Abstract
Background:
Joint effects of mammographic density and other risk factors on breast cancer risk remain unclear.
Methods:
From The Singapore Breast Screening Project, we selected 491 cases and 982 controls. Mammographic density was measured quantitatively. Data analysis was by conditional logistic regression.
Results:
Density was a significant risk factor, adjusting for other factors. Density of 76–100% had an odds ratio of 5.54 (95% CI 2.38–12.90) compared with 0–10%. Density had significant interactions with body mass index and oral contraceptive use (P=0.02).
Conclusions:
Percent density increases breast cancer risk in addition to effects of other risk factors, and modifies the effects of BMI and OCs.
Similar content being viewed by others
Main
Radiologically dense breast tissue is associated with an increased risk of breast cancer (Sala et al, 1998; McCormack and dos Santos Silva, 2006; Boyd et al, 2007). Breast density is also positively correlated with some breast cancer risk factors and negatively correlated with others, notably body mass index (BMI) and age (Boyd et al, 1998; Jakes et al, 2000; Sala et al, 2000). Unresolved issues include the extent to which density contributes to risk independently of other risk factors, how it interacts with other risk factors (that is, whether the effect of density is modified in the presence of other factors), whether absolute dense area or percent density is a better risk predictor and the possible interplay between ethnic origin and density (Maskarinec et al, 2002; Duffy et al, 2004; Chen et al, 2006).
We previously reported on a case-control study of 174 breast cancer cases and 348 controls nested within the Singapore Breast Screening Project (SBSP) using the Tabar qualitative measure of breast density (Jakes et al, 2000; Duffy et al, 2004). The major finding of this study was a significant increase in risk with the Tabar mammographic pattern IV (Jakes et al, 2000). We have now enhanced the same study to include 491 cases and 982 controls, and using a quantitative measure of density, we address the following issues:
-
1)
The association of density with other breast cancer risk factors;
-
2)
The additional effect of density on risk, after adjusting for other risk factors;
-
3)
Interactions between breast density and other risk factors; and
-
4)
Differences between Chinese and other ethnic groups with respect to density and its effect on risk.
Materials and methods
As part of the SBSP, 29 193 Singaporean women aged 45–69 years were screened with a single two-view mammography between 1994 and 1997 (Ng et al, 1998). All subjects completed a questionnaire covering the major breast cancer risk factors (Jakes et al, 2000). Breast cancer cases were notified as either detected through the SBSP or subsequently through record linkage with the Singapore Cancer Registry. This study was approved by the National University of Singapore Institutional Review Board. For each cancer case, we selected two controls, who had not been diagnosed with breast cancer, matched for age, ethnicity and time of screening. The original mammograms from cancer patients and controls were retrieved and density was measured using the Cumulus interactive threshold method (Byng et al, 1998). This estimates both total breast area, total area of dense tissue and percent density, calculated as the quotient of the total area of dense tissue and the total breast area, multiplied by 100. We analysed a total of 491 breast cancer cases (122 diagnosed at screening and 369 subsequently – we were unable to retrieve the mammograms for 10 cases in the previous study) and 982 controls with density measures.
Associations of mammographic density with other breast cancer risk factors among controls only were assessed using the χ2-test. The effects of density breast cancer risk was assessed using conditional logistic regression (Breslow and Day, 1980). Interactions of density with other risk factors in their joint effects on risk were also evaluated using conditional logistic regression.
Results
Table 1 shows the distributions of breast density and other breast cancer risk factors for cases and controls. In univariate conditional logistic regression, significantly increased risks were observed for higher percent density (P<0.001), higher BMI (P=0.03), low parity (P=0.005), early menarche (P=0.003), family history of breast cancer (P<0.001), high socioeconomic status as measured by education (P=0.001), later age at menopause (P=0.008) and ever use of hormone replacement therapy (HRT) (P=0.008). Significantly reduced risks were associated with breast feeding (P=0.006) and early age at first birth (P=0.01). In addition, a significantly increased risk (P=0.001) was observed with higher total dense area and a significantly reduced risk (P=0.002) with higher total breast area (data not shown). Percent breast density had a stronger effect on risk than total dense area or total breast area. We therefore used percent density in subsequent analyses.
After entering the nonmammographic variables into stepwise conditional logistic regression, breast feeding and socioeconomic status were no longer significant. The remaining factors were used for multivariable adjustment of the effect of density. Table 2 shows the odds ratios (OR) associated with density, unadjusted, adjusted only for BMI and adjusted for all significant risk factors. Density had a stronger effect after adjustment for BMI, consistent with the negative confounding effect. Density remained a significant risk factor after adjustment for other risk factors (P<0.001). After multivariable adjustment, the 76–100% density category had an OR of 5.54 (95% CI 2.38–12.90) compared with 0–10%.
We estimated the effect of percent density on risk of cancers by time since screen (detailed results available from the authors). The trend remained highly significant 6 or more years after the mammogram, although its magnitude showed a tendency to decrease with time.
We also tabulated percent density against various breast cancer risk factors within the controls (data available from the authors). Density was significantly increased in association with low BMI (P<0.001), nulliparity and low parity (P<0.001), no history of breast feeding (P<0.001), HRT use (P=0.001), premenopausal status (P<0.001), later age at first birth (P=0.02), younger age (P<0.001) and being Chinese (P<0.001). After adjusting for the well-established confounders age, BMI and ethnicity, all associations remained significant or borderline significant except for age at first birth.
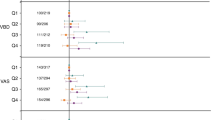
Table 3 shows the results of the interaction analyses. Significant interactions with percent density were observed for BMI and oral contraceptive (OC) use (P=0.02 in both cases). The increasing risk with density was stronger in those with high BMI (that is, in those with high density despite high BMI), and in those with a history of OC use. Numbers of cases and controls in individual categories are available from the authors.
Discussion
Our main findings in this Asian population are that percent breast density, as measured by the Cumulus interactive threshold, is strongly associated with risk of breast cancer. Also, percent density was a stronger associate of risk than absolute dense area, remaining substantial and significant after adjustment for other risk factors. The adjusted odds of breast cancer for those with more than 75% density was around five times that of those with density 10% or less.
We found that percent density was a stronger predictor of risk than absolute density, in agreement with some (Vachon et al, 2007; Torres-Mejia et al, 2005), but not with all studies (Stuedal et al, 2008; Chen et al, 2004). In our study, the pseudo-R2 for absolute dense area was 1% compared with 7% for percent density. However, the negative confounding with BMI was only observed for percent density. Although the regression coefficient in the conditional logistic model for percent density increased by 20% after adjustment for BMI, the coefficient for absolute dense area decreased by 4%. Others have similarly found greater confounding with BMI for percent density than for absolute dense area (Stone et al, 2009). The negative confounding of percent density with BMI was entirely because of a positive correlation of BMI with absolute nondense area (Haars et al, 2005).
We found that density was positively associated with late first birth, lack of history of breast feeding and use of HRT, but negatively associated with other breast cancer risk factors, namely age, low parity and BMI, as reported by others (Haars et al, 2005; Dite et al, 2008). We also found that risk persisted beyond 6 years after a single mammographic density reading, supporting to the hypothesis that mammographic density may be an intermediate phenotype for breast cancer (Boyd et al, 2005) as many of the standard risk factors are irreversible by the time of menopause.
Although percent density was higher in Chinese women in our study, we could not confirm our previous finding of heterogeneity by ethnicity of the effect of density on risk (Duffy et al, 2004). Although this effect was slightly stronger in non-Chinese subjects (Table 3), it did not reach statistical significance. We did, however, find significant heterogeneity of the density effect by OC use and BMI, the increased risk associated with higher density being more pronounced in those who had used OC or in those with higher BMI. The latter result may explain the long-observed negative confounding of breast density and BMI. The higher BMI in postmenopausal women is associated with both higher risk and lower percent breast density (Boyd et al, 1998, 2007; Stone et al, 2009), but higher breast density for a given BMI confers higher risk. Our results suggest that for those whose density remains high despite high BMI, there is an increase in risk more than twice as large as that expected from the combination of the two risk factors. It should be noted that the interaction tests tend to have low statistical power because of small numbers, as reflected by the wide confidence intervals on some ORs.
Our results confirm the independent effect of breast density on breast cancer risk. We found that percent breast density was a stronger risk factor than absolute dense area, but was also more confounded with BMI. Our results indicate that density is positively related to most breast cancer risk factors, with the notable exceptions of age and BMI, the effect being increased in women with high BMI or a history of OC use.
Change history
29 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, Jong RA, Hislop G, Chiarelli A, Minkin S, Yaffe MJ (2007) Mammographic density and the risk and detection of breast cancer. N Engl J Med 356: 227–236
Boyd NF, Lockwood GA, Byng JW, Tritchler DL, Yaffe MJ (1998) Mammographic densities and breast cancer risk. Cancer Epidemiol Biomarkers Prev 7: 1133–1144
Boyd NF, Rommens JM, Vogt K, Lee V, Hopper JL, Yaffe MJ, Paterson AD (2005) Mammographic breast density as an intermediate phenotype for breast cancer. Lancet Oncol 6: 798–808
Breslow N, Day NE (1980) Statistical Methods in Cancer Research vol. 1: The Analysis of Case-control Studies. International Agency for Reseach on Cancer: Lyon
Byng JW, Yaffe MJ, Jong RA, Shumak RS, Lockwood GA, Tritchler DL, Boyd NF (1998) Analysis of mammographic density and breast cancer risk from digitized mammograms. Radiographics 18: 1587–1598
Chen J, Pee D, Ayyagari R, Graubard B, Schairer C, Byrne C, Benichou J, Gail MH (2006) Projecting absolute invasive breast cancer risk in white women with a model that includes mammographic density. J Natl Cancer Inst 98: 1215–1226
Chen Z, Wu AH, Gauderman WJ, Bernstein L, Ma H, Pike MC, Ursin G (2004) Does mammographic density reflect ethnic differences in breast cancer incidence rates? Am J Epidemiol 159: 140–147
Dite GS, Gurrin LC, Byrnes GB, Stone J, Gunasekara A, McCredie MR, English DR, Giles GG, Cawson J, Hegele RA, Chiarelli AM, Yaffe MJ, Boyd NF, Hopper JL (2008) Predictors of mammographic density: insights gained from a novel regression analysis of a twin study. Cancer Epidemiol Biomarkers Prev 17: 3474–3481
Duffy SW, Jakes RW, Ng FC, Gao F (2004) Interaction of dense breast patterns with other breast cancer risk factors in a case-control study. Br J Cancer 91: 233–236
Haars G, van Noord PA, van Gils CH, Grobbee DE, Peeters PH (2005) Measurements of breast density: no ratio for a ratio. Cancer Epidemiol Biomarkers Prev 14: 2634–2640
Jakes RW, Duffy SW, Ng FC, Gao F, Ng EH (2000) Mammographic parenchymal patterns and risk of breast cancer at and after a prevalence screen in Singaporean women. Int J Epidemiol 29: 11–19
Maskarinec G, Nagata C, Shimizu H, Kashiki Y (2002) Comparison of mammographic densities and their determinants in women from Japan and Hawaii. Int J Cancer 102: 29–33
McCormack VA, dos Santos Silva I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev 15: 1159–1169
Ng EH, Ng FC, Tan PH, Low SC, Chiang G, Tan KP, Seow A, Emmanuel S, Tan CH, Ho GH, Ng LT, Wilde CC (1998) Results of intermediate measures from a population-based, randomized trial of mammographic screening prevalence and detection of breast carcinoma among Asian women: the Singapore Breast Screening Project. Cancer 82: 1521–1528
Sala E, Warren R, McCann J, Duffy S, Day N, Luben R (1998) Mammographic parenchymal patterns and mode of detection: implications for the breast screening programme. J Med Screen 5: 207–212
Sala E, Warren R, McCann J, Duffy S, Luben R, Day N (2000) High-risk mammographic parenchymal patterns, hormone replacement therapy and other risk factors: a case-control study. Int J Epidemiol 29: 629–636
Stone J, Warren RM, Pinney E, Warwick J, Cuzick J (2009) Determinants of percentage and area measures of mammographic density. Am J Epidemiol 170: 1571–1578
Stuedal A, Ma H, Bernstein L, Pike MC, Ursin G (2008) Does breast size modify the association between mammographic density and breast cancer risk? Cancer Epidemiol Biomarkers Prev 17: 621–627
Torres-Mejia G, De Stavola B, Allen DS, Perez-Gavilan JJ, Ferreira JM, Fentiman IS, Dos Santos Silva I (2005) Mammographic features and subsequent risk of breast cancer: a comparison of qualitative and quantitative evaluations in the Guernsey prospective studies. Cancer Epidemiol Biomarkers Prev 14: 1052–1059
Vachon CM, Brandt KR, Ghosh K, Scott CG, Maloney SD, Carston MJ, Pankratz VS, Sellers TA (2007) Mammographic breast density as a general marker of breast cancer risk. Cancer Epidemiol Biomarkers Prev 16: 43–49
Acknowledgements
This work was supported by the National Medical Research Council, Singapore.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Wong, C., Lim, G., Gao, F. et al. Mammographic density and its interaction with other breast cancer risk factors in an Asian population. Br J Cancer 104, 871–874 (2011). https://doi.org/10.1038/sj.bjc.6606085
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6606085
Keywords
This article is cited by
-
Influence of breast density on breast cancer risk: a case control study in Japanese women
Breast Cancer (2020)
-
Body mass index, mammographic density, and breast cancer risk by estrogen receptor subtype
Breast Cancer Research (2019)
-
Diagnostic Efficacy of Synthesized 2D Digital Breast Tomosynthesis in Multi-ethnic Malaysian Population
Scientific Reports (2019)
-
Association between alcohol consumption and mammographic density: a hospital-based cross-sectional study
Breast Cancer (2019)
-
Combined effect of volumetric breast density and body mass index on breast cancer risk
Breast Cancer Research and Treatment (2019)