Abstract
Objectives To compare the effects of nitrous oxide and midazolam on cognition and mood.
Design A three-way, counterbalanced, cross-over study, using patients receiving conscious sedation for routine dental treatment.
Methods On each of three separate visits, patients performed a computerised test battery to determine baseline cognitive performance. Then, following administration of either midazolam, nitrous oxide, or no drug, patients re-performed the test battery. Finally, patients completed visual analogue scales assessing their subjective mood state.
Results Relative to baseline performance, midazolam administration produced significantly slower reaction times compared with nitrous oxide and no-drug conditions. Furthermore, patients receiving midazolam were impaired in accuracy relative to the other conditions on many of the cognitive tasks, particularly those assessing the recall of information. Patient performance in nitrous oxide and control conditions did not significantly differ. These results could not be explained by differences in mood between the conditions, as subjective mood ratings during midazolam or nitrous oxide administration were very similar.
Conclusions It is important for clinicians to be aware that peri-operative recall of information is reduced in patients who have undergone midazolam sedation. This is an advantage for patients who are anxious, and do not wish to be aware of the operative treatment being performed. However, as the cognitive impairment is enduring, an adult escort and written post-operative instructions should be mandatory for midazolam sedation patients. In contrast, the use of nitrous oxide sedation does not significantly impair higher cognitive tasks and thus patients receiving nitrous oxide sedation can resume normal activities in the post-operative period.
Similar content being viewed by others
Main
Benzodiazepines are widely used for conscious sedation in dentistry. One of the most widely used is midazolam, a water-soluble compound, which has a short half-life, powerful amnesic qualities, profound anxiolytic, sedative-hypnotic, muscle-relaxant, anti-convulsant actions, and few secondary side effects.1 There is a general consensus that the benzodiazepines prevent the acquisition of newly learned information, leaving previously acquired knowledge intact and impair performance on psychomotor and vigilance tasks.2 Benzodiazepines exert their effects by increasing GABAA receptor affinity for endogenous GABA, thereby inhibiting the ability of the neuron to conduct impulses. These receptors are densely distributed in regions of the brain thought to be principally involved in learning and memory processing.
The other class of sedative agents used for conscious dental sedation are the inhalation anaesthetics. Nitrous oxide is the most widely used as it is non-toxic, rapidly acting, and produces CNS depression with few adverse side effects. Given by inhalation, an appropriate level of sedation is achieved rapidly, with the effects wearing off quickly.3 Human behavioural studies have indicated that nitrous oxide influences psychomotor function, cognition, learning, memory, and mood.4,5 In clinical groups, it has also been shown that nitrous oxide administration impairs the recall of written instructions given to dental patients.6 However, the effects of this compound appear to be more widespread and diffuse than those of the benzodiazepines, as it may act through a mechanism that does not involve direct binding to receptor sites.7 It might thus be expected that the behavioural and functional effects of nitrous oxide and midazolam would differ.
Many anxious and phobic dental patients wish to be asleep for their dental treatment, or certainly do not wish to be aware of the operative dental procedures being undertaken. Sedative agents not only provide anxiolysis so that treatment can be provided, but also induce amnesia for the operative procedure. This amnesic state is an important property of many sedation agents, and is considered to be a useful therapeutic aim.8,9,10 Dentists practising sedation need to understand the cognitive effects of various sedative agents, as such knowledge will not only influence their own practice, but also the subjective experience of the patient. Previous analyses of sedation agents used for dental procedures have been limited by a lack of availability of objective and sensitive tests that can reliably evaluate cognitive tasks. Studies have typically assessed memory impairment for dental procedures, but have not sought to evaluate specific aspects of cognitive performance.11
The aim of this study was to compare the cognitive and mood profiles resulting from the administration of nitrous oxide and midazolam (at standardised clinical doses) to patients undergoing conscious sedation for routine dental treatment. Cognitive performance was assessed using a computerised test battery which has established validity and reliability, and has been shown to be highly sensitive to sedative drug administration.12
Methods
Patients
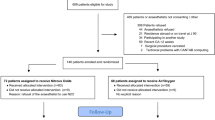
The study was approved by the Joint Ethics Committee of Newcastle and North Tyneside Health Authority, and the University of Northumbria, Division of Psychology Ethics Board. Using a pseudo-randomised order according to a Latin-Squares design, 22 patients were allocated to a treatment-order cell, whereby the cognitive and mood effects of 3.0 mg midazolam, 25% nitrous oxide, and no drug control, were compared. All were out-patients attending the Sedation Department at Newcastle Dental Hospital for restorative dental treatment requiring at least three consecutive visits. They had been referred to the clinic because they were too anxious to receive treatment with local analgesia alone. Prior to each treatment and test session, patients were asked to fast for two hours, and were instructed to refrain from alcohol the previous night. Each individual gave written, witnessed and informed consent to participate.
Procedure
On three separate occasions, each patient performed the computerised test battery under baseline (no drug) conditions, and then following either midazolam, nitrous oxide, or drug-free administration, performed the same battery again. During all conditions, patients were seated in a dental chair in one of two treatment clinics and were tested individually. Following cognitive testing, patients completed an assessment of their current mood state. The whole procedure lasted approximately 40 minutes. On each occasion, after testing was complete, patients then received their planned dental treatment.
Sedation technique
i. Midazolam
There is wide individual variation in sensitivity to midazolam, so much so that dose recommendations for dental sedation are not made on the basis of body weight but are titrated according to clinical response.13 A relatively small clinical dose of 3.0 mg was selected and used as standard throughout. This dose was deemed appropriate to produce the required cognitive effects but without the risk of clinical over-sedation.14 The midazolam (Roche Products Ltd, UK) was administered intravenously using a 5 ml-graduated syringe via a peripheral venous cannula that remained in situ throughout the procedure. The site of the injection was the dorsum of the hand or the antecubital fossa of the arm. Following an initial dose of 1 mg, additional 1 mg increments were administered at 60-second intervals. On receipt of the total dose, a further interval of 5 minutes was allowed prior to cognitive assessment in order to achieve a stable drug state based on the finding that optimal cognitive effects occur between 5–20 minutes after drug administration.14
ii. Nitrous Oxide
A mixture of 25% nitrous oxide in oxygen for inhalation was delivered via a Quantiflex MDM machine (BOC Health Care, USA) through a non-rebreathing circuit fitted with a two-litre reservoir and a close fitting nasal mask. The dose of 25% nitrous oxide was selected as previous studies have suggested a threshold of impairment begins at around 8–12%, and that doses of between 20–30% produce marked and consistent effects on performance.15,16 Again, cognitive assessment did not begin until five minutes of continuous inhalation had passed in order to achieve a stable plateau of approximately 95% concentration in the brain.3 On completion of cognitive assessment, 100% oxygen was administered for two minutes before mask removal to prevent diffusion hypoxia.
iii. No drug control
In the control session, testing did not commence until 5 minutes following the baseline session in order to make this condition comparable to those of the drug conditions.
Cognitive performance
The study used a tailored version of the Cognitive Drug Research (CDR Ltd, Reading, UK) computerised assessment system installed on an Elonex pc386sxm/16 computer. The CDR system includes a number of measures specific to particular aspects of attention (simple reaction time — SRT; choice reaction time — CRT; and digit vigilance — DV); working memory (spatial working memory — SM; immediate word recall — IWR); and long-term memory (picture recognition — PR; word recognition — WR; and delayed word recall — DWR). Full details of these tasks and their administration have been published previously.12,17 Responses are made using a 2-button response box, labelled 'Yes' and 'No', the use of which enables performance to be accurately measured even in sedated patients.
Subjective Mood
Visual Analogue Scales (VAS) assess subjective emotional state and have been found to be effective in measuring change over time in response to drug treatment.18 Their reliability and validity have been well-documented.19 The patient has to rate their feelings on 16 scales by making a perpendicular mark across a horizontal line 100 mm in length, lacking gradation. The line is anchored by two adjectives representing contrasting states of mind and participants are informed that making a mark at the extreme ends of the line would represent the strongest feeling that they had ever experienced of the adjective in question. The ratings are measured in mm, transformed, and weighted according to three factor loadings of 'alertness', 'contentedness', and 'relaxation/calmness'.
Statistical Analysis
Drug-induced performance changes in all variables were derived by subtracting the pre-dose (baseline scores on each study day) from the subsequent post-dose (or control) scores. This method ensures that day-to-day variability is taken into account in the analyses, therefore neither pre- nor post-drug scores are examined separately although it is clear from the pre-drug (baseline) scores that such variability was negligible (Tables 1, 2, 3, 4). The difference scores were examined across conditions using Greenhouse–Geisser corrected repeated-measures (the within-subjects factor being the three drug conditions) analyses of variance (ANOVA). Follow-up comparisons were conducted using Scheffe's conservative method.
Results
Of the 22 patients recruited, 4 withdrew from the study prior to completing all three sessions. Thus the final experimental group comprised 18 patients (13 males, 5 females) aged 17–60 years (mean=33).
Cognitive profiles
As is conventional with such studies using the CDR computerised test battery, the variables tested in this investigation were organised into three main categories:
i. Attention
The analysis demonstrated a significant effect of condition on simple reaction time performance (p=0.015), and the Scheffe post-hoc comparisons revealed that reaction time was significantly slower following midazolam administration. Although simple reaction time in the nitrous oxide session was also slowed relative to the no drug control session, this was non-significant (Table 1, Figure 1a).
Graphs a and b represent measures of attention (data expressed in milliseconds); c and d measures of immediate and long-term verbal memory respectively (data expressed in number of words); e and f mood dimensions (data expressed in millimetres). All graphs depict mean changes from baseline, error bars depict standard errors. *P<0.05; **P<0.01.
For choice reaction time, while there was no significant decline in response accuracy in any of the three sessions, midazolam administration again produced a significant slowing of reaction time relative to the other conditions (p=0.001). Once more, nitrous oxide administration also showed a slowing of response time relative to the no drug control session, but this did not reach significance (Table 1, Figure 1b). To assess effects on the cognitive component of choice reaction time (i.e. decision time), simple reaction time responses were subtracted from choice reaction time responses for each session. Midazolam administration significantly impaired decision time relative to both nitrous oxide and no drug control sessions (p=0.009), whilst performance between nitrous oxide and no drug control sessions did not differ.
Finally, a significant main effect of condition was found for the accuracy of digit vigilance. Patients in the midazolam session exhibited a significant decline from baseline (p=0.007) relative to the other sessions whilst performance between nitrous oxide and no drug control sessions did not differ. Once more, reaction time was severely affected following midazolam administration, performance during this session was significantly slower than during the control session (p=0.026). Reaction times during nitrous oxide and control sessions did not differ (Table 1).
ii. Working memory
The analyses demonstrated a significant main effect of drug on patients' ability to accurately retain spatial information. Midazolam administration produced a significant impairment on the spatial working memory test compared with the nitrous oxide session (p=0.05) and led to a significantly slower response times (p=0.001), (Table 2). However spatial recognition accuracy following midazolam administration remained significantly greater than chance. Immediate word recall performance was severely affected following midazolam administration, as the number of words correctly recalled decreased significantly (p=0.004). Although word recall was also poorer following nitrous oxide administration, this did not differ from that during the control session (Table 2, Figure 1c). Similarly, midazolam administration led to a significant increase in errors (recalling words that had not been presented) compared with the control session, and a significant increase in intrusions (recall of words from previous lists) relative to the nitrous oxide session.
iii. Long-term memory
Delayed word recall performance was significantly affected in the midazolam session (p=0.006) as patients recalled fewer words than in the no drug control session (in fact no correct words were recalled at all following midazolam administration). While administration of nitrous oxide also produced impairment on this task, performance did not differ from that of the no drug control session (Table 3, Figure 1d). On the word recognition task, response times were significantly slower following midazolam administration (p<0.05) and in addition, patients receiving midazolam were significantly impaired in the ability to discriminate between positive and negative items relative to the other sessions (p<0.01). Performance in the nitrous oxide and no drug control sessions did not differ (Table 3). However, (as observed in the spatial working memory measure) recognition following midazolam administration remained significantly above chance (p=0.0002).
Finally, response latencies during picture recognition were significantly slower following midazolam administration (p=0.003) whilst performance in the nitrous oxide and no drug control sessions did not differ. In addition there was a significant main effect of drug on the ability to accurately discriminate between original and new stimuli (p=0.001). Picture recognition performance was impaired following midazolam administration relative to the other conditions; once more nitrous oxide and no drug control sessions did not differ (Table 3). Again however, recognition accuracy following midazolam administration remained above chance (p<0.0001).
Mood
No significant differences were obtained between all sessions on the VAS dimension of 'contentedness' (p>0.05). On the 'alertness' dimension, patients rated themselves as being significantly less alert following midazolam and nitrous oxide administration than during the no-drug control session. Importantly though, alertness ratings following midazolam or nitrous oxide administration did not differ. On the 'calmness' dimension, patients receiving midazolam rated themselves as being significantly calmer than when in the no drug control session (p=0.027) but again midazolam and nitrous oxide sessions did not significantly differ (Table 4, Figure 1e and 1f).
Discussion
As predicted, midazolam administration produced a significant and severe impairment, relative to baseline performance, in all of the cognitive tasks. Nitrous oxide administration produced a rather less severe, and more diffuse/widespread drop in performance, which in general did not differ significantly to that shown during the no-drug control session.
On all measures of attention, patients receiving midazolam displayed markedly slower response times, increased cognitive decision time and digit vigilance accuracy was impaired. These results are in accord with previous findings.20 On both working memory tasks, midazolam administration also produced performance decrements, consistent with the idea that benzodiazepines unequivocally impair acquisition and encoding of new information into episodic memory.20
On the measures of long-term memory, significantly slower response times were again observed, but in addition, delayed word recall was severely impaired. Finally, on word and picture recognition while responses were slowed, and accuracy was significantly impaired during midazolam administration, in both tasks, performance remained above chance. This indicates a dissociation between recall and recognition ability, with recall being markedly more affected than recognition during midazolam administration. This dissociation has been reported in human and animal studies of anterograde amnesia,21 but the issue of whether benzodiazepines differentially affect recall and recognition remains equivocal. This issue requires further clarification.
One issue for consideration concerns the extent to which the severe decrements in cognitive performance during midazolam administration were due simply to its sedative actions.22 Despite the fact that the patients receiving midazolam did rate themselves as being less alert, these ratings did not differ during nitrous oxide inhalation, when impairments were much milder. This indicates that the amnesic properties of midazolam are not due solely to its sedative actions.
While nitrous oxide administration also led to a generalised response slowing, reaction times did not differ significantly to those during control sessions. One study using a similar concentration of nitrous oxide to that reported here, also reported nonsignificant increases in reaction time.23 While other studies have revealed significant increases in reaction time, such effects were dose-dependent, and reaction time slowing may only be seen at the highest doses.17
On the other cognitive measures, nitrous oxide inhalation led to mild performance impairments, which did not differ significantly from performance in the control sessions. These findings are difficult to reconcile with other studies that have reported nitrous oxide inhalation of 15% and above, to produce significant impairments in a wide range of cognitive tasks.24 However, such negligible performance deficits may be due to the reported stimulatory effects of this agent, there having been reports that it can actually stimulate the sympathetic nervous system and may have some characteristics of a CNS stimulant.25 However, this is not always reported;26 it is therefore clear that the cognitive consequences of extended nitrous oxide inhalation require further clarification.
In a clinical sense, it thus appears that midazolam administration produces severe cognitive impairments, not only in the ability to both detect and process information, but also to recall specific aspects of information (ie verbal instructions) over relatively short periods of time. The severe deficit in the recall of episodic material is not mirrored by a comparable deficit in the recognition of similar information. Although impaired relative to baseline, patients receiving midazolam were still able to recognise previously presented verbal and visual information at a level well above chance. In clinical practice midazolam sedation is ideal for those patients who require anxiolysis but who do not wish to be aware of what is happening during their operative treatment. One disadvantage of the amnesic effect of midazolam is that although patients will recall instructions presented before their treatment appointment, they cannot be expected to remember instructions provided during or immediately after sedation. This reinforces the importance of ensuring that dental patients receiving midazolam sedation are accompanied by an adult escort and are not permitted to undertake skilled tasks (eg driving) until all the midazolam has been cleared from the body.9 This also emphasises the need to ensure that post-operative instructions are given both verbally and in writing to the escort, rather than to the patient.
Nitrous oxide administration led to a slowing of responses, but did not produce significant cognitive deficits compared with the control sessions. This finding, in combination with the fact that nitrous oxide is rapidly eliminated from the body following termination of sedation, means that once the patient is fit to be discharged they can, depending on the type of dental treatment provided, resume their normal daily activities. There is no need to restrict their activity during the post-operative period, nor for an escort to accompany them.
This study has provided detailed cognitive profiles of two commonly used sedation agents in a clinical patient population. Previous studies comparing these two drugs have either used less robust tests, or have assessed amnesia for dental procedures and information only.11 The use of such a patient group is of particular importance as previous studies describing drug effects in healthy volunteers may have little relevance to the clinical population who may be prescribed benzodiazepines. In fact, only a small minority of studies have assessed the effects of both benzodiazepines and nitrous oxide on memory in clinical groups.21 This may be of particular importance as subjective reports of cognitive performance correlate poorly with objective laboratory-based test findings, and patients may greatly underestimate drug-induced cognitive deficits.27 The current study has combined laboratory rigour (through the use of the computerised test battery) and ecological validity (through the use of an appropriate clinical population). It is hoped that the cognitive profiles of midazolam and nitrous oxide reported here will be of value to those clinicians who use these sedation techniques on a regular basis.
References
Ghoneim M M, Mewaldt S P . Benzodiazepines and human memory: a review. Anesthesiol 1990; 72: 926–938.
Greenblatt D J . Pharmacology of benzodiazepine hypnotics. J Clin Psychiatry 1992; 53 (suppl.): S7–S13.
Eger E I II . Pharmacokinetics. In: Eger E I. II, (ed.), Nitrous oxide, pp 81–107. London: Edward Arnold, 1985.
Armstrong P J, Morton C, Sinclair W, Tiplady B . Effects of nitrous oxide on psychological performance. A dose-response study using inhalation of concentrations up to 15%. Psychopharmacol 1995; 117: 486–490.
Block R I, Ghoneim M M, Hinrichs J V, Kumar V, Pathak D . Effects of a subanaesthetic concentration of nitrous oxide on memory and subjective experience: influence of assessment procedures and types of stimuli. Human Psychopharmacol 1988; 3: 85–97.
File S E, Balakrishnan, J, Murray A, Harris A, Skelly A M . Effects of nitrous oxide on memory for instructions in dental patients. Human Psychopharmacol 1992; 7: 37–44.
Ueda I, Kamaya H . Molecular mechanisms of anesthesia. Anesth Analg 1984, 63: 929–945.
Ryder W, Wright P A . Dental sedation: a review. Br Dent J 1988; 165: 207–215.
Nadin G, Coulthard P . Memory and midazolam conscious sedation. Br Dent J 1997; 183: 399–407.
Skelly A M, Girdler N M, File S E . The use of temazepam elixir in surgical dental sedation: a comparison with intravenous midazolam. Br Dent J 1992; 172: 153–157.
Easton P, File S F, Skelly A M . Mood change and amnesia for dental procedures following treatment with nitrous oxide or midazolam. Br J Clin Pharmacol 1991; 31: 602–615.
Wesnes K, Simpson P M, Christmas L . The assessment of human information processing abilities in psychopharmacology. In Hindmarch I, Stonier P D (eds). Human psychopharmacology: measures and methods. Vol. 1. Chichester: Wiley: 1987.
Richards A, Griffiths M, Scully C . Wide variation in patient response to midazolam sedation for outpatient oral surgery. Oral Surg Oral Med Oral Pathol 1993: 76; 408–411.
Dundee J W, Wilson D B . Amnesic action of midazolam. Anaesth 1980; 35: 459–461.
Allison R H, Shirley A W, Smith G . Threshold concentration of nitrous oxide affecting psychomotor performance. Br J Anaesth 1979; 51: 177–180.
Fagan D, Paul D L, Tiplady B, Scott D B . A dose-response study of the effects of inhaled nitrous oxide on psychological performance and mood. Psychopharmacol 1994; 16: 333–338.
Hanks G W, O'Neil W M, Simpson P, Wesnes K . The cognitive and psychomotor effects of opioid analgesics II. A randomised controlled trial of single doses of morphine, lorazepam and placebo in healthy subjects. Eur J Clin Pharmacol 1995; 48: 455–460.
Bond A, Lader M . The use of analogue scales in rating subjective feelings. Br J Med Psychol 1974; 47: 211–218.
McCormack H M, Horne D J, Sheather S . Clinical applications of visual analogue scales: a critical review. Psychol Med 1988; 18: 1007–1019.
Curran V . Benzodiazepines, memory and mood: a review. Psychopharmacol 1991; 105: 1–8.
Aggleton J P, Saunders R C . The relationship between temporal lobe and diencephalic structures implicated in anterograde amnesia. Memory 1997; 5: 49–71.
Hommer D W . Benzodiazepines: cognitive and psychomotor effects. In Roy-Byrne P P, Cowley D S, eds. Benzodiazepines in clinical practice: risks and benefits, pp 113–130. Washington DC: American Psychiatric Press, 1991.
Zacny J P, Sparacino G, Hoffmann P M, Martin R, Lichtor J L . The subjective, behavioural and cognitive effects of subanesthetic concentrations of isoflurane and nitrous oxide in healthy volunteers. Psychopharmacol 1994; 114: 409–416.
Tiplady B, Sinclair W A, Morrison L M M . Effects of nitrous oxide on psychological performance. Psychopharmacol Bull 1992; 28: 207–211.
Smith N T, Eger E I II, Stoelting R K . The cardiovascular and sympathetic responses to the addition of nitrous oxide to halothane in man. Anaesth 1970; 32: 410–421.
Dwyer R, Bennett H L, Eger EI II, Heilbron D . Effects of isoflurane and nitrous oxide in subanaesthetic concentrations on memory and responsiveness in volunteers. Anesthesiol 1992; 77: 888–898.
Barbee J G . Memory, benzodiazepines, and anxiety: integration of theoretical and clinical perspectives. J Clin Psychiatry 1993; 54 (Suppl): 86–97.
Acknowledgements
The authors would like to thank all the patients for their participation in this study, the dental sedation nurses at the Dental Hospital Sedation Department for their tolerance and Mrs C. Grieve for excellent patient organisation. We also express our gratitude to Dr G Ayre of CDR Ltd for his advice concerning use of the CDR test battery; and Mr M Hill, Ms K. Wilson and Mr J. Lyne of the Sedation Department for their support. Finally, the authors would like to express their thanks to the anonymous reviewers for their helpful advice concerning amendments to this manuscript.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Thompson, J., Neave, N., Moss, M. et al. Cognitive properties of sedation agents: comparison of the effects of nitrous oxide and midazolam on memory and mood. Br Dent J 187, 557–562 (1999). https://doi.org/10.1038/sj.bdj.4800330
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800330
This article is cited by
-
Effects of Ketamine and Midazolam on Simultaneous EEG/fMRI Data During Working Memory Processes
Brain Topography (2021)
-
Reaction times of children having nitrous oxide inhalation sedation for dental procedures
European Archives of Paediatric Dentistry (2020)
-
A randomised crossover trial of post-operative cognitive and psychomotor recovery from benzodiazepine sedation: effects of reversal with flumazenil over a prolonged recovery period
British Dental Journal (2002)
-
Referrals to a secondary care dental clinic for anxious adult patients: implications for treatment
British Dental Journal (2001)
-
Dose-dependent effects of Flumazenil on cognition, mood, and cardio-respiratory physiology in healthy volunteers
British Dental Journal (2000)