Abstract
In a study of 32 687 subjects with data on physical activity and body mass index (BMI) collected serially over time, we examined associations with pancreatic cancer mortality (n=212). Despite plausible biologic mechanisms, neither physical activity (multivariate relative risks for increasing levels: 1.00, 0.98, 0.92, and 1.31, respectively) nor BMI (corresponding findings: 1.00, 0.84, 1.08, and 0.99, respectively) significantly predicted pancreatic cancer mortality.
Similar content being viewed by others
Main
Pancreatic cancer is a rapidly fatal cancer with 5-year survival of about 4% for all tumours (Ries et al, 2002), and <1% for nonresectable tumours (Bramhall et al, 1995). In the United Kingdom, this cancer does not rank in the top 10 for newly diagnosed cases, yet, it is the sixth most common cancer death (CancerStats, June 2002; September 2002). Owing to the grim prognosis, prevention of pancreatic cancer is important. Unfortunately, there are few established risk factors, the exception being cigarette smoking (IARC, 1986). Experiments using a hamster model have suggested that insulin and insulin resistance may play a role in the aetiology of pancreatic cancer (Schneider et al, 2001). This is supported by human studies, with a meta-analysis of 20 studies concluding that diabetes mellitus is associated with increased risk (Everhart and Wright, 1995). Additionally, a recent study reported that diets rich in foods that raise postprandial glucose levels increase the risk of pancreatic cancer (Michaud et al, 2002).
Physical inactivity and overweight are associated with abnormal glucose metabolism, including insulin resistance, hyperinsulinaemia, impaired glucose tolerance, and type II diabetes (Albu and Pi-Sunyer, 1998; Kelley and Goodpaster, 2001). Owing to these associations, we hypothesised that physical activity and a lean body weight would decrease the risk of pancreatic cancer. Few data are available, providing the motivation for this study.
Materials and methods
Subjects
The College Alumni Health Study is an ongoing study of physical activity and health among men and women in the United States, initiated in 1962. Subjects were recruited from men matriculating at Harvard University as undergraduates between 1916 and 1950, and men and women matriculating at the University of Pennsylvania as undergraduates and graduates between 1928 and 1940. The first health survey was mailed to Harvard University alumni in either 1962 or 1966, and University of Pennsylvania alumni in 1962. We have since obtained updated health information via mailed surveys at periodic intervals.
In 1962 or 1966, 21 582 Harvard men and 14 342 University of Pennsylvania alumni returned their initial health survey. For the present study, we excluded subjects reporting cancer at baseline (n=601), and those with missing information on age or sex (n=74) and physical activity, body weight, or height (n=1645). Of the remaining 33 604 subjects, we successfully followed 32 687 (including 2302 women) for pancreatic cancer mortality; these represent the subjects for this study.
Assessment of physical activity and body weight
Harvard alumni provided information on physical activity and body weight at baseline in 1962 or 1966 and updated this in 1977, 1988, and 1993. University of Pennsylvania alumni provided the same at baseline in 1962, updating this in 1980 and 1993. For physical activity, we asked about daily walking and stair climbing, and sports and recreational activities undertaken in the past week, as well as the frequency and duration of participation (Lee et al, 1992). This assessment of physical activity has been shown to be reliable and valid (Albanes et al, 1990; Washburn et al, 1991; Ainsworth et al, 1993b). For example, the test–retest correlation coefficient over 1 month was 0.72, while estimates of energy expenditure from questionnaires compared with physical activity records yielded a correlation coefficient of 0.65 (Ainsworth et al, 1993b).
Assessment of other characteristics
We also obtained information on cigarette, cigar, and pipe smoking and physician-diagnosed diabetes mellitus at baseline. These data (except cigar and pipe smoking) were updated in 1977, 1988, and 1993 for Harvard alumni, and 1980 and 1993 for University of Pennsylvania alumni. Information on alcohol, coffee, and tea consumption was obtained in 1977 and 1988 for the former subjects, and 1980 for the latter.
Ascertainment of pancreatic cancer mortality
The Alumni Office of both universities maintains records of deceased alumni. Using these records, we obtained copies of death certificates to ascertain the underlying and contributing causes of mortality.
Data analyses
At each assessment, we estimated total energy expenditure from walking, stair climbing, and participation in sports and recreation (Lee and Paffenbarger, 2000). We categorised subjects into approximate fourths according to the baseline distribution: <2100, 2100–4199, 4200–10 499, and ⩾10 500 kJ week−1. For the different components of physical activity, we categorised subjects into approximate fourths of distance walked and stories climbed (both classified as in Table 2), and dichotomised them into not participating or participating in light-, moderate-, and vigorous-intensity activities (Ainsworth et al, 1993a; details provided in Table 2). For body weight, we calculated body mass index (BMI; weight height−2) at each assessment and divided subjects into approximate fourths using the baseline distribution: <22.5, 22.5 – <25, 25 – <27.5, and ⩾27.5 kg m−2.
We used proportional hazards regression with time-dependent covariates (SAS, 1999) to estimate the hazard ratios (relative risks) of pancreatic cancer mortality associated with physical activity and BMI. Initially, we adjusted for age and sex. In age- and sex-adjusted models, cigarette smoking and diabetes mellitus, but not cigar or pipe smoking, alcohol, coffee, or tea intake, significantly predicted mortality from pancreatic cancer. Therefore, to control for these predictors, we additionally included cigarette smoking and diabetes mellitus (classified as in Table 2) in multivariate models. When we examined the association of the each component of physical activity – walking, climbing stairs, and participating in light, moderate, or vigorous activities – with the risk of pancreatic cancer, we further controlled for the other components.
Results
Among the 32 687 subjects, the mean age at baseline was 47. 1 years and 93% were male. During follow-up through 1995, 212 persons died from pancreatic cancer. Table 1 shows the baseline characteristics of subjects according to physical activity level. The more active subjects tended to be younger, male and, as expected, participated more in all the different activity components. Active individuals tended to be less overweight and were more likely to smoke cigars or pipes; however, the proportions smoking cigarettes were similar among the different activity groups. These smoking patterns were observed at a time when the health hazards of smoking were not well known. Active subjects had a lower prevalence of diabetes mellitus and were more likely to consume alcohol, but did not differ from the less active in coffee or tea consumption.
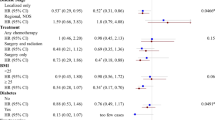
In age- and sex-adjusted analysis, higher levels of energy expenditure did not predict lower risk of pancreatic cancer mortality (P, trend=0.28; Table 2). The most active subjects, expending ⩾10 500 kJ week−1, had a relative risk of 1.27 (95% confidence interval, 0.87–1.84) compared with the least active expending lt;2100 kJ week−1. When we examined the separate components of physical activity (walking, climbing stairs, participation in light, moderate, or vigorous activities), none showed a significant association with pancreatic cancer mortality. Further adjustment for cigarette smoking and diabetes mellitus, as well as participation in the other components, did not materially alter these findings.
For BMI, there was also no significant relation with the risk of pancreatic cancer mortality in age- and sex-adjusted models (P, trend=0.67; Table 2). The heaviest subjects, with BMI⩾27.5 kg m−2, had a relative risk of 1.00 (95% confidence interval, 0.62–1.61) compared with the leanest, with BMI <22.5 kg m−2. Again, further adjustment for cigarette smoking and diabetes mellitus did not change the results.
Finally, we investigated the joint effect of physical activity and BMI on pancreatic cancer risk. We classified subjects into four groups according to whether they met the guidelines for physical activity (Pate et al, 1995) and body weight (WHO, 1995) at baseline: sedentary (<4200 kJ week−1) and overweight (BMI ⩾25 kg m−2), sedentary and normal weight (BMI <25 kg m−2), active (⩾4200 kJ week−1) and overweight, and active and normal weight. The multivariate relative risks of pancreatic cancer were 1.00 (referent), 1.04 (95% confidence interval, 0.81–1.92), 1.25 (0.81–1.92), and 0.97 (0.65–1.46), respectively.
Discussion
This large study of men and women does not support the hypothesis that higher levels of physical activity and leaner body weight decrease the risk of pancreatic cancer. Individuals who satisfied recommendations for physical activity (Pate et al, 1995) and/or a healthy BMI (WHO, 1995) did not experience lower risk of pancreatic cancer than their less active and overweight peers.
Biologically, it appears plausible for physical activity and lean body weight to decrease pancreatic cancer risk. Physical inactivity and overweight are associated with abnormal glucose metabolism, with 90% of type II diabetics in the US being obese (Albu and Pi-Sunyer, 1998). On the other hand, physical activity improves insulin action in overweight and obese individuals, even if body weight and composition are unchanged (Kelley and Goodpaster, 1999). An abnormal insulin and glucose profile is related to increased risk of pancreatic cancer. Hamsters fed a high-fat diet experience peripheral insulin resistance and develop pancreatic cancers when exposed to a pancreatic carcinogen (Schneider et al, 2001). However, if treated with metformin, which improves insulin sensitivity and can lead to lower insulin levels, the incidence of pancreatic cancer is very much reduced. Human pancreatic cancer cells possess insulin receptors, and dose-dependent increases in cell proliferation are observed in response to insulin (Fisher et al, 1996). In humans, higher plasma glucose levels after an oral glucose load is predictive of pancreatic cancer mortality (Gapstur et al, 2000), and a diagnosis of diabetes mellitus is associated with increased risk (Everhart and Wright, 1995).
While the above data suggest that physical activity and body weight may have a role in the aetiology of pancreatic cancer, the findings from epidemiologic studies have been sparse and inconsistent. Three small studies reported no significant association between physical activity and risk (Paffenbarger et al, 1987; Garfinkel and Stellman, 1988; Waterbor et al, 1988), as did a large study with 409 pancreatic cancer deaths (Brownson et al, 1991). In contrast, a prospective study with 350 incident cases observed about a 30–40% reduction in risk among the most active subjects, especially those overweight (Michaud et al, 2001). It is unclear why the present findings differ. Our a priori calculations had estimated reasonable power to detect a 40% reduction in pancreatic cancer risk.
Previous studies of body weight and pancreatic cancer also have yielded inconsistent findings, with case–control studies being more likely to report no association (Howe et al, 1992; Lyon et al, 1993; Coughlin et al, 2000; Michaud et al, 2001). A possible explanation for the discrepancy may be that because of the high mortality from pancreatic cancer, case–control studies are limited by the information obtained from next of kin. However, this study that obtained information on weight prospectively and directly from subjects also did not observe any association with BMI.
Strengths of the present study include its large size and detailed physical activity information. As discussed, the prospective nature of this study limits potential bias from a high fatality rate among pancreatic cancer patients. Limitations include the self-reported information on physical activity and body weight. However, our physical activity assessment is reliable and valid for large population studies (Albanes et al, 1990; Washburn et al, 1991; Ainsworth et al, 1993b). Self-reported body weight also correlates well with measured weights in a well-educated population (Rimm et al, 1990). We were limited in our ability to examine the sexes separately because of the small number of cases in women (n=5). Finally, we ascertained mortality not incidence, but this should not represent a major limitation since, with its high fatality rate, pancreatic cancer mortality would closely reflect incidence.
In conclusion, the data from this large study do not support the biologically plausible hypothesis that physical activity and lean body weight to reduce the risk of pancreatic cancer.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ainsworth BE, Haskell WL, Leon AS, Jacobs Jr DR, Montoye HJ, Sallis JF, Paffenbarger Jr RS (1993a) Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25: 71–80
Ainsworth BE, Leon AS, Richardson MT, Jacobs DR, Paffenbarger Jr RS (1993b) Accuracy of the College Alumnus Physical Activity Questionnaire. J Clin Epidemiol 46: 1403–1411
Albanes D, Conway JM, Taylor PR, Moe PW, Judd J (1990) Validation and comparison of eight physical activity questionnaires. Epidemiology 1: 65–71
Albu J, Pi-Sunyer FX (1998) Obesity and diabetes. In Handbook of Obesity, Bray GA, Bouchard C, James WPT (eds) pp 697–707. New York: Marcel Drekker Inc
Bramhall SR, Allum WH, Jones AG, Allwood A, Cummins C, Neoptolemos JP (1995) Treatment and survival in 13,560 patients with pancreatic cancer, and incidence of the disease, in the West Midlands: an epidemiological study. Br J Surg 82: 111–115
Brownson RC, Chang JC, Davis JR, Smith CA (1991) Physical activity on the job and cancer in Missouri. Am J Public Health 81: 639–642
CancerStats (June 2002) Mortality–UK. United Kingdom: Cancer Research UK
CancerStats (September 2002) Incidence–UK. United Kingdom: Cancer Research UK
Coughlin SS, Calle EE, Patel AV, Thun MJ (2000) Predictors of pancreatic cancer mortality among a large cohort of United States adults. Cancer Causes Control 11: 915–923
Everhart J, Wright D (1995) Diabetes mellitus as a risk factor for pancreatic cancer. A meta-analysis. JAMA 273: 1605–1609
Fisher WE, Boros LG, Schirmer WJ (1996) Insulin promotes pancreatic cancer: evidence for endocrine influence on exocrine pancreatic tumors. J Surg Res 63: 310–313
Gapstur SM, Gann PH, Lowe W, Liu K, Colangelo L, Dyer A (2000) Abnormal glucose metabolism and pancreatic cancer mortality. JAMA 283: 2552–2558
Garfinkel L, Stellman SD (1988) Mortality by relative weight and exercise. Cancer 62: 1844–1850
Howe GR, Ghadirian P, Bueno de Mesquita HB, Zatonski WA, Baghurst PA, Miller AB, Simard A, Baillargeon J, de Waard F, Przewozniak K et al. (1992) A collaborative case–control study of nutrient intake and pancreatic cancer within the search programme. Int J Cancer 51: 365–372
IARC (1986) Vol 38, Tobacco smoking. IARC monographs on the evaluation of the carcinogenic risks of chemicals to humans. Lyon, France: International Agency for Research on Cancer
Kelley DE, Goodpaster BH (1999) Effects of physical activity on insulin action and glucose tolerance in obesity. Med Sci Sports Exerc 31: S619–S623
Kelley DE, Goodpaster BH (2001) Effects of exercise on glucose homeostasis in Type 2 diabetes mellitus. Med Sci Sports Exerc 33: S495–S501; discussion S528-9
Lee IM, Paffenbarger Jr RS (2000) Associations of light, moderate, and vigorous intensity physical activity with longevity. The Harvard Alumni Health Study. Am J Epidemiol 151: 293–299
Lee IM, Paffenbarger Jr RS, Hsieh CC (1992) Time trends in physical activity among college alumni, 1962–1988. Am J Epidemiol 135: 915–925
Lyon JL, Slattery ML, Mahoney AW, Robison LM (1993) Dietary intake as a risk factor for cancer of the exocrine pancreas. Cancer Epidemiol Biomarkers Prev 2: 513–518
Michaud DS, Giovannucci E, Willett WC, Colditz GA, Stampfer MJ, Fuchs CS (2001) Physical activity, obesity, height, and the risk of pancreatic cancer. JAMA 286: 921–929
Michaud DS, Liu S, Giovannucci E, Willett WC, Colditz GA, Fuchs CS (2002) Dietary sugar, glycemic load, and pancreatic cancer risk in a prospective study. J Nat Cancer Inst 94: 1293–1300
Paffenbarger Jr RS, Hyde RT, Wing AL (1987) Physical activity and incidence of cancer in diverse populations: a preliminary report. Am J Clin Nutr 45: 312–317
Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC, Kriska A, Leon AS, Marcus BH, Morris J, Paffenbarger RS Jr, Patrick K, Pollock ML, Rippe JM, Sallis J, Wilmore JH (1995) Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 273: 402–407
Ries LAG, Eisner MP, Kosary CL, Hankey BF, Miller BA, Clegg L, Edwards BK (2002) SEER Cancer Statistics Review, 1973-1999. Bethesda, MD, USA: National Cancer Institute
Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC (1990) Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1: 466–473
SAS(1999) The SAS System, Release 6.12 (TS055). Cary, NC, USA: SAS Institute Inc
Schneider MB, Matsuzaki H, Haorah J, Ulrich A, Standop J, Ding XZ, Adrian TE, Pour PM, (2001) Prevention of pancreatic cancer induction in hamsters by metformin. Gastroenterology 120: 1263–1270
Washburn RA, Smith KW, Goldfield SR, McKinlay JB (1991) Reliability and physiologic correlates of the Harvard Alumni Activity Survey in a general population. J Clin Epidemiol 44: 1319–1326
Waterbor J, Cole P, Delzell E, Andjelkovich D (1988) The mortality experience of major-league baseball players. N Engl J Med 318: 1278–1280
WHO (1995) Physical Status: the Use and Interpretation of Anthropometry.Geneva, Switzerland: World Health Organization
Acknowledgements
This research was supported by grants CA-91213 and HL-67429 from the National Institutes of Health, USA, and a grant from the Robert Wood Johnson Foundation, USA. We are grateful to Sarah E Freeman, Rita W Leung, Doris C Rosoff, and Alvin L Wing for their help with the College Alumni Health Study. This is report No. LXXXII in a series on chronic disease in former college students.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Lee, IM., Sesso, H., Oguma, Y. et al. Physical activity, body weight, and pancreatic cancer mortality. Br J Cancer 88, 679–683 (2003). https://doi.org/10.1038/sj.bjc.6600782
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600782
Keywords
This article is cited by
-
Pancreatic cancer risk in relation to sex, lifestyle factors, and pre-diagnostic anthropometry in the Malmö Diet and Cancer Study
Biology of Sex Differences (2016)
-
Epidemiology of Pancreatic and Periampullary Cancer
Indian Journal of Surgery (2015)
-
Physical activity and risk of pancreatic cancer: a systematic review and meta-analysis
European Journal of Epidemiology (2015)
-
Physical activity and risk of pancreatic cancer in a central European multicenter case–control study
Cancer Causes & Control (2014)
-
Körperliche Bewegung und Sport zur Prävention und Behandlung von Krebskrankheiten
Der Onkologe (2009)