Abstract
Chordomas are radio- and chemo-resistant tumours and metastasise in as many as 40% of patients. The aim of this study was to identify potential molecular targets for the treatment of chordoma. In view of the reported association of chordoma and tuberous sclerosis complex syndrome, and the available therapeutic agents against molecules in the PI3K/AKT/TSC1/TSC2/mTOR pathway, a tissue microarray of 50 chordoma cases was analysed for expression of active molecules involved in this signalling pathway by immunohistochemistry and a selected number by western blot analysis. Chordomas were positive for p-AKT (92%), p-TSC2 (96%), p-mTOR (27%), total mTOR (75%), p-p70S6K (62%), p-RPS6 (22%), p-4E-BP1 (96%) and eIF-4E (98%). Phosphatase and tensin homologue deleted on chromosome 10 expression was lost in 16% of cases. Mutations failed to be identified in PI3KCA and RHEB1 in the 23 cases for which genomic DNA was available. Fluorescence in situ hybridisation analysis for mTOR and RPS6 loci showed that 11 of 33 and 21 of 44 tumours had loss of one copy of the respective genes, results which correlated with the loss of the relevant total proteins. Fluorescence in situ hybridisation analysis for loci containing TSC1 and TSC2 revealed that all cases analysed harboured two copies of the respective genes. On the basis of p-mTOR and or p-p70S6K expression there is evidence indicating that 65% of the chordomas studied may be responsive to mTOR inhibitors, rapamycin or its analogues, and that patients may benefit from combined therapy including drugs that inhibit AKT.
Similar content being viewed by others
Main
Chordoma is a rare malignant locally destructive tumour with a characteristic morphology and immunohistochemical profile (cytokeratin 19 and brachyury positive) that occurs, in the majority of cases, in vertebral bones and presents mostly with a large mass making wide excision rarely possible. Recurrent disease is a common event and metastases occur in as many as 40% of cases (Henderson et al, 2005; Romeo and Hogendoorn, 2006; Vujovic et al, 2006; Tirabosco et al, 2008; Hallor et al, 2008). Surgery, often ablative, is the main treatment option as the tumours are largely resistant to chemotherapy and radiotherapy, although proton/photon-beam radiotherapy is recommended for local control if available (Park et al, 2006) (for review see Casali et al, 2007).
Little is known about the genetic events that account for the development and progression of chordoma although there are reports that this tumour has developed in five patients with tuberous sclerosis complex. This is a tumour suppressor gene-related syndrome occurring on a background of germline mutations in TSC1 and TSC2 (encoding hamartin and tuberin, respectively). One of the cases harbouring a TSC2 mutation had a clear loss of heterozygosity of the wild-type allele. The second case with a TSC1 mutation revealed a reduced signal corresponding to the wild-type allele (allelic imbalance), and this was interpreted as loss of heterozygosity (Lee-Jones et al, 2004). Inactivation of TSC1/TSC2 function results in the phosphorylation of mTOR and its downstream effector molecules, the end result of which is initiation of translation, cell growth and proliferation (for review see Rowinsky (2004); MacKenzie and von Mehren (2007)). Inhibitors to mTOR are available and therefore the possibility exists of directed therapy for chordomas. mTOR exists in two molecular complexes, (mTOR complex mTORC1 and mTORC2), which exhibit different sensitivities to rapamycin and its analogues (Kim et al, 2002; Sarbassov et al, 2004; Yang et al, 2006b). However, investigation into mTOR activity in chordomas is required before offering such treatments as evidence also exists that the locus harbouring mTOR in chordomas is a region where there is frequent genomic loss (frequency of 0.57) (Scheil et al, 2001; Hallor et al, 2008).
The regulation of mTOR is complex, but in summary, AKT, a serine–threonine kinase, can be activated through a number of mechanisms, including the binding of a variety of growth factors to tyrosine kinase receptors, resulting in the phosphorylation of PI3K and PDK1 and subsequent inactivation of TSC1/TSC2 function, through phosphorylation of TSC2 at threonine 1462 by AKT. AKT can also be activated by RAS through PI3K, and through the assembled downstream TORC2 (Downward, 2004; Yang et al, 2006a), and activation of the RAS/MEK/ERK signalling cascade also induces tuberin phosphorylation independently of AKT (Roux et al, 2004). Inactivation of TSC2 releases a negative control on mTOR through the disinhibition of Rheb (RAS homologue enriched in brain), a small GTPase, and brings about phosphorylation of p70S6kinase (p70S6K) and 4E binding protein-1 (4E-BP1), and downstream phosphorylation of S6 ribosomal protein (RPS6) and eukaryotic translation initiation factor 4E (eIF-4E), respectively (Martin and Hall, 2005; Tee et al, 2005). Finally, activation of mTORC1 is also mediated by nutrients and branched amino acids, in particular (Wullschleger et al, 2006).
This study focuses on determining if there is evidence for the activation of PI3K/AKT/TSC1/TSC2/mTOR signalling in chordomas in view of existing therapeutic inhibitors.
Materials and methods
Clinical samples
This study complies with Central Office for Research Ethics Committees standards. The material, snap-frozen and paraffin-embedded tissue, was obtained from the histopathology department of The Royal National Orthopaedic Hospital. The clinical data were retrieved from the clinical notes. The cohort studied consisted of chordomas from 50 patients, 31 males and 19 females, with a median age of 65 years (range 19–84). The tumours were characterised by typical chordoma morphology and the co-expression of a pan-cytokeratin, cytokeratin 19 and brachyury. The sites of the tumours were sacrococygeal (n=41), lumbar (n=6) and cervical (n=3). In a period of follow-up ranging from 6 to 120 months, 46% of patients had one local recurrence, 12% had two and the remainder had no recurrences. Metastases involving bone, skin and lung occurred in 22% of patients. Frozen tumour was available from 23 primary tumours and paraffin embedded from all 50 cases (metastatic disease was not included). Five of the tumours had a dedifferentiated component but this material was only available from two cases and therefore the dedifferentiated component was not studied.
Tissue microarray
The pathology was reviewed by AMF, AS and RT. A tissue microarray (TMA) of all 50 chordomas was constructed using a manual tissue arrayer (Beecher Instruments Inc., Sun Prairie, WI, USA). At least two representative 0.6 mm cores from each case were taken for the array. An additional 120 cores were used as control material and orientation markers and included human salivary gland, kidney, thyroid, tonsil, lymph node, placenta, testis, GIST, thyroid, renal cell and breast carcinomas.
Antibodies and analysis of immunohistochemistry
Details of the antibodies used and conditions for the immunohistochemistry (IHC) are presented in Table 1. The IHC was performed either with the Ventana NexES Autostainer (Ventana Medical Systems, Strasbourg, France), Bond maX Immunostainer (Vision Biosystems, Newcastle upon Tyne, UK) or manually with ventana reagents. Diaminobenzidine was the chromogen in all reactions. Incubation without a primary antibody, as well as incubation with the matching IgG isotype control, under the same conditions for each antibody, served as negative controls.
Each antibody was scored with reference to a positive internal control on the TMA. The scoring system employed was as follows: negative in the absence of immunoreactivity, ‘low’ when the immunoreactivity was unequivocal but less strong than the positive control and ‘high’ when the immunoreactivity was at least as strong as the positive control. The positive cases showed immunoreactivity in more than 95% of the neoplastic cells. Non-neoplastic cells (macrophages, lymphocytes and fibroblasts) in the cores were used as internal negative controls.
Protein isolation and western blot analysis
Ten 10 μm sections were cut from snap-frozen resected specimens. Western blot analysis was carried out according to standard methodology. Briefly, protein extracts (30 μg) were fractionated by SDS-8% polyacrylamide gel electrophoresis (unless otherwise stated) and transferred to a PVDF Immobilion-P transfer membrane (Millipore Corp., Bedford, MA, USA) by standard semi-dry electrotransfer methods. The membrane was blocked with blocking reagents (PBS, 0.1% Tween 20, 5% BSA) for a minimum of 30 min and probed with the appropriate primary antibody overnight at 4°C. Blots were washed in 1 × PBS with 0.1% Tween (PBS-T) and incubated for 1 h at room temperature with the appropriate secondary horseradish peroxidase-conjugated antibody, and enhanced using chemiluminescence detection (Amersham GE Healthcare, Buckinghamshire, UK).
The following antibodies were used for western blotting at a dilution of 1 : 1000 with overnight incubation at 4°C unless otherwise stated: p-AKT (ser 473) (dilution 1 : 250; Cell Signaling Technology, Danvers, MA, USA), total AKT (Cell Signaling Technology), isoform 1 and 2 of p70S6K, which were kindly provided by Professor Ivan Gout (University College London, UK), p-4E-BP1 (Thr 70) (Cell Signaling Technology), p-RPS6 (ser235/236) (Cell Signaling Technology), p-p70S6K (Cell Signaling Technology), S6 Ribosomal protein (clone 54D2; dilution Cell Signaling Technology), mTOR (clone 7C10; Cell Signaling Technology), GAPDH (Mab 6C5, dilution 1 : 5000, incubation 60 min at room temperature; Advanced Immunochemical Inc., Long Beach, CA, USA). Hela cells were used as a positive control when assessing for activation of PI3K/AKT/TSC1/TSC2/mTOR molecules (data not shown).
Nucleic-acid isolation and mutational analysis by direct sequencing
Sampled neoplasms used for nuclei acid extraction comprised between 60 and 80% of tumour. PCR primers for each gene are described in Supplementary Table 1. DNA was extracted using proteinase K (Qiagen, Crawley, UK) from 23 frozen chordomas. Fifty to 100 ng of genomic DNA was amplified by the following touchdown PCR protocol, with annealing temperature reduced by 1°C per cycle from 65° to 56°C followed by 35 further cycles at 56°C as described above. The PCR was performed in a total volume of 50 μl containing 5 μl of 10 × Hotstart buffer I, 0.2 μ M of the dNTP mix, 100 pM of each primer, 1 U of Hotstart DNA polymerase (CLP, San Diego, CA, USA). PCR products were purified using Qiagen purification PCR kit (Qiagen) and DNA sequencing was performed at the Scientific Support Services, UCL. Sequencing reactions were run using GenomeLab DTCS Quick Start chemistry (Beckman Coulter (UK) Ltd Biomedical Research, Bucks, UK) and were analysed on a CEQTM8000 Genetic Analysis System (Beckman Coulter).
RNA was extracted from paraffin-embedded samples using Optimum FFPE RNA Isolation Kit (Ambion Europe, Huntington, Cambridgeshire, UK) and from frozen tissue using TRIzol reagent (Invitrogen Ltd, Paisley, Scotland, UK) followed by purification with RNeasy columns with an additional on-column DNAse I treatment (Qiagen) according to the manufacturer's instructions to avoid genomic DNA contamination. Approximately 150 ng of the total RNA extracted from each sample was reverse transcribed using Superscript III First-Strand Synthesis kit (Invitrogen) according to the manufacturer's instructions and using gene-specific primers for different exons to avoid amplification from gDNA (Supplementary Table 1).
FISH analysis of TSC1, TSC2, mTOR and RPS6
Fluorescence in situ hybridisation (FISH) was performed on TMAs using probes from the RP11 BACs library. RP11-81C14, RP11-304L19, RP11-1107P2 and RP11-624N8 were used for assessing TSC1, TSC2, mTOR and RPS6 allelic loss, respectively (BACPAC Resources Center, Oakland, CA, USA). Centromeric probes, CEP9 and CEP16, were used to assess the presence of two copies of chromosome 9 (RPS6) and 9 and 16 (TSC1 and TSC2, respectively) (Vysis, Abbott Laboratories Inc., Des Plaines, IL, USA), and α-satellite D1Z5 was used for chromosome 1 (mTOR). The probes were prepared with reagents from Vysis. TMA sections were de-paraffinised in xylene and dehydrated in ethanol. Sections were pretreated using the Paraffin Pretreatment Reagent Kit II (Vysis): the slides were placed in the pretreatment solution at 80°C for 50–70 min and in pepsin solution 0.05% at 37°C for 20–25 min. The probe, applied to the slides, were co-denatured for 5 min at 73°C and hybridised for at least 16 h at 37°C in a Thermo-Brite hybridiser (Iris, Westwood, MA, USA). The slides were washed in formamide-free solutions: 2 × SCC/0.3% NP40 (Igepal) at room temperature for 5 min, at 73°C for 2 min and at room temperature for 1 min, and then counterstained with DAPI and analysed under a fluorescent microscope (Olympus, Watford, Hertfordshire, UK) using AnalySIS software (Olympus). The chromosome localisation of all BAC clones was confirmed on normal cells in metaphase. Fifty non-overlapping nuclei that contained unequivocal signals were counted for each case. Hemizygous deletion of RPS6 and mTOR was defined as more than 20% of non-overlapping tumour nuclei containing one RPS6 or mTOR locus red signal and by the presence of two CEP9 and D1Z5 green signals for RPS6 and mTOR, respectively.
Results
Immunohistochemistry results
More than 90% of the chordomas expressed p-AKT (Ser243), p-TSC2 (Thr1462), p-4E-BP1 (Thr70) and eIF-4E as assessed by IHC (Figure 1, Table 2). The labelling pattern of these different antibodies was largely similar and consisted of diffuse granular cytoplasmic immunoreactivity, although nuclear positivity for p-AKT and p-4E-BP1 was also noted in less than 10% of cases (Figure 1). In contrast, phosphorylation of mTOR (Ser2448), p70S6K (Thr389) and RPS6 (Ser235/236) was found in only 13 of 48 (27%), 29 of 46 (62%) and 11 of 49 (22%) cases, respectively (Table 2, Figure 1, and Supplementary Table 2).
Transmitted light photomicrographs of chordoma characterised by cords and clusters of uniform cells with vacuolated cytoplasm set within a myxoid stroma (Ai) and immunoreactive (nuclear) for brachyury (Aii) and cytokeratin 19 (Aiii). The photomicrographs on the left-hand panel represent positive control tissues (breast carcinoma Bi, Ci, Di, Ei, Fi, Gi; colon Hi) that are immunoreactive for the indicated antibodies. The middle panel shows representative chordomas, which were scored as ‘strong’ for expression of the indicated antibody, indicating that the immunoreactivity is as strong as that in the positive control. The right-hand panel includes representative chordomas that were not immunoreactive for the relevant antibody. The bar=50 μm.
Correlation of immunohistochemistry and western blot results
The western blot data on selected cases for p-AKT, p-4E-BP1 and p-p70S6K were in complete concordance with the IHC results (Figure 2). In addition to the phosphorylated status of p70S6K by IHC, all six chordomas analysed by western blot were positive for the rapamycin-sensitive S6K isoform 1, 70 kDa (Figure 2). Western blot analysis for p-mTOR confirmed the IHC data in four of six cases, showing the presence of the activated protein in one case and the absence in three cases.
Validation of the immunohistochemistry results by western blotting for selected targets in the PI3K/AKT/TSC1/TSC2/mTOR pathway on six chordoma (Chdm) cases: (A) western blotting for p-AKT (ser473), total AKT, p-mTOR (ser2448), total mTOR, p-p70S6K (Thr389), isoform 1 of p70S6K, p-RPS6 (ser235/236), total RPS6 and p-4E-BP1 (Thr70). The membranes were stripped and reprobed with anti-GAPDH antibody to assure even loading of proteins in each lane. (B) IHC data for the samples analysed by western blot. Hela cells were used as a positive control when assessing for activation of PI3K/AKT/TSC1/TSC2/mTOR molecules (data not shown).
The p-RPS6 IHC was confirmed in five of the six cases analysed by western blotting: the one discrepant result showed that one immunoreactive case was negative by western blot (Figure 2). Western blot analysis revealed total RPS6 protein in all these six cases although two of these were negative for total protein by IHC. These two cases revealed loss of one RPS6 allele (vide infra), and both were negative for p-RPS6 by western blot, suggesting that the positive result for total RPS6 by western blot may be explained by non-neoplastic stromal cells contaminating the protein lysate.
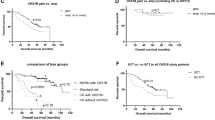
Correlation of mTOR-positive chordomas with other markers
Of the 13 (27%) immunoreactive chordomas for p-mTOR, 12 were immunoreactive for total mTOR protein and showed two copies of the mTOR by FISH, where data were available, and all showed phosphorylation of 4E-BP1 and expressed eIF-4E. Eleven of these 13 p-mTOR-positive cases showed activation of p-p70S6K, and 7 showed activation of p-RPS6. The two cases negative for p-p70S6K activation were also negative for p-RPS6 (Table 2 and Supplementary Table 2).
Correlation of mTOR-negative chordomas with other markers
Thirty-five of 48 chordomas were negative for p-mTOR; 30 of these could be analysed and 21 (70%) were immunoreactive for total mTOR. As mTOR is found in a region reported to be frequently lost in chordomas and other neoplasms, the tumours were analysed for allelic loss by FISH (Figure 3). Of these 21 total mTOR-positive cases, 11 showed two mTOR alleles and 4 revealed loss of one allele (Figure 4A). This left 9 of 30 (30%) p-mTOR-negative cases exhibiting no total mTOR protein as assessed by IHC: five of these cases showed loss of one allele by FISH, two cases showed two copies of the gene and there were no data on two cases.
Photomicrographs of interphase fluorescent in situ hybridisation of chordomas showing an example of allelic loss (right-hand side columns) and the normal two copies (left-hand side columns) for mTOR (top row) and for RPS6 (bottom row). The red signals identify mTOR and RPS6, respectively. The green signals represent chromosome 9 α-satellite probe CEP9 for RPS6, and the D1Z5 α-satellite probe identifies the chromosome 1 centromere for mTOR.
Approximately 50% of the p-mTOR-negative chordomas (16 of 33: 12 of which were immunoreactive for total mTOR) showed activation of neither p70S6K nor RPS6. The remaining 17 p-mTOR-negative chordomas were positive for p-p70S6K, 9 of 15 (60%) of which were immunoreactive for total mTOR, but only one of these cases was positive for RPS6 (Figure 4A).
Correlation of RPS6-negative chordomas with other markers
Thirty-eight of 49 (78%) chordomas were negative for p-RPS6 and 22 of 35 analysable cases (no data for 3 cases of the 38) showed no expression of the total protein RPS6. Fluorescence in situ hybridisation data showed that 18 of the 20 (90%) analysable cases (two had no FISH data available out of the 22) had only one copy of the gene (Figure 4B). In total, 21 cases of 47 (47%) showed loss of one copy by FISH (Supplementary Table 2) (Figure 3).
In view of RPS6 being located in the same chromosomal region as CDKN2A (p16 (INK4)), a common tumour suppressor gene that is lost frequently in chordomas (Hallor et al, 2008), we speculated that the allelic loss of RPS6 correlated with the loss of CDKN2A. This was confirmed by showing that CDKN2A was detected by IHC in only 5 of 48 chordomas (Table 2) and that these 5 cases showed no evidence of allelic loss for RPS6. Furthermore, total RPS6 protein was detected by IHC in four of these (no data for one case, Supplementary Table 2). In contrast, 10 CDKN2A-negative cases showed p-RPS6 positivity and 9 of these showed no RPS6 allelic loss (no data for one case) (Supplementary Table 2).
FISH results for TSC1 and TSC2
Fluorescence in situ hybridisation for TSC1 (28 of 28 cases) and TSC2 (24 of 24 cases) showed two alleles.
Phosphatase and tensin homologue deleted on chromosome 10 in chordoma
Phosphatase and tensin homologue deleted on chromosome 10 (PTEN), a tumour suppressor gene, which when not expressed contributes to constitutive phosphorylation of AKT and activation of the downstream pathways, displayed no immunoreactivity in 16% of chordomas (Figure 1, Table 1). The absence of PTEN by IHC was confirmed by semi-quantitative RT-PCR (data not shown). The absence of PTEN expression did not correlate with the presence of metastatic disease, local recurrence or a dedifferentiated component.
Mutations in RHEB and PI3KCA are not detected in chordomas
Direct sequencing for predicted mutations in RHEB codons 15, 16 and 64, which are similar to K-RAS codons 12, 13 and 61, respectively (Li et al, 2004; Yan et al, 2006), and for common mutations in PI3KCA (exons 4, 5, 7, 9 and 20), failed to reveal mutations (Samuels et al, 2004) (see Supplementary Table 3).
Discussion
mTOR, a protein kinase, is a pivotal regulator of protein synthesis and controls entry into G1 phase of the cell cycle through phosphorylation of the substrates p70S6K and 4E-BP1, molecules that cooperate in translational initiation and ribosomal biogenesis. It is for these reasons that mTOR inhibitors are considered potential therapeutic agents in tumours where mTOR signalling is activated. On the basis of this study of 50 chordomas, we consider that there is evidence that 65% of the tumours are potentially responsive to mTOR antagonists. This figure is generated by the finding that 27% (n=13) of the chordomas exhibit phosphorylated mTOR and a further 18 cases express p-p70S6K although they are negative for p-mTOR.
p-p70S6K is generally used in preference to p-mTOR to assess the tumour response to mTOR antagonists and to predict which tumours may be responsive to such agents (for reviews see Boulay et al (2004); MacKenzie and von Mehren (2007)). Indeed, phosphorylated mTOR has been generally found to be expressed in relatively low numbers of tumours, and several studies make no reference to tumour mTOR expression when assessing the effect of rapamycin and or its analogues (Jaeschke et al, 2002; Gao et al, 2003; Krishnan et al, 2006; El-Salem et al, 2007; Lu et al, 2008; Scheper et al, 2008). Technical difficulties involved in detecting large phosphorylated proteins (mTOR 289 kDa) (Tkaczyk et al, 2002), in addition to the general transient expression of phosphorylated proteins, may contribute to the difficulty in detecting p-mTOR (Riemenschneider et al, 2006). mTOR phosphorylation may also occur on a variety of residues that we have not tested (Cheng et al, 2004).
We consider that the 9 (20%) chordomas that do not express mTOR (total and phosphorylated) protein as assessed by IHC (five of these nine revealed only one mTOR allele (two cases with both alleles, two cases no data)) are unlikely to respond to mTOR inhibitors. Furthermore, we also speculate that the 10 cases that express total mTOR but negative for p-mTOR, p-p70S6K and p-RPS6 would also be at high risk of not responding to mTOR antagonists. On the basis of this calculation, 35% of our chordomas would be unlikely to be responsive to mTOR antagonists.
The complete absence of mTOR expression in nine chordomas raises the question as to how cells survive in the absence of ribosomal biogenesis. One explanation is that the IHC for mTOR is not sufficiently sensitive or that very low levels of mTOR are required for assembling the protein complex (mTORC1). Alternatively, an mTOR-independent pathway, capable of bringing about ribosomal biogenesis and initiation of translation, may be activated. The report that RAS/MEK/ERK pathway activates RPS6 independently of mTOR through p90 ribosomal S6 kinase supports this postulate (Roux et al, 2004).
In view of the importance of ribosomal synthesis in cell growth, the absence of RPS6 protein expression in 58% of chordomas is striking but appears to be a robust result because the IHC data are supported by the finding of RPS6 allelic loss in 21 of the 23 cases. Furthermore, the data correlate with the loss of CDKN2A that lies on chr 9p21.3 and is located adjacent to the cytoband harbouring RPS6 (chr 9p22.1). Hence, the lack of expression of RPS6 protein expression suggests that other p70S6K substrates, such as splicing factor SCAR, translation initiation factor eIF-4B, EF-2B kinase and pro-apoptotic protein Bad1 (Harada et al, 2001; Raught et al, 2004; Richardson et al, 2004), which are less well studied, are likely to undertake this important function (Ruvinsky and Meyuhas, 2006).
It is not clear how loss of RPS6 contributes to the development of neoplasia although its allelic loss has also been reported in chondrosarcomas, a tumour with similarities to chordomas (Rozeman et al, 2006). Interestingly, a causal relationship between RPS6 phosphorylation and protein synthesis has revealed conflicting results. In addition to reports of activation of this protein resulting in elevated cell growth, there is also evidence of increased global protein synthesis in embryonic fibroblasts derived from rpS6−/− mice compared with wild-type cells (Ruvinsky et al, 2005). Furthermore, germline mutations in RPS19, which occur in patients with Blackfan–Diamond syndrome, a cancer susceptibility syndrome associated with haematological malignancies, have already established a role for the loss of RP in cancer. Mutations in this syndrome are directly related to loss of expression of RPs, such as (RP)S19, RPL5 and RPL11 (Draptchinskaia et al, 1999; Cmejla et al, 2009).
One of the reasons for embarking on the analysis of the mTOR pathway in chordomas was the reported loss of heterozygosity in chordomas in two individuals with tuberous sclerosis complex syndrome (Lee-Jones et al, 2004). However, our finding that AKT is activated in over 90% of chordomas argues that the tumour suppressor genes, TSC2 and TSC1, in sporadic chordoma are likely to be ‘inactivated’ not as a result of loss of heterozygosity but rather by phosphorylation of TSC2, at threonine 1462, by p-AKT (Inoki et al, 2002). Indeed, if the tumour suppressor genes were inactivated, the absence of the TSC2 protein would be expected and this was not the case.
The failure to detect RHEB and common PI3K mutations in 23 chordomas provides evidence that these genetic events are unlikely to account for chordoma tumourigenesis in most cases. Furthermore, the published array CGH data showing that neither AKT nor PI3KCA is amplified in 21 cases largely exclude activation of AKT through these genetic events (Hallor et al, 2008). However, these experiments are not exhaustive and additional analyses on greater numbers of genes, in larger tumour series, are warranted.
Functional studies are required to validate our findings, but accessing appropriate control material (notochord), the availability of only one slow-growing chordoma cell line, UCH-1 (Scheil et al, 2001), and the scarcity of animal models prevents this avenue of investigation (although we established xenografts from five different chordomas in nude mice, the tumours disappeared when passaged into a second animal (data not shown)), making this approach difficult. Nevertheless, our findings provide an evidence base for treating selected chordomas with mTOR, AKT inhibitors and antisense molecules to the attractive cancer target, eIF-4E (Graff et al, 2008). A combination of agents, rather than individual drugs, is more likely to offer therapeutic success particularly as there is evidence that AKT is activated at ser473 by TORC2, a rapamycin-insensitive molecule (Sarbassov et al, 2005). The development of a new generation of mTOR-blocking agents (TORKinibs) that interrupt the TORC2 complex is under development and may provide therapeutic benefit over what is currently available (Feldman et al, 2009).
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Boulay A, Zumstein-Mecker S, Stephan C, Beuvink I, Zilbermann F, Haller R, Tobler S, Heusser C, O’Reilly T, Stolz B, Marti A, Thomas G, Lane HA (2004) Antitumor efficacy of intermittent treatment schedules with the rapamycin derivative RAD001 correlates with prolonged inactivation of ribosomal protein S6 kinase 1 in peripheral blood mononuclear cells. Cancer Res 64: 252–261
Casali PG, Stacchiotti S, Sangalli C, Olmi P, Gronchi A (2007) Chordoma. Curr Opin Oncol 19: 367–370
Cheng SW, Fryer LG, Carling D, Shepherd PR (2004) Thr2446 is a novel mammalian target of rapamycin (mTOR) phosphorylation site regulated by nutrient status. J Biol Chem 279: 15719–15722
Cmejla R, Cmejlova J, Handrkova H, Petrak J, Petrtylova K, Mihal V, Stary J, Cerna Z, Jabali Y, Pospisilova D (2009) Identification of mutations in the ribosomal protein L5 (RPL5) and ribosomal protein L11 (RPL11) genes in Czech patients with Diamond–Blackfan anemia. Hum Mutat 30: 321–327
Downward J (2004) PI 3-kinase, Akt and cell survival. Semin Cell Dev Biol 15: 177–182
Draptchinskaia N, Gustavsson P, Andersson B, Pettersson M, Willig TN, Dianzani I, Ball S, Tchernia G, Klar J, Matsson H, Tentler D, Mohandas N, Carlsson B, Dahl N (1999) The gene encoding ribosomal protein S19 is mutated in Diamond–Blackfan anaemia. Nat Genet 21: 169–175
El-Salem M, Raghunath PN, Marzec M, Wlodarski P, Tsai D, Hsi E, Wasik MA (2007) Constitutive activation of mTOR signaling pathway in post-transplant lymphoproliferative disorders. Lab Invest 87: 29–39
Feldman ME, Apsel B, Uotila A, Loewith R, Knight ZA, Ruggero D, Shokat KM (2009) Active-site inhibitors of mTOR target rapamycin-resistant outputs of mTORC1 and mTORC2. PLoS Biol 7: e38
Gao N, Zhang Z, Jiang BH, Shi X (2003) Role of PI3K/AKT/mTOR signaling in the cell cycle progression of human prostate cancer. Biochem Biophys Res Commun 310: 1124–1132
Graff JR, Konicek BW, Carter JH, Marcusson EG (2008) Targeting the eukaryotic translation initiation factor 4E for cancer therapy. Cancer Res 68: 631–634
Hallor KH, Staaf J, Jonsson G, Heidenblad M, Vult von SF, Bauer HC, Ijszenga M, Hogendoorn PC, Mandahl N, Szuhai K, Mertens F (2008) Frequent deletion of the CDKN2A locus in chordoma: analysis of chromosomal imbalances using array comparative genomic hybridisation. Br J Cancer 98: 434–442
Harada H, Andersen JS, Mann M, Terada N, Korsmeyer SJ (2001) p70S6 kinase signals cell survival as well as growth, inactivating the pro-apoptotic molecule BAD. Proc Natl Acad Sci USA 98: 9666–9670
Henderson SR, Guiliano D, Presneau N, McLean S, Frow R, Vujovic S, Anderson J, Sebire N, Whelan J, Athanasou N, Flanagan AM, Boshoff C (2005) A molecular map of mesenchymal tumors. Genome Biol 6: R76
Inoki K, Li Y, Zhu T, Wu J, Guan KL (2002) TSC2 is phosphorylated and inhibited by Akt and suppresses mTOR signalling. Nat Cell Biol 4: 648–657
Jaeschke A, Hartkamp J, Saitoh M, Roworth W, Nobukuni T, Hodges A, Sampson J, Thomas G, Lamb R (2002) Tuberous sclerosis complex tumor suppressor-mediated S6 kinase inhibition by phosphatidylinositide-3-OH kinase is mTOR independent. J Cell Biol 159: 217–224
Kim DH, Sarbassov DD, Ali SM, King JE, Latek RR, Erdjument-Bromage H, Tempst P, Sabatini DM (2002) mTOR interacts with raptor to form a nutrient-sensitive complex that signals to the cell growth machinery. Cell 110: 163–175
Krishnan K, Bruce B, Hewitt S, Thomas D, Khanna C, Helman LJ (2006) Ezrin mediates growth and survival in Ewing's sarcoma through the AKT/mTOR, but not the MAPK, signaling pathway. Clin Exp Metastasis 23: 227–236
Lee-Jones L, Aligianis I, Davies PA, Puga A, Farndon PA, Stemmer-Rachamimov A, Ramesh V, Sampson JR (2004) Sacrococcygeal chordomas in patients with tuberous sclerosis complex show somatic loss of TSC1 or TSC2. Genes Chromosomes Cancer 41: 80–85
Li Y, Inoki K, Guan KL (2004) Biochemical and functional characterizations of small GTPase Rheb and TSC2 GAP activity. Mol Cell Biol 24: 7965–7975
Lu KH, Wu W, Dave B, Slomovitz BM, Burke TW, Munsell MF, Broaddus RR, Walker CL (2008) Loss of tuberous sclerosis complex-2 function and activation of mammalian target of rapamycin signaling in endometrial carcinoma. Clin Cancer Res 14: 2543–2550
MacKenzie AR, von Mehren M (2007) Mechanisms of mammalian target of rapamycin inhibition in sarcoma: present and future. Expert Rev Anticancer Ther 7: 1145–1154
Martin DE, Hall MN (2005) The expanding TOR signaling network. Curr Opin Cell Biol 17: 158–166
Park L, Delaney TF, Liebsch NJ, Hornicek FJ, Goldberg S, Mankin H, Rosenberg AE, Rosenthal DI, Suit HD (2006) Sacral chordomas: impact of high-dose proton/photon-beam radiation therapy combined with or without surgery for primary versus recurrent tumor. Int J Radiat Oncol Biol Phys 65: 1514–1521
Raught B, Peiretti F, Gingras AC, Livingstone M, Shahbazian D, Mayeur GL, Polakiewicz RD, Sonenberg N, Hershey JW (2004) Phosphorylation of eucaryotic translation initiation factor 4B Ser422 is modulated by S6 kinases. EMBO J 23: 1761–1769
Richardson CJ, Broenstrup M, Fingar DC, Julich K, Ballif BA, Gygi S, Blenis J (2004) SKAR is a specific target of S6 kinase 1 in cell growth control. Curr Biol 14: 1540–1549
Riemenschneider MJ, Betensky RA, Pasedag SM, Louis DN (2006) AKT activation in human glioblastomas enhances proliferation via TSC2 and S6 kinase signaling. Cancer Res 66: 5618–5623
Romeo S, Hogendoorn PC (2006) Brachyury and chordoma: the chondroid–chordoid dilemma resolved? J Pathol 209: 143–146
Roux PP, Ballif BA, Anjum R, Gygi SP, Blenis J (2004) Tumor-promoting phorbol esters and activated Ras inactivate the tuberous sclerosis tumor suppressor complex via p90 ribosomal S6 kinase. Proc Natl Acad Sci USA 101: 13489–13494
Rowinsky EK (2004) Targeting the molecular target of rapamycin (mTOR). Curr Opin Oncol 16: 564–575
Rozeman LB, Szuhai K, Schrage YM, Rosenberg C, Tanke HJ, Taminiau AH, Cleton-Jansen AM, Bovee JV, Hogendoorn PC (2006) Array-comparative genomic hybridization of central chondrosarcoma: identification of ribosomal protein S6 and cyclin-dependent kinase 4 as candidate target genes for genomic aberrations. Cancer 107: 380–388
Ruvinsky I, Meyuhas O (2006) Ribosomal protein S6 phosphorylation: from protein synthesis to cell size. Trends Biochem Sci 31: 342–348
Ruvinsky I, Sharon N, Lerer T, Cohen H, Stolovich-Rain M, Nir T, Dor Y, Zisman P, Meyuhas O (2005) Ribosomal protein S6 phosphorylation is a determinant of cell size and glucose homeostasis. Genes Dev 19: 2199–2211
Samuels Y, Wang Z, Bardelli A, Silliman N, Ptak J, Szabo S, Yan H, Gazdar A, Powell SM, Riggins GJ, Willson JK, Markowitz S, Kinzler KW, Vogelstein B, Velculescu VE (2004) High frequency of mutations of the PIK3CA gene in human cancers. Science 304: 554
Sarbassov DD, Ali SM, Kim DH, Guertin DA, Latek RR, Erdjument-Bromage H, Tempst P, Sabatini DM (2004) Rictor, a novel binding partner of mTOR, defines a rapamycin-insensitive and raptor-independent pathway that regulates the cytoskeleton. Curr Biol 14: 1296–1302
Sarbassov DD, Guertin DA, Ali SM, Sabatini DM (2005) Phosphorylation and regulation of Akt/PKB by the rictor–mTOR complex. Science 307: 1098–1101
Scheil S, Bruderlein S, Liehr T, Starke H, Herms J, Schulte M, Moller P (2001) Genome-wide analysis of sixteen chordomas by comparative genomic hybridization and cytogenetics of the first human chordoma cell line, U-CH1. Genes Chromosomes Cancer 32: 203–211
Scheper MA, Chaisuparat R, Nikitakis NG, Sauk JJ (2008) Expression and alterations of the PTEN/AKT/mTOR pathway in ameloblastomas. Oral Dis 14: 561–568
Tee AR, Blenis J, Proud CG (2005) Analysis of mTOR signaling by the small G-proteins, Rheb and RhebL1. FEBS Lett 579: 4763–4768
Tirabosco R, Mangham DC, Rosenberg AE, Vujovic S, Bousdras K, Pizzolitto S, De MG, den Bakker MA, Di FL, Kalil RK, Athanasou NA, O’donnell P, McCarthy EF, Flanagan AM (2008) Brachyury expression in extra-axial skeletal and soft tissue chordomas: a marker that distinguishes chordoma from mixed tumor/myoepithelioma/parachordoma in soft tissue. Am J Surg Pathol 32: 572–580
Tkaczyk C, Metcalfe DD, Gilfillan AM (2002) Determination of protein phosphorylation in Fc epsilon RI-activated human mast cells by immunoblot analysis requires protein extraction under denaturing conditions. J Immunol Methods 268: 239–243
Vujovic S, Henderson S, Presneau N, Odell E, Jacques TS, Tirabosco R, Boshoff C, Flanagan AM (2006) Brachyury, a crucial regulator of notochordal development, is a novel biomarker for chordomas. J Pathol 209: 157–165
Wullschleger S, Loewith R, Hall MN (2006) TOR signaling in growth and metabolism. Cell 124: 471–484
Yan L, Findlay GM, Jones R, Procter J, Cao Y, Lamb RF (2006) Hyperactivation of mammalian target of rapamycin (mTOR) signaling by a gain-of-function mutant of the Rheb GTPase. J Biol Chem 281: 19793–19797
Yang Q, Inoki K, Ikenoue T, Guan KL (2006a) Identification of Sin1 as an essential TORC2 component required for complex formation and kinase activity. Genes Dev 20: 2820–2832
Yang Q, Inoki K, Kim E, Guan KL (2006b) TSC1/TSC2 and Rheb have different effects on TORC1 and TORC2 activity. Proc Natl Acad Sci USA 103: 6811–6816
Acknowledgements
We thank patients for donating their tissue for research and all of the clinicians and support staff in the London Sarcoma Unit who were involved in the care of these patients. The research was generously funded by Skeletal Cancer Action Trust (SCAT), UK and The Rosetrees Trust, UK. The work was also supported by UCLH/UCL Comprehensive Biomedical Research Centre. NP is a research fellow funded by SCAT, AS is a PhD student funded by the Egyptian government and BI is funded by the RNOH NHS Trust. UCL is a partner of the EuroBoNeT consortium, a European Commission granted Network of Excellence for studying the pathology and genetics of bone tumours. We acknowledge Lisa Thompson for her technical assistance for mutation screening.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on British Journal of Cancer website (http://www.nature.com/bjc)
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Presneau, N., Shalaby, A., Idowu, B. et al. Potential therapeutic targets for chordoma: PI3K/AKT/TSC1/TSC2/mTOR pathway. Br J Cancer 100, 1406–1414 (2009). https://doi.org/10.1038/sj.bjc.6605019
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605019
Keywords
This article is cited by
-
Chordoma: demographics and survival analysis with a focus on racial disparities and the role of surgery, a U.S. population-based study
Clinical and Translational Oncology (2023)
-
Impact of silencing eEF2K expression on the malignant properties of chordoma
Molecular Biology Reports (2023)
-
Targeted Therapy for Chordoma: Key Molecular Signaling Pathways and the Role of Multimodal Therapy
Targeted Oncology (2021)
-
Drug combination screening as a translational approach toward an improved drug therapy for chordoma
Cellular Oncology (2021)
-
A novel TSC1 variant associated with tuberous sclerosis and sacrococcygeal teratoma
Human Genome Variation (2020)