Key Points
-
Explains the differences between minimal intervention dentistry, minimally invasive dentistry, micro-dentistry, atraumatic restorative treatment and selective tissue excavation.
-
Examines the foundations of minimal intervention dentistry.
-
Considers the implementation of modern concepts into everyday clinical practice.
Abstract
The concept of minimal intervention dentistry is based on all the factors that affect the onset and progression of disease and therefore integrates concepts of prevention, control and treatment. The field of minimal intervention dentistry is wide, including the detection of lesions as early as possible, the identification of risk factors (risk assessment) and the implementation of preventive strategies and health education for the patient. When the effects of the disease are present, in the form of a carious lesion, other therapeutic strategies are required, but in this case the least invasive solutions should be chosen, for example remineralisation, therapeutic sealants and restorative care aimed at conserving the maximum amount of sound tissue. This article aims to enlighten dental practitioners as to the foundations of minimal intervention dentistry in order to help them in the implementation of modern concepts into everyday clinical practice.
Similar content being viewed by others
Introduction
Cariology has advanced over the past 30 years with scientific advances in the knowledge of the caries process in terms of its pathogenesis, its transmission, the demineralisation and remineralisation continuum, the mode of action of fluoride, but also with respect to the great technological developments in biomaterials, equipment for the detection of caries lesions and methods for cavity preparation. This new scientific knowledge combined with developments both technological and technique related, impose that both medically and ethically, the sole pertinent therapeutic model that is relevant is one that is based on prevention and treatment using the least invasive of approaches. This 'rational' model of care is known as minimal intervention dentistry and is applicable not only to cariology but to periodontology and all other areas of dentistry.1,2,3boxed-text
Studies conducted in France in the early 2000s indicated that dental practitioners had not yet integrated this concept of cariology into practise4,5,6,7 even though, since the 1990s, Elderton had already denounced traditional approaches to conservative dentistry when considered in isolation.8,9,10 Indeed, traditional oral care, which comprises largely conservative/operative dentistry, including scaling and polishing, has very little impact on the oral health of patients both in children and adults because the patient finds himself/herself caught in a repeat restoration spiral of care, where successive replacement of restorations results in the restoration increasing in size each time the restoration is renewed, leading to eventual loss of the tooth.2,8,11,12Figure 1 illustrates a patient, aged 33 at the time of the photograph, who has, judging by the number of endodontic treatments present, been obliged to visit the dentist on numerous occasions in the past. The problem of oral hygiene has not been resolved and, the caries process, which is very aggressive, has not been halted. Restorative and endodontic treatment do not in themselves solve the problems of oral health. The reasons for the delay in adopting minimal intervention in routine dental practice are certainly many, including lack of initial training and continuous education of practitioners in this subject area, lack of time and personnel for its easy implementation in general practice, lack of knowledge and appreciation of preventive and non-invasive therapeutic strategies by the public authorities and their lack of incorporation into financial reimbursement schemes. Adapted from a series first published in French in Réalités Cliniques, the BDJ offers a series of articles on the general topic of minimal intervention dentistry written by international authors to help the dental practitioner integrate this concept into daily clinical practice.
What are the differences between minimal intervention dentistry, minimally invasive dentistry, micro-dentistry, atraumatic restorative treatment and selective tissue excavation and how should each be defined?
A primary source of confusion for practitioners concerns the terminology used since 'minimally invasive dentistry' and 'minimal intervention dentistry' are often used interchangeably although they describe different concepts. This first section aims to define the terms most commonly used that are associated with minimal intervention.
Minimal intervention dentistry
Minimal intervention dentistry is a concept of patient care that deals with the causes of dental disease and not just the symptoms.1,13,14 Based on biological solutions rather than purely restorative, minimal intervention is based entirely on prevention and control of oral disease.
Primary prevention focuses on preventing new cases of oral diseases. It uses collective prevention measures such as artificial fluoridation of water or school oral health programmes. At the individual level, primary prevention aims to prevent the early colonisation of childrens' teeth by cariogenic bacteria (for example, Streptococcus mutans, one of the species associated with the initiation of the caries process). Prevention also includes the management of other factors such as a cariogenic diet rich in fermentable carbohydrates, coupled with poor oral hygiene habits.
Secondary prevention aims at preventing the disease from becoming established and progressing. This includes screening to detect carious lesions at the earliest possible stage so that appropriate treatment can be delivered.
Tertiary prevention, for its part, aims to prevent recurrence of disease as well as the failure of preventive and restorative care initially implemented.
The concept of minimal intervention is based on all the factors that affect the onset and progression of disease and therefore integrates concepts of prevention, control and treatment. The field of minimal intervention dentistry is wide, including the detection of lesions as early as possible, the identification of risk factors (risk assessment) and the implementation of preventive/control strategies and health education for the patient. When the effects of the disease are present, in the form of a carious lesion, other therapeutic strategies are required, but in this case the least invasive solutions should be chosen for example, remineralisation, therapeutic sealants and restorative care aimed at conserving the maximum amount of dental tissue.
Minimally invasive dentistry, ultraconservative and micro-dentistry
Minimally invasive dentistry, ultraconservative and micro-dentistry are terms that embrace operative restorative approaches that respect both the dental tissues and patient's comfort. The excavation of dentine caries is performed with the objective of preserving not only sound tooth tissue but also that tissue which has the potential to remineralise. The use of adhesive biomaterials is preferred, for example, resin composite of different viscosities selected according to the clinical situation and glass-ionomer cements, particularly those of high viscosity.15 One should not confuse minimal intervention dentistry and minimally invasive dentistry since the latter is merely a component of the minimal intervention treatment (care) plan (Fig. 2). In traditional dentistry the preparation and restoration of cavities are the only and systematic response to the presence of carious lesions. With a minimal intervention approach, the placement of restorations is an ancillary phase of the overall management of patient care where restorations are indicated only when the lesion has advanced to frank cavitation and where remineralisation techniques have reached their limits. Micro-dentistry is performed preferably using optical aids (magnification, microscopes, intra-oral cameras) and can also make use of more sophisticated devices other than traditional rotary instruments mounted on a contra-angle handpiece or air-turbine, such as chemo-mechanical, air-abrasion, sono-abrasion and laser systems.
Atraumatic restorative treatment (ART)
The atraumatic restorative treatment (ART) approach is part of the therapeutic armamentarium of minimal intervention dentistry and is minimally invasive. The manual selective excavation of tissues destroyed by the caries process, involving excavation of the infected dentine while conserving the affected dentine, is described in a separate article later in this series. A sealant restoration is then placed, which comprises a conventional adhesive restoration combined with the sealing of adjacent pits and fissures. In the case of ART, the restoration and sealant are placed simultaneously using high-viscosity glass-ionomer cement. Initially, this approach was proposed for the management of patients in developing countries because it can be performed using only manual instruments. The excellent results from clinical studies suggest that it also has its applications in industrialised countries especially for patients with multiple caries lesions during the stabilisation and motivation phase. Figure 3 illustrates the prophylactic phase in the management of the caries process. This patient consulted the dental department of the University Hospital of Clermont-Ferrand for restoration of his teeth. Many open lesions can be observed as well as the presence of abundant plaque. Brushing was impossible because the many open dentine caries lesions made it very painful. ART was performed in quadrants. This not only improved the aesthetics but more importantly oral hygiene recommendations could then be implemented by the patient.
Minimal intervention dentistry: building the treatment (care) plan?
'Rational' clinical practice is based on four key elements:
-
1
Control of the disease by identifying and managing the risk factors
-
2
The detection and remineralisation of early lesions
-
3
Minimally invasive surgical intervention
-
4
Where possible the repair rather than replacement of defective restorations.15,16
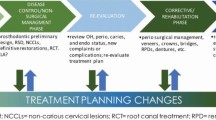
Clinically, a cariology-based care plan comprises three main phases: the diagnostic phase, the prophylactic phase and the (recall) monitoring phase (Fig. 4).
The diagnostic phase
The diagnostic phase allows one to understand why the disease (caries) has occurred and is used to evaluate the severity of the damage caused. It includes the determination of the individual caries risk factors and detection of carious lesions (presence and activity) for the application during the next phase, of non-invasive therapeutic solutions.
The determination of caries risk of individual patients is based on the identification of the presence of pathological and protective factors that affect the demineralisation and remineralisation process respectively but also on the identification of risk predictors.17,18,19 Within the term 'risk predictors' are grouped all those factors which, while being not directly related to the caries process itself, have been shown in longitudinal studies to be correlated with the appearance of new lesions. The main risk predictors are past exposure to caries, the presence of cavitated caries lesions or recent restorations placed due to caries, as well as demographic factors relating to the patient in terms of age, level of education and disabilities that potentially expose the patient to risk habits – a teenager with uncontrolled eating habits, the elderly where oral hygiene is more difficult to maintain due to loss of motor skills, education associated with the level of care one takes of oneself and harmful lifestyles, which expose people to situations of poor hygiene and failure to seek care.20,21,22,23,24,25,26
Figure 5 illustrates the imbalance between protective factors, pathological factors and risk predictors that exist in the case of high caries risk, a concept developed by Featherstone.27,28,29 Indeed, the weight of the caries risk predictors is important and entails the need to counterbalance them in the implementation of measures tailored to the pathological factors present for each clinical case.
Prophylactic phase
The second prophylactic phase aims to readjust the balance between pathological and protective factors. During this phase, measures required to curb the phenomena of demineralisation and to initiate remineralisation are implemented. Emphasis is placed on recommendations relating to hygiene and dietary habits, antibacterial therapy, prescription of appropriate fluoride measures and the placement of preventive sealants. In the case of patients with cavitated lesions involving the dentine, atraumatic restorative care can complement the arsenal of prophylactic or partial excavation of caries. ART reduces the bacterial load, places a glass-ionomer cement restoration, eliminates the cavity responsible for retention of the plaque biofilm and protects the dentine allowing the patient to develop efficient oral hygiene.
Follow-up monitoring and maintenance
The third phase includes follow-up monitoring and maintenance. It concerns the reinforcement of patient education, monitoring the effectiveness of all preventive and control measures implemented for example, fluoride and preventive sealants, and therapeutic measures for example, the integrity of therapeutic sealants and restorations. During follow-up visits, potential failures can be intercepted and the recall interval adjusted based on new clinical findings and the behaviour of the patient.30,31,32
Restorations
The placement of restorations has long been regarded, incorrectly, as the primary solution to manage the caries process. The restorative component is of course not excluded, when required, from a minimal intervention care plan, but has no effect on the aetiologic factors and is not an essential component unlike the other three described above. Restorative treatment is therefore still required when the caries process has resulted in significant loss of dental tissue, in order to eliminate the retention of plaque within cavities and restore physiological masticatory function and aesthetics. The restorative phase can fit between control and surveillance. It must follow a minimally invasive approach, where caries removal/cavity preparation is delayed until there are cavitated dentine lesions and through the use of adhesive materials, these cavities can remain minimally invasive.13,15,16,33,34,35,36,37 Such cavities are, by definition, conservative in design and there is no so-called 'extension for prevention', although sometimes it might be necessary to remove some sound tissue for example, reducing a weakened cusp or making retentive features. In the case of lesions close to the pulp, the complete removal of all the carious dentine is now called into question since glass-ionomer cements allow ion exchange leading to the remineralisation of demineralised tissue.38,39,40,41,42,43,44 Defective restorations are not systematically removed and replaced. These radical solutions need to be rethought and nuanced; polishing reduces the indications for the complete replacement of the restoration, the margins of restorations can be sealed and restorations can be repaired.15,45,46,47,48
Conclusions
High quality modern dentistry based on minimal intervention focuses on prevention and control of disease with operative dental interventions that are limited to the absolute minimum.1 Ideally, care strategies must meet certain criteria, namely effectiveness, 'does it work in dental practice?' and efficiency, 'is the cost–effectiveness adequate?' Although there is a growing scientific evidence-base about the effectiveness of minimal intervention dentistry, it is nevertheless clear that the problem of efficiency arises in the context of implementation levels within current healthcare systems in different countries.
References
Sheiham A . Minimal intervention in dental care. Med Princ Pract 2002; 11 (Suppl 1): 2–6.
Elderton R J . Preventive (evidence-based) approach to quality general dental care. Med Princ Pract 2003; 12 (Suppl 1): 12–21.
Bowley J . Minimal intervention prosthodontics: current knowledge and societal implications. Med Princ Pract 2002; 11 (Suppl 1): 22–31.
Doméjean-Orliaguet S, Tubert-Jeannin S . La prise en charge des lésions carieuses en France. Clinic 2009; 30: 229–288.
Doméjean-Orliaguet S, Léger S, Auclair C, Gerbaud L, Tubert-Jeannin S . Caries management decision: influence of dentist and patient factors in the provision of dental services. J Dent 2009; 37: 827–834.
Doméjean-Orliaguet S, Tubert-Jeannin S, Riordan P J, Espelid I, Tveit A B . French dentists' restorative treatment decisions. Oral Health Prev Dent 2004; 2: 125–131.
Tubert-Jeannin, S, Doméjean-Orliaguet S, Riordan P J, Espelid I, Tveit A B . Restorative treatment strategies reported by French university teachers. J Dent Educ 2004; 68: 1096–1103.
Elderton R J . Iatrogenesis in the treatment of dental caries. Proc Finn Dent Soc 1992; 88: 25–32.
Elderton R J . Overtreatment with restorative dentistry: when to intervene? Int Dent J 1993; 43: 17–24.
Elderton R J, Mjör I A . Changing scene in cariology and operative dentistry. Int Dent J 1992; 42: 165–169.
Sheiham A . Impact of dental treatment on the incidence of dental caries in children and adults. Community Dent Oral Epidemiol 1997; 25: 104–112.
Elderton R J . Clinical studies concerning re-restoration of teeth. Adv Dent Res 1990; 4: 4–9.
Mount G J . A new paradigm for operative dentistry. Aust Dent J 2007; 52: 264–270.
Featherstone J D . The science and practice of caries prevention. J Am Dent Assoc 2000; 131: 887–899.
Tyas M J, Anusavice K J, Frencken J E, Mount G J . Minimal intervention dentistry - a review. FDI Commission Project 1–97. Int Dent J 2000; 50: 1–12.
Mount G J, Ngo H . Minimal intervention: a new concept for operative dentistry. Quintessence Int 2000; 31: 527–533.
Beck J D . Risk revisited. Community Dent Oral Epidemiol 1998; 26: 220–225.
Stamm J W, Stewart P W, Bohannan H M, Disney J A, Graves R C, Abernathy J R . Risk assessment for oral diseases. Adv Dent Res 1991; 5: 4–17.
Bader J D, Perrin N A, Maupomé G, Rush W A, Rindal B D . Exploring the contributions of components of caries risk assessment guidelines. Community Dent Oral Epidemiol 2008; 36: 357–362.
Tagliaferro E P, Pereira A C, Meneghim Mde C, Ambrosano G M . Assessment of dental caries predictors in a seven-year longitudinal study. J Public Health Dent 2006; 66: 169–173.
Tinanoff N . Dental caries risk assessment and prevention. Dent Clin North Am 1995; 39: 709–719.
Enjary C, Tubert-Jeannin S, Manevy R, Roger-Leroi V, Riordan P J . Dental status and measures of deprivation in Clermont-Ferrand, France. Community Dent Oral Epidemiol 2006; 34: 363–371.
Azogui-Lévy S, Lombrail P, Riordan P J et al. Evaluation of a dental care program for school beginners in a Paris suburb. Community Dent Oral Epidemiol 2003; 31: 285–291.
de Saint Pol T . La santé des plus pauvres. Insee Premiere 2007; 1161.
Haut Comité de la santé publique. La progression de la précarité en France et ses effets sur la santé. Rennes: Haut Comité de la santé publique, 1998.
Powell L V . Caries prediction: a review of the literature. Community Dent Oral Epidemiol 1998; 26: 361–371.
Featherstone J D . The caries balance: contributing factors and early detection. J Calif Dent Assoc 2003; 31: 129–133.
Featherstone J D . The caries balance: the basis for caries management by risk assessment. Oral Health Prev Dent 2004; 2 (Suppl 1): 259–264.
Featherstone J D, Doméjean-Orliaguet S, Jenson L, Wolff M, Young D A . Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc 2007; 35: 703–707, 710–713.
National Institute for Clinical Excellence. Dental recall - recall interval between routine dental examinations. London: NICE, 2004.
Beirne P, Clarkson J E, Worthington H V . Recall intervals for oral health in primary care patients. Cochrane Database Syst Rev 2007; 4: CD004346.
Beirne P, Forgie A, Clarkson J, Worthington H V . Recall intervals for oral health in primary care patients. Cochrane Database Syst Rev 2005; 18: CD004346.
Mount G J . Minimal intervention dentistry: rationale of cavity design. Oper Dent 2003; 28: 92–99.
Mount G J, Ngo H . Minimal intervention: advanced lesions. Quintessence Int 2000; 31: 621–629.
Mount G J, Ngo H . Minimal intervention: early lesions. Quintessence Int 2000; 31: 535–546.
Peters M C, McLean M E . Minimally invasive operative care. I. Minimal intervention and concepts for minimally invasive cavity preparations. J Adhes Dent 2001; 3: 7–16.
Peters M C, McLean M E . Minimally invasive operative care. II. Contemporary techniques and materials: an overview. J Adhes Dent 2001; 3: 17–31.
Ngo H . Glass-ionomer cements as restorative and preventive materials. Dent Clin North Am 2010; 54: 551–563.
Ngo H C, Mount G, Mc Intyre J, Tuisuva, J, Von Doussa R J . Chemical exchange between glass-ionomer restorations and residual carious dentine in permanent molars: an in vivo study. J Dent 2006; 34: 608–613.
Ricketts D . Management of the deep carious lesion and the vital pulp dentine complex. Br Dent J 2001; 191: 606–610.
Ricketts D . Deep or partial caries removal: which is best? Evid Based Dent 2008; 9: 71–72.
Ricketts D N, Kidd E A, Innes N, Clarkson J . Complete or ultraconservative removal of decayed tissue in unfilled teeth. Cochrane Database Syst Rev 2006; 3: CD003808.
Bjørndal L . Indirect pulp therapy and stepwise excavation. Pediatr Dent 2008; 30: 225–229.
Bjørndal L, Reit C, Bruun G et al. Treatment of deep caries lesions in adults: randomized clinical trials comparing stepwise vs. direct complete excavation, and direct pulp capping vs. partial pulpotomy. Eur J Oral Sci 2010; 118: 290–297.
Criteria for placement and replacement of dental restorations: an international concensus report. Int Dent J 1988; 38: 193–194.
Moncada G, Martin J, Fernández E, Hempel M C, Mjör, I A, Gordan V V . Sealing, refurbishment and repair of Class I, Class II defective restorations: a three-year clinical trial. J Am Dent Assoc 2009; 140: 425–432.
Moncada G, Fernández E, Martín J, Arancibia C, Mjör I A, Gordan V V . Increasing the longevity of restorations by minimal intervention: a two-year clinical trial. Oper Dent 2008; 33: 258–264.
Cardoso M, Baratieri L N, Ritter A V . The effect of finishing and polishing on the decision to replace existing amalgam restorations. Quintessence Int 1999; 30: 413–418.
Acknowledgements
The authors would like to thank Claudie Damour-Terrasson, publishing director of the Groupe Information Dentaire, Paris France, for the authorisation of translation and publication of the series in the BDJ, and Christopher Holmgren for his assistance with the translation of the present article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Featherstone, J., Doméjean, S. Minimal intervention dentistry: part 1. From 'compulsive' restorative dentistry to rational therapeutic strategies. Br Dent J 213, 441–445 (2012). https://doi.org/10.1038/sj.bdj.2012.1007
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2012.1007
This article is cited by
-
Top tips for minimally invasive dentistry in primary care
British Dental Journal (2023)
-
A scoping literature review on minimum intervention dentistry for children with dental caries
British Dental Journal (2022)
-
Effect of silver diamine fluoride solution application on the bond strength of dentine to adhesives and to glass ionomer cements: a systematic review
BMC Oral Health (2020)
-
Minimum intervention oral healthcare for people with dental phobia: a patient management pathway
British Dental Journal (2020)
-
KISS principle and non AGP dentistry for pandemic periods and beyond
BDJ In Practice (2020)