Key Points
-
Identify the possible causes of post-treatment apical periodontitis and approach these cases accordingly.
-
Recognise the alternatives for management of teeth with post-treatment apical periodontitis.
-
Understand the technical difficulties in performing retreatment
Abstract
Endodontic treatment failure is usually characterised by the presence of post-treatment apical periodontitis, which may be persistent, emergent or recurrent. The major aetiology of post-treatment disease is persistent intraradicular infection, but in some cases a secondary intraradicular infection due to coronal leakage or an extraradicular infection may be the cause of failure. Understanding the causes of endodontic treatment failure is of paramount importance for the proper management of this condition. Teeth with post-treatment apical periodontitis can be managed by either nonsurgical endodontic retreatment or periradicular surgery, both of which have very high chances of restoring the health of the periradicular tissues and maintaining the tooth function in the oral cavity. This review article focuses on the aetiological factors of post-treatment apical periodontitis and discusses the indications and basics of the procedures for optimal clinical management of this condition.
Similar content being viewed by others
Introduction
The main objectives of endodontic treatment are to prevent or treat apical periodontitis so that the tooth can be retained in the oral cavity in healthy conditions. The occurrence of signs and/or symptoms of disease in association with root canal-treated teeth means that apical periodontitis (disease) is present. This is often referred to as post-treatment apical periodontitis, which can be categorised as emergent (if developed after treatment), persistent (if persisted despite treatment), or recurrent (if developed after having healed).1 These are the same diseases as the primary apical periodontitis associated with untreated canals; the difference is the root canal conditions.
Post-treatment apical periodontitis is usually observed after endodontic treatments that have not followed acceptable standards for prevention and control of the root canal infection.2,3,4,5 In these cases it is not difficult to realise the cause of disease: persistent or secondary root canal infection resulting from inadequate treatment. Nevertheless, post-treatment apical periodontitis can also be observed in some teeth that were apparently well treated. Post-treatment disease has been reported to occur in 5-15% of teeth with pre-operative apical periodontitis even when treatment has followed proper standards.2,6,7,8
The cause of post-treatment disease is essentially bacterial infection. This can be a persistent or secondary intraradicular infection, but in some cases it may be an extraradicular infection. Non-microbial factors have also been suggested as a potential cause of post-treatment disease,9 but evidence is relatively weak as it comes from a few case reports.
Teeth with post-treatment apical periodontitis can be managed by either nonsurgical endodontic retreatment or periradicular surgery; both of which have high chances of restoring health of the periradicular tissues and maintaining the tooth functional in the oral cavity. This review article deals with the aetiological factors of post-treatment apical periodontitis and discusses the indications and basics of the procedures for clinical management of this condition.
Causes of post-treatment apical periodontitis
Microbial cause – intraradicular infection
Post-treatment apical periodontitis is certainly a microbiological problem, because infection is present in virtually all cases associated with this condition, even in teeth with apparently adequate root canal treatments. Infection is usually located within the root canal system (intraradicular infection), but in a few cases it may extend to the periradicular tissues (extraradicular infection). Depending on the time bacteria gained entry into the root canal, the intraradicular infection can be persistent or secondary. Persistent infection is caused by bacteria present at the time of the first treatment, which were not successfully eliminated or controlled. Persistent infection is the main cause of persistent post-treatment apical periodontitis.10 Secondary infection is caused by bacteria not present in the canal before treatment but introduced in the canal following a breach in the aseptic conditions during treatment or a failure in the coronal seal after treatment conclusion. Secondary infection is possibly the main cause of emergent and even of recurrent disease, although persistent infections can also contribute to the latter.11
Post-treatment disease has been demonstrated to be highly associated with intraradicular infection by studies using microscopy,12,13,14 culture15,16 or molecular methods.17,18,19 Bacteria resisting the effects of treatment and causing persistent periradicular inflammation are usually located in areas of difficult access to instruments and irrigants, and often in direct contact with a source of nutrients from the periradicular tissues. Areas of bacterial persistence include the very apical part of the root canal, lateral canals, apical ramifications, isthmuses and dentinal tubules.11,12,14,20,21,22 Bacterial biofilms are commonly seen in most of these areas.13
The outcome of treatment has been shown to be negatively affected when bacteria persist in the root canals at the time of filling.23,24 This indicates that residual bacteria can survive in treated canals for many years and induce or sustain periradicular tissue inflammation. Actually, there are strong reasons to believe that persistent rather than secondary infections are the most common cause of post-treatment disease. In other words, contrary to the assumption that coronal leakage (secondary infection) plays a major role in treatment failure, evidence is mounting that post-treatment disease is mostly caused by bacteria that persisted in the root canal system after the initial treatment. This is based on the following findings: a) biopsy specimens of teeth with post-treatment disease usually reveal a bacterial infection located at the apical third of the canal, but not extending along the entire length of the canal walls (which would be suggestive of coronal leakage, that is, secondary infection);14 b) positive cultures of root canal samples taken at the time of filling project a poor outcome – this indicates a persistent infectious problem;24 c) the incidence of post-treatment disease is higher in teeth with pre-operative apical periodontitis than in teeth with no lesion – should secondary infection due to coronal leakage be the most significant cause of post-treatment disease, the failure rates for the treatment of vital and necrotic teeth would be the same – and they are not.2,5,6,8,25
The fact that persistent infections are the major cause of post-treatment apical periodontitis does not preclude secondary infections due to coronal leakage from being responsible for poor outcome in some cases. A good example is emergent disease, like the one developing in teeth that were vital at the time of treatment but developed an apical periodontitis lesion in the period following conclusion of treatment. Because cross-sectional studies indicate that the best outcome is achieved in teeth with adequate root canal fillings associated with adequate coronal restorations,3,4,26 it is advisable to treat the tooth as a continuum, placing a well-adapted permanent coronal restoration as soon as possible after finishing root canal treatment.
Microbial cause – extraradicular infection
Apical periodontitis is basically characterised by an inflammatory response to intraradicular infection and represents an attempt of the host to prevent the spread of the infection to the alveolar bone and other body sites. In most situations, this inflammatory barrier succeeds in confining the infectious process to the canal, but there are certain circumstances in which bacteria may overcome this barrier and establish an infection beyond the boundaries of the apical foramen. Extraradicular infections are usually associated with acute inflammation, clinically characterised by an abscess with accompanying pain and swelling, or a sinus tract. However, it has been suggested that in some cases an extraradicular infection may be associated with chronic inflammation and lead to endodontic treatment failure. This condition may be associated with a biofilm formation on the external root surface,27 sometimes showing calculus-like calcifications,28 or forming cohesive actinomycotic colonies within the body of the lesion.9,29
The extraradicular infectious process can be dependent on or independent of the intraradicular infection.30 The dependent infection is the one maintained by constant proliferation and invasion of the periradicular tissues by bacteria present in the intraradicular infection. This represents a continuum of intraradicular and extraradicular infection in which the latter component is constantly challenged and combated by host defences and cannot sustain itself without the intraradicular component. Independent extraradicular infections are those that are no longer fostered by an intraradicular infection and as such may not respond to adequate root canal treatment. So far, there is no clear evidence that an extraradicular infection can exist as a self-sustained process independent of the intraradicular infection.21 In a histologic study, Ricucci et al.14 evaluated several treated teeth with post-treatment apical periodontitis and could not detect any case of independent extraradicular infection. In the few cases that bacteria were found invading the inflamed periradicular tissues, concomitant intraradicular infection was also observed. While not so common, extraradicular bacteria were more frequent in symptomatic teeth.
Non-microbial cause – fact or myth?
Sophisticated molecular biology techniques have demonstrated that most, if not all, of the root canals of teeth with post-treatment apical periodontitis are associated with intraradicular or extraradicular infections.17,18,31 Morphological studies also confirm that intraradicular infection is the major cause of post-treatment disease.12,14 Nevertheless, there are some few case reports that suggest that some lesions may not heal because of endogenous or exogenous non-microbial factors.9 Endogenous causes purportedly include cholesterol crystals and true cysts, whereas exogenous causes comprise foreign-body reactions to apically extruded filling materials, paper points or food.14,32 In most of these cases it is very difficult to rule out the concomitant presence of infection as the cause of disease. Therefore, the participation of non-microbial factors as the exclusive cause of treatment failure has still to be consistently proven.
Procedural errors and post-treatment disease
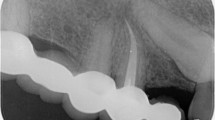
Procedural errors, such as fractured instrument, ledge, perforation, overfilling and so on, are not the direct cause of the post-treatment disease.33,34 In most of the cases infection is also present and is responsible for the persistent or emergent inflammation. The major problem with a procedural accident arising during chemomechanical procedures is when it prevents or makes it difficult for the clinician to properly disinfect the apical part of the root canal. Consequently, the potential for treatment failure in association with a procedural accident relates to the treatment of teeth with infected root canals. For instance, if not manageable, a fractured instrument or a ledge may impede instruments and irrigants from reaching the most apical part of the canal, leaving bacteria in this area unaffected by the disinfection procedures (Fig. 1).
The tooth had been root canal-treated eight years before. A radiolucency is present on the mesial root apex. Retreatment was scheduled; Figs. 1b and c It was not possible to negotiate the mesial canals to their full length because of a ledge; Fig. 1d After a total of 108 days of calcium hydroxide medication (three changes), the canals were filled and the crown restored; Fig. 1e Two years later the patient presented with a flare-up. The radiolucency had remained the same size; Fig. 1f Apicoectomy was scheduled and a cone-beam computed tomography scan was performed to ascertain the relationship of the root apex with the mandibular nerve; Fig. 1g Cross-cut sections of the removed mesial root apex, taken approximately at the level of the line in 1f. An isthmus connecting the two main canals is present (Taylor's modified Brown and Brenn, original magnification × 16), with an enlarged area (1 h) clogged with a thick biofilm (×100); Fig. 1i High power view from the area indicated by the left arrow in (1 h). Condensations of filamentous bacterial forms and accumulation of inflammatory cells (×400); Fig. 1j High power view from the area indicated by the right arrow in (1 h). The lumen is occupied by a thick bacterial biofilm at this level (×400)
There is also a misconception related to failures associated with overfillings. Although in the past the toxicity of the root filling materials had been considered as the cause of persistent inflammation when apically extruded,35 it has been currently accepted that the apical extent of root canal fillings seems to have no correlation with treatment failure, provided infection is absent.24,36 Most of the contemporary materials used for root canal obturation are either biocompatible or show significant cytotoxicity only before setting.37,38 Therefore, the tissue injury caused by extruded sealers is usually only transient. Disease associated with overfilled root canals is generally caused by a concomitant infection in cases where a proper apical seal is missing, favouring nutrient supply to residual bacteria in the canal, or when infected dentinal debris are projected extraradicularly as a result of previous overinstrumentation.1
Management of post-treatment apical periodontitis
Indication: retreatment or surgery
Cross-sectional studies performed in different countries indicate a clear association between teeth with substandard root canal treatment and post-treatment apical periodontitis.3,4,26 Whereas the potential for success reaches 85-95% when the root canal is treated following acceptable standards, poorly-treated teeth exhibit less than 40-50% success. Still lower rates are observed in cases with inadequate coronal restoration. Therefore, a substandard root canal treatment can be regarded as the most predictable risk factor for persistent or emergent apical periodontitis.
Endodontic treatment of teeth with apical periodontitis usually shows a lower success rate than teeth with no lesion at the time of treatment.8,39 This is mostly related to the presence of infection in the root canal system and the difficulties to eliminate or control it. Apical periodontitis lesions usually take six months to two years to heal completely, but some cases can take even longer. It is almost a consensus that if an apical periodontitis lesion has not healed after four years, there is no reason to wait longer for revision of the root canal procedures. Actually, if after one year of follow-up a lesion remains the same size or even expands, or if it emerges in a tooth with no previous apical disease, then management is indicated.40
When facing a case of post-treatment disease, the clinician should consider two main questions: can the tooth be saved? Is it worth saving the tooth? Conditions like advanced periodontal disease, root fracture and unrestorability may contraindicate attempts to save the tooth, while prosthetic planning or the patient´s desire may make tooth saving efforts not worthwhile. Once the decision-making process points to positive answers to these two questions the next step is to decide whether management of post-treatment apical periodontitis will be done by root canal retreatment or periradicular surgery. It has been shown that teeth with inadequate root canal treatment and available coronal access are good candidates for retreatment. Surgery may be the best option in the following circumstances: teeth with well-treated canals where retreatment offers no better prognosis; retreatment is not feasible because coronal access to the apical canal is impossible or with high risk of accidents (extensive restorations, fractured instruments, perforations, ledges, etc); teeth that have already been subjected to retreatment; and cases where there is a need for biopsy.
Technical aspects of endodontic retreatment
The main reasons for failure of primary endodontic treatment are of microbiologic nature; therefore, the success of retreatment procedures will depend upon proper (re)disinfection and reduction of the bacterial load. Nonetheless, retreatment procedures may present several technical challenges.
Case selection, difficulty assessment and pre-treatment evaluation
Retreatment represents a reasonable treatment option if the reason(s) for failure of primary root canal treatment can be identified, which is not possible in all cases.33,40 Retreatment should be considered only for teeth in which technical management seems feasible, periodontal support is sufficient and the tooth can be restored to function. Retreatment may also be indicated as a preventive and pre-emptive treatment in teeth without apical periodontitis or clinical symptoms but with questionable quality of the primary root canal treatment.41
The reason for failure may not be clinically and radiographically discernible in some treated teeth. In these cases, the use of cone beam computed tomography (CBCT) may be of great help to reveal the probable cause of post-treatment disease, including missing or additional canals, poorly prepared/filled canal, root fractures, perforations, and aberrant anatomical variations.42 Thus, CBCT may be indicated as a valuable adjunct diagnostic tool in some retreatment cases. Unfortunately, radiographic and CBCT investigations give no information about disinfection.
Before starting retreatment, the teeth should also be checked for potential treatment challenges and problems that might occur during treatment: inaccessible root canals, additional and previously undetected root canals, blockages, ledges, perforations, fractured instruments, severe curvatures, internal or external resorptions, irremovable root filling material, posts or cores (Fig. 2) and many more.41,43 The radiograph has to be analysed with regard to changes in original root canal anatomy, since severe modifications of original anatomy (for example, straightening, apical transportation, ledging) can present technical problems that cannot be overcome and will compromise the prognosis.44 If any of these problems are anticipated (and communicated to the patient), difficulty, time frame, costs, and chance for success can be calculated more realistically. Nevertheless, it should be considered, and also communicated to the patient, that under certain circumstances the decision may have to be changed, aims and methods of treatment be redefined, and occasionally extraction and implantation selected as the preferable option during any stage of retreatment.
Diagnostic radiograph demonstrating the presence of several challenges and problems that may arise during endodontic retreatment, including unknown core material, unknown amount of remaining sound coronal dentine, perforation, silver cones, undetected and unfilled mesial root canal, ledges, uninstrumented root canal areas, apical blockages, and apical periodontitis lesions
Coronal restoration
Although retention of an existing coronal restoration allows easier placement of rubber dam and does not necessitate a new temporary coverage of the tooth, removal of the restoration offers several important advantages: improved inspection of the pulp chamber; easier access and improved possibilities to detect additional root canals, fractures, dentinal cracks or caries; increased control of tooth margins; and better evaluation of the quantity and integrity of the residual tooth substance (Fig. 3).45 If a restoration cannot or shall not be removed due to several reasons (for example, margins look intact, cost considerations, patient does not agree) the pulp chamber and the margins of the restorations have to be controlled thoroughly for caries and imperfections that might result in bacterial contamination of the root canals.46
Tooth 4.6, restored with a crown, was asymptomatic at the visit. A radiograph showed that the tooth had been root canal-treated, but the apical distal canal was clearly untreated and the mesial canals underinstrumented. The tooth was restored with a well-fitted metal-ceramic crown; Fig. 3c Endodontic retreatment was scheduled. The crown was removed and access to the canals was achieved. Note how the isolation was implemented; Fig. 3d Obturation materials were removed, and new working lengths established; Fig. 3e Appearance of the pulp chamber just before root canal obturation; Fig. 3f The canals were obturated after 48 days of Ca(OH)2 medication with cold gutta-percha laterally compacted and sealer; Fig. 3g Postoperative radiograph; Fig. 3h Two-year follow-up radiograph. Only a minor radiolucency is present on the mesial root; Fig. 3i Radiograph taken after ten years. Normal periradicular conditions
Removal of posts and cores
If the tooth to be retreated is restored with a metal post, the radiograph should be checked for the type of post: cast post or prefabricated post. It should be considered that removal of massive cast posts and cores sometimes is associated with a risk of crack initiation47 and subsequent root fracture. Following reduction in the size of the core, the post can be loosened and removed with ultrasonics.43 In cases of a prefabricated post, screwed or cemented, the core material has to be removed and the pulp chamber be cleaned. With the aid of an appropriate ultrasonic instrument, the majority of posts can be loosened within 15-30 minutes, depending on the length and friction of the post and the intensity of the ultrasonic energy applied.48
Adhesively inserted glass or quartz fibre posts have to be drilled out using burs for post space preparation or modified Gates-Glidden burs with cut off tips (Fig. 4). Great care should be taken to prevent excessive removal of root dentine. In cases with cemented posts, a layer of hard cement should be expected apically to the post, preventing further deeper penetration of instruments in the root canal. This cement layer can be removed using ultrasonic tips in most cases.
The maxillary first premolar had been root canal-treated approximately six years before. A buccal sinus tract was present; Fig. 4b A large mesio-occlusal-distal (MOD) composite restoration was present and a carbon fibre post could be seen at the occlusal surface; Fig. 4c A radiograph revealed an inadequate root canal treatment with the apical canals untreated; there was a post in the palatal canal; Fig. 4d Endodontic retreatment was scheduled. After rubber dam isolation the core material was removed and the post drilled out with burs for post space preparation in the coronal portion, and with ultrasonic diamond tips in the deepest part; Fig. 4e Working length determination. The two canals joined in a common apical canal. After instrumentation the canals were medicated with Ca(OH)2 paste in saline; Fig. 4f The patient returned after one week. The sinus tract had disappeared and the tooth was comfortable; Fig. 4g The canals were obturated
Removal of gutta-percha
Many techniques for removal of gutta-percha have been described in the endodontic literature, including rotary instruments made of stainless steel or nickel-titanium.49 The use of Gates-Glidden burs is usually very effective in removing gutta-percha from the coronal part of the root canal, while the use of stainless-steel hand files or rotary nickel-titanium instruments has been advocated for the middle and apical parts of the canal. Some manufacturers even have developed and marketed special retreatment files. These instruments have an active cutting tip that rapidly and effectively screws into the gutta-percha filling mass. It should be regarded that the use of such instruments bears a high risk of ledging. Rotary removal of gutta-percha using nickel-titanium instruments significantly decreases the time spent to reach the working length and remove the bulk of the filling material, but may also include a certain risk of instrument fracture.
It is important to point out that no technique is able to remove gutta-percha and sealer completely.49,50 Numerous studies have shown that, regardless of the retreatment technique and instruments, residues of the previous filling material remain on the root canal walls.51,52,53 Such residual material has the potential to interfere with disinfection, by physically impeding irrigants and medicaments from reaching bacteria in some areas of the canal system.1
Solvents
Several different solvents have been recommended for softening gutta-percha and facilitation of penetration of the filling material with files. Because chloroform, the most effective solvent, is carcinogenic and no longer recommended,43,49 eucalyptol seems to be the solvent of choice. Dissolved by the solvent, softened gutta-percha can disseminate into the intricacies of the root canal system and make complete removal much more difficult or even impossible. Consequently, the use of solvents should strictly be restricted to cases in which penetration of the gutta-percha seems impossible, and should never be considered in the apical part of the root canal. Softening of gutta-percha can also be achieved by the use of heat, which can be delivered to the root canal via the tip of the unit for thermoplasticised obturation.
Carrier-based filling materials
Carrier-based filling materials, such as Thermafil or Guttacore, can be removed with hand instruments introduced alongside the carrier. Once inserted to a sufficient depth, the instrument (preferably one or two Hedström files) can be used to pull out the carrier.
Additional root canals
It has been shown that in many cases of retreatment, additional root canals can be detected and verified as a possible origin of treatment failure.54 Therefore, in each case the pulp chamber floor has to be searched thoroughly for previously undetected orifices (Fig. 5). Illumination and magnification, both optimally delivered by a dental operating microscope, and dryness of the working field are important prerequisites; in some cases, staining (methylene blue), the 'champagne test' (bubbles appearing from orifices following application of sodium hypochlorite), or transillumination can be used additionally.
The patient declared that the buccal sinus tract never disappeared after the treatment and the tooth was painful. For these reasons the tooth was not restored permanently; Figs. 5c and d Periapical radiographs, taken with different angulations, showed that the canals had been poorly instrumented and obturated, and a large radiolucency was present around the mesio-buccal root apex. Endodontic retreatment was scheduled; Fig. 5e Following isolation with a rubber dam and removal of the temporary restoration and remaining restorative materials, abundant carious tissue appeared on the pulp chamber floor and in the rest of the cavity; Fig. 5f After a first cleaning of the cavity, a fissure appeared connecting the mesiobuccal and the palatal root canal orifices; Fig. 5g Removal of the dentin projections covering this fissure with ultrasonic diamond tips revealed that additional canals were present in the mesial root, which could be negotiated with #10 files. Note the calcification adhered to the pulp chamber floor; Fig. 5h Dentinal septa separating the orifices of these extra canals were carefully eliminated so that there was only one ribbon-shaped canal at the entrance of the mesial root; Fig. 5i In the mesial root the uninstrumented canal (MB2) was found ending considerably short of the radiographic apex; Fig. 5j Removal of the obturation material in the mesio-buccal canal and working length determination; Fig. 5k The canals were obturated after three weeks of Ca(OH)2 medication; during this period the tooth became asymptomatic and the sinus tract had disappeared; Fig. 5l Follow-up radiograph taken after three years and seven months. The radiolucency on the mesial root disappeared completely. The tooth is comfortable
Determination of the working length
The main goal of the endodontic retreatment of failed cases should be to get access to the remaining bacteria that are causing the post-treatment disease. Therefore, the ideal working length should be established apically to the frontline of infection.1 As the most advanced front of infection cannot be determined clinically, it should be advisable to reach the very apical part of the root canal with instruments, irrigants and medicaments; care should be taken to avoid passage of instruments and antimicrobial substances to the periradicular tissues, which might cause unnecessary injury.
In many clinical cases access to the apical foramen is blocked by filling material or dentinal debris, which may be very difficult or even impossible to remove. Nevertheless, an attempt should be made to render the root canal free of debris and filling material and to regain access to the apical foramen. This should be determined both electronically and radiographically. The radiograph will provide the clinician with important information on the presence and nature of curvatures, presence of ledges and other obstacles, as well as additional root canals and remaining filling material. Moreover, if the apical part of the root canal is still blocked by gutta-percha and the apical foramen is not patent no correct electronic measurement should be expected.
Re-preparation
Following removal of the filling material, mechanical preparation of the root canal aims at elimination of residual bacterial biofilms and preparation of a root canal shape that can be adequately obturated. Nevertheless, over-preparation and weakening of the root with the subsequent risk of initiation or perpetuation of dentinal cracks should be avoided.55 The greatest challenge in many cases can be found at the transition between the previously prepared and obturated areas and the unprepared/unobturated apical root canal spaces. Blockages or ledges can be found in this area and occasionally cannot be managed or corrected. There is no evidence as to which size re-preparation should be performed. Good access to infected root canal spaces and complete removal of the previous filling material should be important determinants for the final preparation size.50 To ensure increased canal cleanliness and disinfection as a consequence of maximal elimination of the previous endodontic filling material and incorporation of areas that contain persistent biofilms, the root canal should be enlarged to sizes larger than it was in the previous treatment. Obviously, this should be accomplished without compromising the integrity of the root and predisposing the root to fracture.
Disinfection
It has been shown that teeth with persistent or secondary infections present with a microbiological profile distinct from primary infections.1,56 Species may be more resistant to some medications and/or may be located in areas that are difficult to reach with instruments. Consequently, the disinfection strategy has to take these aspects into consideration. At present, using sodium hypochlorite as the main irrigant (from 0.5% to 5.25% concentration), which has a strong antimicrobial activity and the ability to dissolve organic matter, followed by ethylenediaminetetraacetic acid (EDTA) for removal of the smear layer can be recommended as the basic protocol. Adding a final rinse with 2% chlorhexidine or passive ultrasonic irrigation for activation of sodium hypochlorite seems to be an interesting strategy to improve disinfection.57,58,59 Furthermore, the use of interappointment medication with a calcium hydroxide paste is still recommended to maximise disinfection, especially of areas more distant to the main root canal.59,60,61 Actually, there is an urgent need for development of therapeutic protocols that can predictably treat the infected root canal as a system, reaching the anatomic intricacies where bacteria can spread and remain unaffected by currently available treatment procedures.20 Some technologies have been proposed that may improve root canal disinfection, including laser (photon-induced photoacoustic streaming) activation of irrigants,62 the self-adjusting file system,63,64 and negative pressure systems for delivery of irrigants.65 Although they may be potentially beneficial for retreatment cases or avoiding the need for retreatment, there is a need for clinical studies confirming this potential.
Outcome of retreatment
In teeth with post-treatment disease, the success rate of retreatment as revealed by well-controlled studies ranges from 62% to 84%.2,6,15,66 The approximately 10-20% lower success rate of retreatment as compared with initial treatment is very likely to be related to the following: inability of completely removing the previous obturation or correcting previous errors, which may limit access to residual bacteria; difficulties to reach persistent bacteria located in areas distant from the main root canal; and resistance of persistent bacteria to the antimicrobials used.1
Retreatment of teeth with post-treatment disease that had previous root canal obturation categorised as inadequate presents a significantly better outcome than well-treated teeth.66 This is because these teeth have a greater chance to be properly cleaned, disinfected and filled during retreatment. Adequately treated root canals that fail have also a good chance to fail again after retreatment, because the persistent infection, which is the main cause of failures, is usually located in areas unaffected by instruments, irrigants and possibly the intracanal medication. During retreatment there is a high chance for these bacteria to still remain untouched. Bacteria in extraradicular infections can also be a possible cause of failure and will not be affected by retreatment procedures. Because post-treatment disease in adequately treated teeth may not respond so well to retreatment, periradicular surgery may then arise as a good therapeutic alternative. Studies have reported a high success rate for surgery (87%-92%) when performed using magnification, ultrasonic root-end preparation, and root-end fillings with materials such as mineral trioxide aggregate (MTA), intermediate restorative material (IRM) or Super ethoxy benzoic acid (SuperEBA).67,68
Concluding remarks
In conclusion, like primary apical periodontitis, post-treatment apical periodontitis is a disease caused by intraradicular and sometimes extraradicular infections. Endodontic retreatment of these cases presents several treatment challenges and constitutes a treatment modality of its own, differing in many aspects from primary endodontic treatment. Proper case selection and pre-operative treatment planning are important for a good prognosis of retreatment, which is, however, 10-20% lower than for primary treatment. Periradicular surgery also arises as a viable alternative to retreatment in some cases or as the last attempt to save the tooth and re-establish health.
References
Siqueira J F Jr. Treatment of endodontic infections. London: Quintessence Publishing, 2011.
Sjögren U, Hagglund B, Sundqvist G, Wing K . Factors affecting the long-term results of endodontic treatment. J Endod 1990; 16: 498–504.
Siqueira J F Jr, Rôças I N, Alves F R, Campos L C . Periradicular status related to the quality of coronal restorations and root canal fillings in a Brazilian population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100: 369–374.
Tronstad L, Asbjornsen K, Doving L, Paedersen I, Eriksen H M . Influence of coronal restorations on the periapical health of endodontically treated teeth. Endod Dent Traumatol 2000; 16: 218–221.
Chugal N M, Clive J M, Spångberg L S . Endodontic infection: some biologic and treatment factors associated with outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96: 81–90.
Strindberg L Z . The dependence of the results of pulp therapy on certain factors. Acta Odontol Scand 1956; 14(Suppl 21): 1–175.
Siqueira J F Jr, Rôças I N, Riche F N, Provenzano J C . Clinical outcome of the endodontic treatment of teeth with apical periodontitis using an antimicrobial protocol. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 757–762.
Ricucci D, Russo J, Rutberg M, Burleson J A, Spångberg L S . A prospective cohort study of endodontic treatments of 1.369 root canals: results after 5 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011; 112: 825–842.
Nair P N . Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med 2004; 15: 348–381.
Siqueira J F Jr, Rôças I N . Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod 2008; 34: 1291–1301.
Vieira A R, Siqueira J F Jr, Ricucci D, Lopes W S . Dentinal tubule infection as the cause of recurrent disease and late endodontic treatment failure: a case report. J Endod 2012; 38: 250–254.
Nair P N, Sjögren U, Krey G, Kahnberg K E, Sundqvist G . Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. J Endod 1990; 16: 580–588.
Ricucci D, Siqueira J F Jr. Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod 2010; 36: 1277–1288.
Ricucci D, Siqueira J F Jr., Bate A L, Pitt Ford T R . Histologic investigation of root canal-treated teeth with apical periodontitis: a retrospective study from twenty-four patients. J Endod 2009; 35: 493–502.
Sundqvist G, Figdor D, Persson S, Sjögren U . Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 85: 86–93.
Pinheiro E T, Gomes B P, Ferraz C C, Sousa E L, Teixeira F B, Souza-Filho F J. Microorganisms from canals of root-filled teeth with periapical lesions. Int Endod J 2003; 36: 1–11.
Siqueira J F Jr, Rôças I N . Polymerase chain reaction-based analysis of microorganisms associated with failed endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 97: 85–94.
Rôças I N, Siqueira J F Jr. Characterization of microbiota of root canal-treated teeth with posttreatment disease. J Clin Microbiol 2012; 50: 1721–1724.
Schirrmeister J F, Liebenow A L, Pelz K et al. New bacterial compositions in root-filled teeth with periradicular lesions. J Endod 2009; 35: 169–174.
Ricucci D, Loghin S, Siqueira J F Jr. Exuberant biofilm infection in a lateral canal as the cause of short-term endodontic treatment failure: report of a case. J Endod 2013; 39: 712–718.
Ricucci D, Siqueira J F Jr. Apical actinomycosis as a continuum of intraradicular and extraradicular infection: case report and critical review on its involvement with treatment failure. J Endod 2008; 34: 1124–1129.
Carr G B, Schwartz R S, Schaudinn C, Gorur A, Costerton J W . Ultrastructural examination of failed molar retreatment with secondary apical periodontitis: an examination of endodontic biofilms in an endodontic retreatment failure. J Endod 2009; 35: 1303–1309.
Fabricius L, Dahlén G, Sundqvist G, Happonen R P, Möller A J R . Influence of residual bacteria on periapical tissue healing after chemomechanical treatment and root filling of experimentally infected monkey teeth. Eur J Oral Sci 2006; 114: 278–285.
Sjögren U, Figdor D, Persson S, Sundqvist G . Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J 1997; 30: 297–306.
Østavik D, Qvist V, Stoltze K . A multivariate analysis of the outcome of endodontic treatment. Eur J Oral Sci 2004; 112: 224–230.
Moreno J O, Alves F R, Goncalves L S, Martinez A M, Rocas I N, Siqueira J F Jr. Periradicular status and quality of root canal fillings and coronal restorations in an urban Colombian population. J Endod 2013; 39: 600–604.
Tronstad L, Barnett F, Cervone F . Periapical bacterial plaque in teeth refractory to endodontic treatment. Endod Dent Traumatol 1990; 6: 73–77.
Ricucci D, Martorano M, Bate A L, Pascon E A . Calculus-like deposit on the apical external root surface of teeth with post-treatment apical periodontitis: report of two cases. Int Endod J 2005; 38: 262–271.
Happonen R P . Periapical actinomycosis: a follow-up study of 16 surgically treated cases. Endod Dent Traumatol 1986; 2: 205–209.
Siqueira J F Jr. Periapical actinomycosis and infection with Propionibacterium propionicum. Endodontic Topics 2003; 6: 78–95.
Subramanian K, Mickel A K . Molecular analysis of persistent periradicular lesions and root ends reveals a diverse microbial profile. J Endod 2009; 35: 950–957.
Koppang H S, Koppang R, Solheim T, Aarnes H, Stolen S O . Cellulose fibres from endodontic paper points as an etiological factor in postendodontic periapical granulomas and cysts. J Endod 1989; 15: 369–372.
Siqueira J F Jr. Aetiology of root canal treatment failure: why well-treated teeth can fail. Int Endod J 2001; 34: 1–10.
Lin L M, Rosenberg P A, Lin J . Do procedural errors cause endodontic treatment failure? J Am Dent Assoc 2005; 136: 187–193; quiz 231.
Muruzábal M, Erasquin J, DeVoto F C . A study of periapical overfilling in root canal treatment in the molar of rat. Arch Oral Biol 1966; 11: 373–383.
Lin L M, Skribner J E, Gaengler P . Factors associated with endodontic treatment failures. J Endod 1992; 18: 625–627.
Spångberg L S, Barbosa S V, Lavigne G D . AH 26 releases formaldehyde. J Endod 1993; 19: 596–598.
Ørstavik D, Mjor I A . Histopathology and x-ray microanalysis of the subcutaneous tissue response to endodontic sealers. J Endod 1988; 14: 13–23.
Friedman S . Expected outcomes in the prevention and treatment of apical periodontitis. In Ørstavik D, Pitt Ford T, eds. Essential endodontology. pp 408–469. Oxford: Blackwell Munksgaard Ltd, 2008.
Wu M K, Dummer P M H, Wesselink P R . Consequences of and strategies to deal with residual post-treatment root canal infection. Int Endod J 2006; 39: 343–356.
Friedman S . Considerations and concepts of case selection in the management of post-treatment endodontic disease (treatment failure). Endodontic Topics 2002; 1: 54–78.
Siqueira J F Jr, Rôças I N, Veiga L M, Lopes H P, Machado de Oliveira J C, Alves F R . Outlining the causes of persistent post-treatment pain in endodontics. ENDO 2009; 3: 185–204.
Hülsmann M, Schäfer E . Problems in endodontics: prevention, identification and management. Berlin: Quintessence Publishing, 2007.
Gorni F G, Gagliani M M . The outcome of endodontic retreatment: a 2-yr follow-up. J Endod 2004; 30: 1–4.
Ricucci D, Grosso A . The compromised tooth: conservative treatment or extraction? Endodontic Topics 2006; 13: 108–122.
Rhodes J S . Disassembly techniques to gain access to pulp chambers and root canals during non-surgical root canal re-treatment. Endodontic Topics 2008; 19: 22–32.
Altshul J H, Marshall G, Morgan L A, Baumgartner J C . Comparison of dentinal crack incidence and of post removal time resulting from post removal by ultrasonic or mechanical force. J Endod 1997; 23: 683–686.
Ruddle C J . Nonsurgical retreatment. J Endod 2004; 30: 827–845.
Duncan H F, Chong B S . Removal of root filling materials. Endodontic Topics 2008; 19: 33–57.
Hülsmann M, Drebenstedt S, Holscher C . Shaping and filling root canals during root canal re-treatment. Endodontic Topics 2008; 19: 74–124.
Hassanloo A, Watson P, Finer Y, Friedman S . Retreatment efficacy of the Epiphany soft resin obturation system. Int Endod J 2007; 40: 633–643.
Hülsmann M, Bluhm V . Efficacy, cleaning ability and safety of different rotary NiTi instruments in root canal retreatment. Int Endod J 2004; 37: 468–476.
Alves F R, Vieira M V, Moreno J O, Lopes W S, Neves M A, Siqueira J F Jr. Removal of filling material in the apical root canal by three retreatment approaches. ENDO 2012; 6: 257–262.
Cantatore G, Berutti E, Castellucci A . Missed anatomy: frequency and clinical impact. Endodontic Topics 2006; 15: 3–31.
Shemesh H, Roeleveld A C, Wesselink P R, Wu M K . Damage to root dentin during retreatment procedures. J Endod 2011; 37: 63–66.
Sundqvist G, Figdor D . Life as an endodontic pathogen. Ecological differences between the untreated and root-filled root canals. Endodontic Topics 2003; 6: 3–28.
Zamany A, Safavi K, Spångberg L S . The effect of chlorhexidine as an endodontic disinfectant. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96: 578–581.
Carver K, Nusstein J, Reader A, Beck M . In vivo antibacterial efficacy of ultrasound after hand and rotary instrumentation in human mandibular molars. J Endod 2007; 33: 1038–1043.
Paiva S S, Siqueira J F Jr, Rôças I N et al. Clinical antimicrobial efficacy of NiTi rotary instrumentation with NaOCl irrigation, final rinse with chlorhexidine and interappointment medication: a molecular study. Int Endod J 2013; 46: 225–233.
Vera J, Siqueira J F J., Ricucci D et al. One-versus two-visit endodontic treatment of teeth with apical periodontitis: a histobacteriologic study. J Endod 2012; 38: 1040–1052.
Shuping G B, Ørstavik D, Sigurdsson A, Trope M . Reduction of intracanal bacteria using nickel-titanium rotary instrumentation and various medications. J Endod 2000; 26: 751–755.
Ordinola-Zapata R, Bramante C M, Aprecio R M, Handysides R, Jaramillo D E . Biofilm removal by 6% sodium hypochlorite activated by different irrigation techniques. Int Endod J 2013.
Neves M A, Rôças I N, Siqueira J F Jr. Clinical antibacterial effectiveness of the self-adjusting file system. Int Endod J 2013.
Siqueira J F Jr, Alves F R, Almeida B M, Machado de Oliveira J C, Rôças I N . Ability of chemomechanical preparation with either rotary instruments or self-adjusting file to disinfect oval-shaped root canals. J Endod 2010; 36: 1860–1865.
Miller T A, Baumgartner J C . Comparison of the antimicrobial efficacy of irrigation using the EndoVac to endodontic needle delivery. J Endod 2010; 36: 509–511.
Farzaneh M, Abitbol S, Friedman S . Treatment outcome in endodontics: the Toronto study. Phases I and II: Orthograde retreatment. J Endod 2004; 30: 627–633.
Rubinstein R A, Kim S . Long-term follow-up of cases considered healed one year after apical microsurgery. J Endod 2002; 28: 378–383.
Chong B S, Pitt Ford T R, Hudson M B . A prospective clinical study of Mineral Trioxide Aggregate and IRM when used as root-end filling materials in endodontic surgery. Int Endod J 2003; 36: 520–526.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Siqueira, J., Rôças, I., Ricucci, D. et al. Causes and management of post-treatment apical periodontitis. Br Dent J 216, 305–312 (2014). https://doi.org/10.1038/sj.bdj.2014.200
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.200
This article is cited by
-
Conservative endodontic microsurgery to protect critical anatomical structures–selective curettage: a case series
BMC Oral Health (2023)
-
Microcomputed tomographic analysis of the efficiency of two retreatment techniques in removing root canal filling materials from mandibular incisors
Scientific Reports (2023)
-
Dose–response association of smoking with delayed healing of apical periodontitis after endodontic treatment
Evidence-Based Dentistry (2023)
-
In vitro evaluation of the sealing ability of combined use of iRoot BP Plus and iRoot SP for root-end filling
Clinical Oral Investigations (2023)
-
Implications of root, pulp chamber, and canal anatomy on pulpotomy and revitalization procedures
Clinical Oral Investigations (2023)