectional instability, capsular contracture or capsulitis, Charcot arthropathy, RC tear, RC impingement and scapular pain. Other authors also proposed that diseases such as osteoarthritis and osteoporosis of the glenohumeral and acromioclavicular joints (ACJ) were the causes of shoulder pain in patients with SCI.4 As these diseases can be easily identified with clinical history and physical exam, it is very important to emphasize the central role of anamnesis and physical examination, including all specific tests that are reliable according to the literature.
As shoulder pain is very common in SCI patients, leading to decrease in life quality, and as rehabilitation is necessary to improve this scenario, it is mandatory that the physician recognizes the patient in the initial stage of the painful process or even detect a subclinical situation to avoid the pain. This study intends to find signs on plain radiographs that could be related to shoulder pain and, therefore, this inexpensive and available examination could be used to predict risk factor for developing shoulder pain among patients in rehabilitation program, leading to preventive measures.
Patients and methods
The Biomechanics and Locomotor-System Rehabilitation Laboratory of the University Hospital of UNICAMP (State University of Campinas) offers a gait-training program with neuromuscular stimulation. For the tetraplegic, it consists of sessions in which the patients’ trunk is stabilized by a harness support and then steps are taken with the help of a device that alternately contracts both quadriceps, followed by a withdraw reflex that is achieved through the stimulation of the fibular nerve. For the paraplegic, the same stimulation pattern is applied but they use walkers, as they can have trunk control alone.5, 6
Sixteen patients from the Spinal Cord Injuries’ Rehabilitation Ambulatory (outpatient clinic) participated in this study and 16 normal subjects voluntarily composed the control group. The study was approved by the local ethics committee.
Shoulder pain was not an inclusion criteria, as the intention was to identify subclinical lesions. SCI subjects were divided into paraplegics and tetraplegics.
All the patients were diagnosed at the time of trauma with magnetic resonance imaging, defining the level of injury. All subjects follow a rehabilitation program of two periods of 1 h 30 min through two different days.
Exclusion criteria were indisposition for a clinical assessment or for the radiography of the shoulders.
All clinical history and physical exams were performed by the same doctor on a comfortable place, with the patient seated on a chair or wheelchair and undressed above the waist. Local inspection was performed and exam continued with judicious palpation of the bony prominences and soft tissues, looking for sites of tenderness, which could suggest specific pathologies. Assessment of the shoulder range of motion (ROM) was performed passively and actively. Specific shoulder tests were performed for pain and instability.
Plain film radiography was acquired from both shoulders of all subjects in the true anteroposterior, Zanca, axilary and lateral scapular incidences. The radiographic images were taken by conventional X-ray and individually analyzed by two different doctors (orthopedic specialist and an experienced medical radiologist) and reviewed together.
The measurement of the ACJ space was performed considering the distance between the medial tip of the acromion and the lateral border of the clavicle (Figure 1a). The acromiohumeral interval was measured from a thin line of dense cortical bone, marking the inferior aspect of the acromion at a point directly above the humeral head and recorded as the smallest distance between this line and the articular cortex of the humeral head (Figure 1b). The subacromion space was considered to be either greater than or less than 7 mm. The measures were taken by the doctors who analyzed the X-rays, and a mean value was obtained.
The glenohumeral space was classified as normal, decreased or subluxated/dislocated. The humeral head was either normal or with irregularities; the glenohumeral joint was normal or with degenerative changes; the presence of calcifications or other type of changes was observed.
Statement of ethics
All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Statistics
The statistics performed was based on descriptive analysis for categorical variables (frequency tables) and position and dispersion measurements for continuous variables. Towards comparison of proportions, the exact test of Fisher was applied.
Towards comparison of continuous or sortable measures between two groups, the Mann–Whitney test was used, and between three groups, the Kruskal–Wallis test was performed.
Towards comparison of continuous measures or sortable measures between sides and presence of pain, the method of generalized estimation equations (GEE) was used.
Spearman's correlation coefficient (from −1 to 1) was used to assess linear relation between two variables, values next to the extremes indicating positive or negative correlation, close to zero meaning no correlation at all.
The P-level chosen as demonstrating significance for the results obtained was 5%.
The data obtained in this study were analyzed by the computer program SAS System for Windows (Statistical Analysis System), version 9.2., SAS Institute Inc., 2002–2008, Cary, NC, USA.
Results
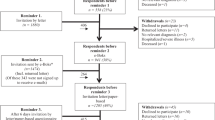
Among the 16 patients, there were seven paraplegics and nine tetraplegics. Three patients from the paraplegic and eight from the tetraplegic group complained of shoulder pain (Figure 2). There were four women and 12 men. Two women and nine men had shoulder pain. All patients had chronic pain (mean 16.8 months). The time of injury ranged from 1.5–22 years (mean 7.88 years). The patients had a mean age of 34.68 years (range, 21–57 years). Patient's characteristics are summarized in Table 1 and the control group in Table 2. The descriptive analysis between shoulder pain regarding age and time since injury can be verified on Table 3.
None of the patients presented physical exam suggestive of RC tear, impact syndrome, shoulder instability, capsular contracture or capsulitis. The physical exam of each patient and the specific tests performed can be seen on Tables 4 and 5.
The ACJ space ranged from 0.03–0.7 cm on the right and 0.15–0.7 cm on the left side, with a mean of 0.37 and 0.41 cm for the right and left side, respectively. All acromiohumeral intervals were greater than 7 mm. Patient 4 presented a round increased density of 0.7 cm on the greater tuberosity without clinical relevance. Patients 8 and 9 had previous clavicle fracture, without repercussion, and patient 13 had a firearm projectile on the left supraclavicular region. The radiographic features of the patients are presented on Table 6 and the control group on Table 7.
Comparison of gender and age between paraplegic, tetraplegic and control group, and comparison of time since injury between paraplegic and tetraplegic, showed that the groups are homogeneous for age and time since injury, but not for gender (P=0.0268, Fisher's exact test).
The analysis of variance for repeated measures was used towards comparison of the acromioclavicular space between groups (tetraplegic, paraplegic and control) and between sides. There was no significant correlation between side and group (P=0.1113). We didn’t find any difference on the ACJ measures when sides were compared (P=0.8901). But we did find a difference in these measures in relation to groups (P=0.0041). Tukey's test pointed out the difference between the tetraplegic and paraplegic, and between tetraplegic and controls. The paraplegic group did not differ from the control. Because of the difference between the groups regarding gender, the analysis of the ACJ space was remade using gender as covariate. However, the results did not change after the adjustment. The tetraplegic group differs from the control group and from the paraplegic (Tukey–Kramer test). On average, the tetraplegic group had ACJ measures smaller than the other two groups.
The complaint of shoulder pain in the SCI patients was classified in ‘yes’ or ‘no’ on each side. The analysis of the associated factors was made using the generalized estimating equation, considering the factor side also. The studied variables were: gender, age, time since lesion and type of lesion, as well as ACJ measures and the ROM of the shoulder. There was no difference between shoulder pain and gender (P=0.4927), age (P=0.3537) or time since injury (P=0.7612), and the effect of the side was also not significant. There was a trend to correlation between shoulder pain and the type of lesion (P=0.0597), with tetraplegic patients having a tendency to pain symptoms. Regarding shoulder pain, the radiographic measurement was not able to discriminate the subjects (P=0.4521).
We also analyzed the correlation between the ACJ distance and numerical variables such as ROM, age and time since injury. We found moderate linear correlation only for the passive external rotation; greater the external rotation, greater the distance of the ACJ (r=0.53954, P=0.0310 for the right side and r=0.54676, P=0.0284 for the left side).
All other radiological features did not present correlation with either shoulder pain or type of lesion (paraplegia × tetraplegia).
Discussion
It is general consensus that UE pain is common in 1/3–1/2 of SCI population, most frequently on the shoulder. 1, 2, 7, 8, 9, 10 This might be because the UE is needed for DA and, therefore, is submitted to increased stress.1 This scenario may interfere with their function and independence, because UE pain usually limits shoulder mobility.7
Overall, 68.75% (11/16) of the studied patients presented shoulder complaints, being 88.89% (8/9) of the tetraplegic patients, and 42.85% (3/7) of the paraplegic patients, corroborating the finding reported by literature of a higher incidence of complaints in SCI, particularly tetraplegic patients.7, 8, 10, 11 In our study, there was no difference between pain and type of injury (paraplegic × tetraplegic; P=0.0597). Dalyan et al.1 reported the same. Maybe with an increase on the number of patients studied, we would find an actual statistical relation between these variables.
The shoulder, particularly the scapular–humeral joint, is primarily designed for providing mobility and to position hand in space. Whenever this complex joint mechanism starts to act as a load supporting joint, as in the case of SCI patients, degenerative changes manifest early, making DA difficult.10, 12
As in our study, other authors have reported no significant difference in time since injury between patients with and without UE pain.1, 7, 8, 9
We found no correlation between shoulder pain and age as Samuelsson et al.13 also described, but there was a significant difference on the basis of age, demonstrated by Lal,7 being higher the incidence of shoulder pain in older patients.
In our study, we found no difference between right and left sides, neither regarding gender. Dalyan et al.1 presented similar results with these variables. Samuelsson et al.13 did not demonstrate correlation of pain and gender. Two other studies had different results, reporting female gender as a higher risk for shoulder pain.7, 9
SCI patients place greater strain on the shoulder. The cause of pain is related to the absence of muscle support or sensation in patients with severe high SCI, making these patients prone to injuries. It is also related to muscle imbalance explaining why tetraplegic have more shoulder pain than paraplegic.2
Our study showed that tetraplegic had smaller ACJ space. Lal7 found 100% of involvement of the ACJ and attributed to the badly transmitted forces on the shoulder joint in wheelchair activities, the cause of rapid progression of degenerative changes, leading to an increase incidence of radiographic changes in tetraplegic older than 30 years, with predilection of the ACJ. However, in our study, regarding shoulder pain, the radiographic measurement was not able to discriminate the subjects (P=0.4521).
Conventional radiography has limited potential to evaluate soft tissues injuries, which are better identified by ultrasound or magnetic resonance imaging. We didn’t perform either of these exams, but on the clinical tests, none of the patients had features of soft tissue injuries. We all know that clinical history and physical exam are the cornerstone of diagnosis, with complementary exams used to confirm the hypothesis. Kivimäki and Ahoniemi2 in his study with ultrasound findings noted very small difference in changes of the supraspinatus tendon between subject with or without SCI. Previous authors have already described radiographic signs of RC tears.14, 15, 16 None of the patients in our study had these findings. Kivimäki and Ahoniemi2 found a mean ACJ space of 3.7 mm in SCI patients and 4 mm in able-bodied, which is similar to our work.
We found that the greater the ACJ space, the greater was the external rotation. No explanation was found, but possibly it is associated to the less ROM on shoulders of tetraplegic patients in whom we found smaller ACJ.
There is a need for UE pain prevention and management programs for SCI patients in the early phases of rehabilitation and during ongoing care, even for decades. It is very complex as SCI patients are unable to rest their shoulders because they are used for DA. It is paramount to eliminate damaging patterns, manage the early signs of strain and overuse, teach alternative techniques of DA, strengthen the muscles acting around the shoulder and optimize posture to achieve a normal alignment of shoulder, head and spine. Environmental changes are necessary. There is a recent study that described that persons with SCI and limited shoulder ROM at discharge are more limited in their activities 1 year later than those without limited shoulder ROM,17 reinforcing the importance of early and maintained rehabilitation of SCI patients.
Difficulties were found while performing the physical examination of the tetraplegic patients as some of them, because of the level of injury, were not able to do the tests that required active motion. Therefore, for those patients it becomes rather important that they are constantly assessed and a complementary exam performed to identify a shoulder lesion.
Conclusion
No correlation was found between shoulder pain and gender, age or time since injury. There was no difference between sides also. On average, tetraplegic had smaller ACJ.
As it was not possible to analyze the correlation between presence of shoulder pain, the ACJ measure and type of injury at the same time because of the reduced number of patients, we suggest a work with a greater number of subjects. This could demonstrate association between shoulder pain and the reduced ACJ, making plain radiography a trial exam for SCI patients, enabling us to identify those at risk for developing shoulder pain and, therefore, preventive measures can be made. The small number of patients in this study did not allow us to confirm the hypothesis that X-ray finding may indicate risk for shoulder pain in SCI patients.
References
Dalyan M, Cardenas DD, Gerard B . Upper extremity pain after spinal cord injury. Spinal Cord 1999; 37: 191–195.
Kivimäki J, Ahoniemi E . Ultrasonographic finding in shoulders of able-bodied, paraplegic and tetraplegic subjects. Spinal Cord 2008; 46: 50–52.
Campbell CC, Koris MJ . Etiologies of shoulder pain in cervical spinal cord injury. Clin Orthop Related Res 1996; 322: 140–145.
Hastings J, Goldstein B . Paraplegia and the shoulder. Phys Med Rehabil Clin N Am 2004; 15: vii, 699–718.
Carvalho DCL, Zanchetta MC, Sereni JM, Cliquet Jr A . Metabolic and cardiorespiratory responses of tetraplegic subjects during treadmill walking using neuromuscular eletrical stimulation and partial body weight support. Spinal Cord 2005; 43: 400–405.
Ferro FP, Gonzales HJ, Ferreira DM, Cliquet Jr A . Electrical stimulation and treadmill gait in tetraplegic patients: assessment of its effects on the knee with magnetic resonance imaging. Spinal Cord 2008; 46: 124–128.
Lal S . Premature degenerative shoulder changes in spinal cord injury patients. Spinal Cord 1998; 36: 186–189.
Jensen MP, Hoffman AJ, Cardenas DD . Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord 2005; 43: 704–712.
Gutierrez DD, Thompson L, Kemp B, Mulroy SJ . The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. J Spinal Cord Med 2007; 30: 251–255.
Silfverskiold J, Waters RL . Shoulder pain and functional disability in spinal cord injury patients. Clin Orthop Related Res 1991; 272: 141–145.
Sie IH, Waters RL, Adkins RH, Gellman H . Upper extremity pain in the post rehabilitation spinal cord injured patient. Arch Phys Med Rehabil 1992; 73: 44–48.
Ninomyia AF, Jesus CLM, Auletta LL, Rimkus CM, Ferreira DM, Filho AZ et al. Shoulders of patients with spinal cord injuries submitted to rehabilitation program—a clinical and ultrasound-based assessment. Acta Ortop Bras 2007; 15: 109–113.
Samuelsson KAM, Tropp H, Gerdle B . Shoulder pain and its consequences in paraplegic spinal cord-injured, wheelchair users. Spinal Cord 2004; 42: 41–46.
Harrison SH . The painful shoulder. J Bone Joint Surg 1949; 31-B: 418–422.
Cotton RE, Rideout DF . Tears of the humeral rotator cuff. J Bone Joint Surg 1964; 46-B: 314–328.
Weiner DS . Superior migration of the humeral head. A radiological aid in the diagnosis of tears of the rotator cuff. J Bone Joint Surg 1970; 52: 524–527.
Eriks-Hoogland IE, de Groot S, Post MW, van der Woude LH . Correlation of shoulder range of motion limitations at discharge with limitations in activities and participation one year later in persons with spinal cord injury. J Rehabil Med 2011; 43: 210–215.
Acknowledgements
This study was supported by the State of Sao Paulo Foundation for Research—FAPESP.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Medina, G., Nascimento, F., Rimkus, C. et al. Clinical and radiographic evaluation of the shoulder of spinal cord injured patients undergoing rehabilitation program. Spinal Cord 49, 1055–1061 (2011). https://doi.org/10.1038/sc.2011.64
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.64
Keywords
This article is cited by
-
Prevalence of upper extremity pain in a population of people with paraplegia
Spinal Cord (2018)
-
Is sport practice a risk factor for shoulder injuries in tetraplegic individuals?
Spinal Cord (2015)
-
Risk factors for shoulder pain in patients with spinal cord injury: a multicenter study
MUSCULOSKELETAL SURGERY (2015)
-
Acromioclavicular joint arthrosis in persons with spinal cord injury and able-bodied persons
Spinal Cord (2013)