Key Points
-
Reports a high prevalence of apical periodontitis and poor technical quality root canal treatment (RCT) in an adult sub-population in London.
-
Highlights a statistically significant negative correlation between the technical quality of RCT and the presence of apical periodontitis.
-
Suggests endodontic training, and current NHS policies, may require review to maximise the effectiveness of RCT.
Abstract
Aim To assess the prevalence of apical periodontitis (AP) and the technical quality of root canal treatment in an adult sub-population in London.
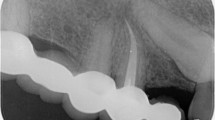
Methodology Panoramic radiographs of 136 patients who attended a dental hospital were collected. The periapical health of teeth present was assessed radiographically and the presence or absence of AP noted. The technical quality of the root canal treatment was scored as adequate or inadequate, based on the European Society of Endodontology (2006) guidelines.
Results A total of 3,396 teeth were assessed; AP was detected in 4.1% of the teeth. Forty-nine percent of patients had at least one tooth with radiographic evidence of AP. The percentage of root filled teeth with AP was 38.3%. AP was significantly more frequently found in root treated, compared with non-root treated, teeth (p <0.001). In 44.3% of the cases, the technical quality of the root canal filling was inadequate. AP was detected in 14% of adequately, compared with 68.6% of inadequately, root filled teeth. There is a significant negative correlation between the technical quality of root canal treatment and the presence of AP (p <0.001).
Conclusions There was a high prevalence of AP and poor technical quality root canal treatment; a strong association between AP and root filled teeth, and between the periapical health and the technical quality of the root canal treatment. The results are consistent with previous studies using similar methodology and re-confirmed that high technical quality root canal treatment is crucial to ensure a favourable treatment outcome.
Similar content being viewed by others
Introduction
Apical periodontitis (AP) is a chronic inflammatory disease that manifests itself as a dynamic host defence response to microbial infection within the root canal system.1 From epidemiological studies AP has been reported to be a widespread disease in the adult population: the percentage of patients having at least one tooth with AP ranges from 27-80%.2,3,4
Following completion of root canal treatment, it is essential to monitor the outcome.5 The presence of AP is usually detected through radiological assessment. The persistence, or the new appearance, of a periapical radiolucency is considered an indication of an unfavourable outcome of root canal treatment; while the re-establishment or the appearance of a normal periodontal ligament space is considered a favourable and desired outcome.5 The data on the quality and outcome of root canal treatment is derived mainly from follow-up studies undertaken in controlled environments, such as university hospitals or specialist clinics. These studies have reported success rates of up to 96% in establishing periapical health following root canal treatment.2,4 A recent prospective study6 has shown favourable outcome rates based on radiographic evidence of periapical health, of 83% for primary, and 80% for secondary, root canal treatment.
Numerous cross-sectional studies (Table 1) from various countries have reported a high prevalence of AP in root filled teeth. All these studies were carried out in university hospitals and involved a retrospective analysis of dental panoramic radiographs. These studies have shown a high percentage of inadequate root canal treatment and a prevalence of AP associated with root filled teeth ranging from 24.1% to 53.5%.7,8 De Moor et al.,9 Loftus et al.10 and Kabak and Abbott3 found that in over half the cases the technical quality of the root fillings was inadequate, at 56.7%, 52.6% and 52.3% respectively. Several studies have shown that the periapical health status is strongly influenced by the technical quality of root canal treatment. In a study by Lupi-Pegurier et al.,11 68.8% of the root fillings were scored as inadequate and 45.3% of these were associated with periapical lesions. Kabak & Abbott3 and Sunay et al.8 have reported similar findings but at higher percentages, 68% and 83.5% respectively.
Other epidemiological studies have used intra-oral radiographs12,13,14 or a combination of panoramic and periapical radiographs.15,16 Saunders et al.12 have shown that 58.1% of root filled teeth in an adult sub-population in Scotland had radiographic evidence of AP. Tsuneishi et al.13 reported a 70% prevalence of AP in an adult Japanese population and 87% of the subjects had root filled teeth.
Some cross-sectional studies17,18 have shown no significant correlation between the technical quality of root canal treatment and the presence of AP. Da Silva et al.18 suggested that other factors, such as the quality of the coronal restoration, should be investigated further. Saunders et al.12 found that 77% of teeth with post-retained crowns had evidence of periapical pathosis. Segura-Egea et al.19 and Siqueira et al.20 assessed the periapical health status in relation to the quality of the coronal restorations and root fillings; it was found that although the coronal restoration had an impact on periapical health, the technical quality of the root filling was the most critical factor influencing treatment outcome.
The comparison between follow-up and epidemiological studies indicates a lower favourable outcome rate of root canal treatment carried out in general dental practice;2,4 this discrepancy may reflect a difference in the technical quality of the root canal treatment. Regardless of the advances in techniques and materials, it would appear that root canal treatment carried out in general dental practice is not producing the desired treatment outcome.
The aims of this study were to assess the periapical health status and the technical quality of root canal treatment in an adult sub-population in London and to compare the results with other studies using similar methodology. As far as we are aware, no data have been published previously on the prevalence of apical periodontitis and the quality of root canal treatment in London. The intention was to provide an indication of the trend and the disease profile of AP in relation to the technical quality of root canal treatment; this may help with the planning of future dental services and the alignment of endodontic training of dental professionals from a local, national and global health perspective.
Materials and methods
Patient selection
Approval for this study was obtained from the Clinical Effectiveness Unit, Barts Health NHS Trust (Registration No. 010/12). Patient confidentiality was strictly respected and no personal information was divulged.
The clinical records and panoramic radiographs of adult patients referred to, and who attended, the Institute of Dentistry, Barts and the London School of Medicine and Dentistry, over a chosen period (11 January - 7 February 2012) were collected. Patients of the orthodontic department and those younger than 16 years old were excluded.
Radiographs and assessors
The dental panoramic radiographs were taken by trained and qualified radiographers, using either a Planmeca Proline XC (Planmeca Oy, Helsinki, Finland) or a Siemens Orthophos CD (Sirona Dental GmbH, Salzburg, Austria) orthopantomograph machine. All films (Agfa Curix HT1.00G Plus, AGFA Healthcare NV, Mortsel, Belgium) were processed in an AGFA Classic E.O.S. machine (Siemens Healthcare, Erlangen, Germany), using AGFA developer and fixer (AGFA Healthcare NV). The panoramic images were evaluated under standardised and optimised conditions, using a light-box (Kenro Ltd, Swindon, UK) and a Brynolf viewer (JS Dental Inc, Ridgefield, Connecticut, USA) in a darkened room.
Assessor calibration
Twenty panoramic radiographs, not included in the study, were assessed in conjunction with a lecturer in dental maxillofacial radiology in order to calibrate the two examiners, both practising endodontists. The examiner variability was determined by calculating Cohen's kappa values for evaluating the periapical health status and the quality of the root filling. The kappa coefficients were: κ = 0.908 for the detection of AP and κ = 0.898 for the categorisation of the quality of the root filling, indicating a high inter-observer agreement. Based on these results it was considered justifiable to use one examiner, except in cases of difficulties with radiographic interpretation, when scoring was carried out in conjunction with the second examiner; where there was disagreement, a consensus was reached between the two examiners. The 20 radiographs were reassessed three months after the original viewing and the scores reconfirmed high inter-examiner agreement.
Assessment of periapical health status and technical quality of root fillings
The criterion adapted from De Moor et al.9 and employed in other studies3,9,11,21 was used to evaluate radiographically the periapical health status and define AP that is, a radiolucency in connection with the apical part of the root, exceeding at least two times the width of the lateral part of the periodontal ligament.
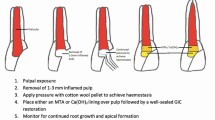
Teeth were classified as root treated if they contained a radiopaque material in the pulp chamber and/or in the root canal.9 The overall technical quality of the root fillings was assessed as either adequate or inadequate based on the European Society of Endodontology guidelines:5
Adequate – the root canal filling should be contained within the tooth, terminating no more than 2 mm from the radiographic apex and without visible voids.
Inadequate – the root canal filling is more than 2 mm short of the radiographic apex, extruded beyond the apical foramen or poorly condensed.
Multi-rooted teeth were categorised according to the root exhibiting the most severe periapical condition; if the tooth was root treated, the quality of the corresponding root filling was assessed. Teeth that were not possible to assess radiographically, due to superimposition of anatomical structures, were excluded from the study.
Statistical analysis
Statistical analysis was performed with the SPSS software (IBM SPSS Statistics 20.0, SPSS Inc, Chicago, IL, USA). Chi-squared tests were used to analyse the relationship between the periapical health status and the presence of the root filling, and the association between AP and the technical quality of the root canal treatment; a p value of <0.05 was considered statistically significant.
Results
The panoramic radiographs of 136 patients, 73 females and 63 males were assessed (Table 2). The periapical health status of 41 teeth, 3 of which were root treated, was not possible to assess due to problems with interpreting the radiographic images and were excluded from the study. As a result, a total number of 3,396 individual teeth were assessed. Just over 49% of all patients, consisting of 43.8% of female and 55.5% of male patients, had at least one tooth with AP (Table 2). AP was detected in 138 (4.1%) of all the teeth assessed; in female patients, 3.0% of teeth had AP, while the percentage rose to 5.3% in male patients (Table 2).
The prevalence of AP according to age groups is shown in Table 3; the 56-65 age group had the highest prevalence (65.2% of patients and 7.7% of teeth), while the 16-25 age group had the lowest (15.8% of patients and 0.7% of teeth).
The frequency of AP and root fillings by tooth type is shown in Table 4. The teeth with the highest frequency of AP were the mandibular first and second molars (11%), followed by the maxillary first and second molars (7.2%). The number of root filled teeth was 115 (3.4% of all teeth observed). The teeth with the highest prevalence of root fillings were the maxillary incisors (6.9%) and the mandibular first and second molars (6.3%).
The total number of root filled and non-root filled with AP was 138 (4.1%); 44 (38.3%) of the root filled teeth had radiographic evidence of AP compared with 94 (2.9%) of non-root filled teeth (Table 5). Chi-squared tests revealed that AP was significantly more frequent in root treated compared with non-root treated teeth (χ2 = 833.106, p <0.001, DF = 1). Among root treated teeth, the highest prevalence of AP was found in mandibular first and second molars (58.3%), followed by maxillary first and second molars (55.6%) and mandibular premolars (53.3%).
The percentage of root fillings scored as inadequate was 44.3% (Table 6). The relationship between the technical quality of root filling and radiographic evidence of AP is shown in Table 7. Inadequately root filled teeth were associated with AP in 68.6% of cases compared with 14% of adequately root filled teeth. Statistical analysis showed a significant negative correlation between the technical quality of root canal treatment and the presence of AP (χ2 = 35.774, p <0.001, DF = 1).
Discussion
The sub-population of patients studied attended the Institute of Dentistry, Barts and the London School of Medicine and Dentistry, which is located in Tower Hamlets, a densely populated borough in inner London. Tower Hamlets is one of the most deprived urban areas in the UK. Due to its location on the fringe of the City of London, the borough has, historically, attracted newer immigrant communities. In the late twentieth century, people from Bangladesh and other Asian and African countries moved into the area, resulting in a richly diverse and multi-cultural population. The patients attending the Institute of Dentistry are almost exclusively referred by National Health Service (NHS) general dental practitioners. The Institute of Dentistry is one of three major referral centres for dentistry in London. Hence, although the sample of patients in this study may not be strictly representative of the entire population of the country, it is not dissimilar to the sub-population of other inner cities and environs in the UK and other major cities of the world where an ethnically and culturally diverse population inhabits. Epidemiology and public health are closely intertwined; therefore, the data collected provide useful information on the prevalence of AP and the quality of root canal treatment, which are relevant to everyday clinical practice in similar sub-populations and from a global health perspective.
In reality, a periapical radiolucency observed on a radiograph is only a static image of a dynamic process; it is not possible to determine whether the lesion is increasing or decreasing in size. However, Petersson et al.22 found that after a 10-year period, the number of root treated teeth with healed periapical lesions was comparable to the number of root treated teeth that developed lesions during the same period; the results indicate the reliability of cross-sectional studies in providing information on the long-term outcome of root canal treatment.
It is not always possible to detect periapical pathosis radiologically; cortical bone involvement may be necessary before radiographic changes are observed.9,23 Furthermore, the present study does not take into consideration teeth in need of root canal treatment without obvious signs of periapical involvement, for example, teeth with irreversible pulpitis. In view of the above, the prevalence of AP and the treatment needs of the sub-population in this study may represent an under-estimation of the real situation. In addition, given the large number of referrals and patients attending, it was necessary to limit the sample size to that of a chosen time period; as it is, 3,396 individual teeth were assessed.
Evaluating the radiographic appearance of the root filling itself may not be sufficient for the purpose of assessing the overall technical quality of the root canal treatment.3 Technical aspects of treatment, such as disinfection, instrumentation and controlled asepsis may influence the outcome of root canal treatment.24 Poor technical quality root fillings may contribute to the introduction or persistence of microorganisms in the root canal system; this may be due to less than stringent adherence to the principles of thorough disinfection, adequate instrumentation and complete obturation of the root canal system.25 However, the visual quality of the root filling is one of the few prognostic factors that can be easily evaluated and recorded.8 Therefore, not unlike other studies (Table 1), the quality of root filling based on visual evaluation was used as an indicator of the overall technical standard of the root canal treatment.
In the present study, data on the prevalence of AP was obtained from panoramic radiographs. Panoramic radiographs are often used in epidemiological studies for convenience and availability.10 With panoramic images, a large volume of data is easily collected without exposing patients to further radiation8 and all teeth in the dentition can be seen on a single radiograph.11 These factors make panoramic radiographs advantageous compared to full-mouth periapical radiographs, which are seldom taken or clinically indicated unless, for example, for comprehensive periodontal assessment. The accuracy of panoramic radiography in the detection of AP, compared with full-mouth periapical radiographs, has been questioned. Ahlqwist et al.26 found a sensitivity of 76% for single-rooted teeth and 90% for multi-rooted teeth, compared with full-mouth radiographic surveys. Muhammed et al.27 concluded that the use of panoramic radiography in the detection of periapical radiolucencies in epidemiological studies was acceptable as the difference between periapical and panoramic radiographs was not statistically significant. This is confirmed by other studies on the specificity for detecting apical radiolucencies on panoramic radiographs.28,29 In addition, modern panoramic radiography machines can produce better images and increase the detection of periapical lesions, even in the anterior region.9
A number of studies10,30,31 have used the 'Periapical index' (PAI) scoring system, as proposed by Ørstavik et al.,32 to assess the periapical health status. PAI is a visual five-point ordinal scale ranging from healthy periapical bone to severe AP with exacerbating features. Usually, AP is recorded as being present for radiolucencies with PAI scores between three and five.30,31 In the study by Loftus et al.,10 only radiolucencies of PAI scores four and five were classified as AP. In this study, for simplicity, all periapical radiolucencies were considered to indicate the presence of AP. Therefore, AP was defined as: a radiolucency in connection with the apical part of the root, exceeding at least two times the width of the lateral part of the periodontal ligament. The above definition should encompass periapical radiolucencies with PAI scores three to five. A new PAI, based on cone beam computed tomography (CBCT), has been proposed.33 Radiolucencies are measured on CBCT scans in three dimensions: bucco-palatal, mesio-distal, as well as diagonal; the CBCT-PAI score is determined by the largest lesion extension. With the CBCT-PAI system, the incidence of false-negatives can be reduced and observer unreliability minimised.33 A high percentage of cases considered as being healthy when assessed using conventional radiography revealed the presence of AP when assessed using CBCT and histology.34 A recent clinical study35 on outcome, one year after completion of root canal treatment, reported a 'healed' rate of 92.7% when assessed using conventional radiography but only 73.9% when CBCT was used. Given conventional radiography underestimates the prevalence of periapical disease, the outcome of root canal treatment should be re-evaluated in long-term longitudinal studies using CBCT and stricter criteria.33 The greater sensitivity and specificity of CBCT will aid the accurate assessment of periapical health status and improve the reliability of prevalence studies on AP. However, CBCT scans are not, currently, routinely used or available for such a large number of patients unlike panoramic radiographs.
In the present study, there was a high inter-observer agreement in categorising the presence of AP and the quality of root fillings. Lupi-Pegurier et al.11 and Loftus et al.10 reported a similarly high inter-observer agreement; the authors stated that this is probably due to the use of strict criteria in the analysis of panoramic radiographs and prior observer calibration, as well the exclusion of poor quality radiographs from the studies. In this study and others quoted in Table 1, some teeth were eliminated because they could not be easily categorised due to difficulties with radiographic interpretation. However, the proportion of non-assessable teeth was lower: 1.2% in the present study, while Kabak and Abbott,3 Lupi-Pegurier et al.11 and Peters et al.7 reported rates of 1.9%, 3.5% and 8% respectively. Similar percentages were reported in studies using intra-oral radiographs. In a study carried out using full mouth periapical radiographs,36 the periapical health status of 3.7% of teeth was impossible to evaluate, due to radiographic faults.
The prevalence of AP in the present study is high; almost half of the patients had at least one tooth with AP, which was detected in 4.1% of all teeth observed. These results are comparable to previous studies using dental panoramic radiographs (Table 1). In the present study, the percentage of root filled teeth with radiographic evidence of AP was 38.3%; studies undertaken in other European countries7,10,11 have reported slightly lower rates, ranging from 24.1-31.5%. In a recent systematic review of cross-sectional studies,37 meta-analysis was performed on 28,881 root filled teeth and revealed the presence of AP in 36% of cases. In the present study, AP was over 13 times more frequent in root filled teeth than in non-root filled teeth, which is statistically significant.
The percentage of inadequate root fillings in this study was 44.3%, consistent with other studies using similar methodology showing poor technical quality of root canal filling (Table 1). The finding of a statistically significant correlation between the quality of root canal treatment and the presence of AP is also consistent with studies quoted previously.3,8,10,11 In this study, AP was associated with inadequately root filled teeth approximately five times more frequently than with adequately root filled teeth.
Since the technical quality influences outcome, root canal treatment should be performed to a high standard. The presence of AP in previously root treated teeth is often associated with poor technical quality treatment, which do not adequately eliminate intra-radicular infection.24 Treatment failures invariably drain valuable and limited financial resources from public health services such as the NHS in the UK. An estimated 415,024 endodontic treatment items, under the Band 2 patient charge (£49) and 206,769 under Band 3 (£214) were provided to adults on the NHS in England in 2012/13.38 Although there are other items of treatment included in Band 2 and 3, this equates to £20,336,176 and £44,248,566 respectively in patient charges. As the root fillings evaluated in this study were almost exclusively carried out in general dental practice and within the NHS, the results of this study would suggest that the technical quality is not conducive and effective in preventing or treating AP. However, outcome studies on root fillings carried out in dental schools or specialist clinics have been reported to be effective in controlling AP.2,4,6 Unfortunately, this is not reflected in cross-sectional studies of the general population, including the present study, reporting high rates of root filled teeth with concomitant AP. Therefore, there is a need to improve the technical quality of root canal treatment as well as a need for root canal re-treatment. Unfortunately, a survey in England of newly qualified dentist in vocational training to join the NHS reported that most expressed a lack of preparedness with regards to complex/molar endodontics with 66% rating their preparedness as 'poor' and 3% as 'very poor'.39 Clearly, high technical quality root canal treatment is not delivered in primary care. Therefore, in view of the findings of this study, the current and limited number of General Dental Council (UK) registered specialists in endodontics is grossly insufficient to manage the increasing demand for complex treatment and re-treatment requirements of the general population in the UK. Consideration should be made to increase access to specialist endodontic services by increasing training opportunities in this speciality in the UK.
There are also financial considerations; in deprived areas, such as the Borough of Tower Hamlets, patients may be unable to afford the cost of private specialist treatment and, hence, arrangements should be made to develop and extend endodontic services funded by the NHS. In a recent independent review of NHS dental services in England40 it was recommended to develop a new contract framework to improve oral care, based on two separate parts: routine care and 'advanced/high-skill' treatments. The review also stated that 'by taking the most demanding types of care out of the routine and continuing part of the contract' it would be possible to 'improve efficiency by directing the care to those who most need it'. Root canal treatment, especially of complex cases, should be part of the advanced services of oral care and should be provided by specialists or general dental practitioners with advanced knowledge and training in endodontics. Under- and post-graduate endodontic training, as well as current treatment policies within the NHS dental services, may need to be reviewed in order to maximise the effectiveness of root canal treatment, thereby reducing the prevalence of AP.
Conclusions
A high prevalence of AP and poor technical quality root canal treatment was found in the sub-population studied. Apical periodontitis was over 13 times more frequent in root filled, compared with non-root filled teeth. There was a statistically significant negative correlation between the technical quality of root canal treatment and the presence of AP. The results of this study are consistent with previous studies using similar methodology. The technical standard of root canal treatment is crucial to achieving a favourable treatment outcome when treating AP.
References
Nair P N . On the causes of persistent apical periodontitis: a review. Int Endod J 2006; 39: 249–281.
Kirkevang L L, Hørsted-Bindslev P . Technical aspects of treatment in relation to treatment outcome. Endodontic Topics 2002; 2: 89–102.
Kabak Y, Abbott P V . Prevalence of apical periodontitis and the quality of endodontic treatment in an adult Belarusian population. Int Endod J 2005; 38: 238–245.
Friedman S . Expected outcomes in the prevention and treatment of apical periodontitis. In Ørstavik D, Pitt Ford T (eds) Essential endodontology. Prevention and treatment of apical periodontitis. 2nd ed. Oxford: Blackwell Munksgaard, 2008.
European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 2006; 39: 921–930.
Ng Y L, Mann V, Gulabivala K . A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J 2011; 44: 583–609.
Peters L B, Lindeboom J A, Elst M E, Wesselink P R . Prevalence of apical periodontitis relative to endodontic treatment in an adult Dutch population: a repeated cross-sectional study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011; 111: 523–528.
Sunay H, Tanalp J, Dikbas I, Bayirli G . Cross-sectional evaluation of the periapical status and quality of root canal treatment in a selected population of urban Turkish adults. Int Endod J 2007; 40: 139–145.
De Moor R J, Hommez G M, De Boever J G, Delmé K L, Martens G E . Periapical health related to the quality of root canal treatment in a Belgian population. Int Endod J 2000; 33: 113–120.
Loftus J J, Keating A P, McCartan B E . Periapical status and quality of endodontic treatment in an adult Irish population. Int Endod J 2005; 38: 81–86.
Lupi-Pegurier L, Bertrand M F, Muller-Bolla M, Rocca J P, Bolla M . Periapical status, prevalence and quality of endodontic treatment in an adult French population. Int Endod J 2002; 35: 690–697.
Saunders W P, Saunders E M, Sadiq J, Cruickshank E . Technical standard of root canal treatment in an adult Scottish sub-population. Br Dent J 1997; 182: 382–386.
Tsuneishi M, Yamamoto T, Yamanaka R et al. Radiographic evaluation of periapical status and prevalence of endodontic treatment in an adult Japanese population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100: 631–635.
Moreno J O, Alves F R, Gonçalves L S, Martinez A M, Rôças I N, Siqueira J F Jr. Periradicular status and quality of root canal fillings and coronal restorations in an urban Colombian population. J Endod 2013; 39: 600–604.
Dugas N N, Lawrence H P, Teplitsky P E, Pharoah M J, Friedman S . Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int Endod J 2003; 36: 181–192.
Gencoglu N, Pekiner F N, Gumru B, Helvacioglu D . Periapical status and quality of root fillings and coronal restorations in an adult Turkish subpopulation. Eur J Dent 2010; 4: 17–22.
Marques M D, Moreira B, Eriksen H M . Prevalence of apical periodontitis and results of endodontic treatment in an adult, Portuguese population. Int Endod J 1998; 31: 161–165.
Da Silva K, Lam J M, Wu N, Duckmanton P . Cross-sectional study of endodontic treatment in an Australian population. Aust Endod J 2009; 35: 140–146.
Segura-Egea J J, Jemenez-Pinzon A, Poyato-Ferrera M, Velasco-Ortega E, Rios-Santos J V . Periapical status and quality of root fillings and coronal restorations in a adult Spanish population. Int Endod J 2004; 37: 525–530.
Siqueira J F Jr, Rôças I N, Alves F R, Campos L C . Periradicular status related to the quality of coronal restorations and root canal fillings in a Brazilian population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100: 369–374.
Gulsahi K, Gulsahi A, Ungor M, Genc Y . Frequency of root-filled teeth and prevalence of apical periodontitis in an adult Turkish population. Int Endod J 2008; 41: 78–85.
Petersson K, Hakansson R, Hakansson J, Olsson B, Wennberg A . Follow-up study of endodontic status in an adult Swedish population. Endod Dent Traumatol 1991; 7: 221–225.
Bender I B . Factors influencing the radiographic appearance of bony lesions. J Endod 1982; 8: 161–170.
Sundqvist G, Figdor D . Endodontic treatment of apical periodontitis. In Ørstavik D, Pitt Ford T (eds) Essential Endodontology. Prevention and treatment of apical periodontitis. Oxford: Blackwell, 1998.
Wu M K, Dummer P M, Wesselink P R . Consequences and strategies to deal with residual post-treatment root canal infection. Int Endod J 2006; 39: 343–356.
Ahlqwist M, Halling A, Hollender L . Rotational panoramic radiography in epidemiological studies of dental health. Swed Dent J 1986; 10: 79–84.
Muhammed A H, Mason-Hing L R, Ala B . A comparison of panoramic and intraoral radiographic surveys in evaluating a dental clinic population. Oral Surg Oral Med Oral Pathol 1982; 54: 108–117.
Molander B, Ahlqwist M, Grondahl H G . Image quality in panoramic radiography. Dentomaxillofac Radiol 1995; 24: 17–22.
Molander B, Ahlqwist M, Grondahl H G . Panoramic and restrictive intraoral radiography in comprehensive oral radiographic diagnosis. Eur J Oral Sci 1995; 103: 191–198.
Kim S . Prevalence of apical periodontitis of root canal-treated teeth and retrospective evaluation of symptom-related prognostic factors in an urban South Korean population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 110: 795–799.
Gumru B, Tarcin B, Pekiner F N, Ozbayrak S . Retrospective radiological assessment of root canal treatment in young permanent dentition in a Turkish subpopulation. Int Endod J 2011; 44: 850–856.
Ørstavik D, Kerekes K, Eriksen H M . The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol 1986; 2: 20–43.
Estrela C, Reis Bueno M, Correa Azevado B, Ribamar Azevado J, Djalma Pécora J . A new periapical index based on cone beam computed tomography. J Endod 2008; 34: 1325–1331.
Wu M K, Shemesh H, Wesselink P R . Limitations of previously published systematic reviews evaluating the outcome of endodontic treatment. Int Endod J 2009; 42: 656–666.
Patel S, Wilson R, Dawood A, Foschi F, Mannocci F . The detection of periapical pathosis using digital periapical radiography and cone beam computed tomography – Part 2: a 1-year post-treatment follow up. Int Endod J 2012; 45: 711–723.
Georgopoulou M K, Spanaki-Voreadi A P, Pantazis N, Kontakiotis E G . Frequency and distribution of root filled teeth and apical periodontitis in a Greek population. Int Endod J 2005; 38: 105–111.
Pak J G, Fayazi S, White S N . Prevalence of periapical radiolucency and root canal treatment: a systematic review of cross-sectional studies. J Endod 2012; 38: 1170–1176.
Health and Social Care Information Centre. Estimated total number of clinical treatment items provided to adults by strategic health authority, 2012/13. London: HSCIC, 2013. Online report available at http://www.hscic.gov.uk/article/2021/Website-Search?productid=12370&q=Prescribing+by+Dentists&sort=Relevance&size=10&page=1 &area=both#top (accessed February 2014).
Patel J, Fox K, Grieveson B, Youngson C C . Undergraduate training as preparation for vocational training in England: a survey of vocational practitioners' and their trainers' views. Br Dent J 2006; 201 (Suppl): 9–15.
Department of Health. NHS dental services in England. An independent review led by Professor Jimmy Steele. London: DH, 2009.
Acknowledgements
The authors would like to thank J. Miller for acting as an assessor and J. Sullivan for the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Di Filippo, G., Sidhu, S. & Chong, B. Apical periodontitis and the technical quality of root canal treatment in an adult sub-population in London. Br Dent J 216, E22 (2014). https://doi.org/10.1038/sj.bdj.2014.404
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.404
This article is cited by
-
Effectiveness of full Pulpotomy compared with Root canal treatment in managing teeth with signs and symptOms indicative of irreversible pulpitis: a protocol for prospectiVE meta-analysis of individual participant data of linked randomised clinical trials (PROVE)
Trials (2023)
-
Implications of root, pulp chamber, and canal anatomy on pulpotomy and revitalization procedures
Clinical Oral Investigations (2023)
-
Prevalence of apical periodontitis in endodontically-treated maxillary and mandibular posterior teeth in a Saudi Arabian population: a cone-beam computed tomography study
Oral Radiology (2023)
-
The objectives and instructional design of undergraduate endodontic program: multicenter cross-sectional study in Saudi Arabia
BMC Medical Education (2022)
-
The effect of different irrigation and disinfection methods on post-operative pain in mandibular molars: a randomised clinical trial
BMC Oral Health (2022)