Abstract
Plasma membrane ion channels contribute to virtually all basic cellular processes, including such crucial ones for maintaining tissue homeostasis as proliferation, differentiation, and apoptosis. Enhanced proliferation, aberrant differentiation, and impaired ability to die are the prime reasons for abnormal tissue growth, which can eventually turn into uncontrolled expansion and invasion, characteristic of cancer. Prostate cancer (PCa) cells express a variety of plasma membrane ion channels. By providing the influx of essential signaling ions, perturbing intracellular ion concentrations, regulating cell volume, and maintaining membrane potential, PCa cells are critically involved in proliferation, differentiation, and apoptosis. PCa cells of varying metastatic ability can be distinguished by their ion channel characteristics. Increased malignancy and invasiveness of androgen-independent PCa cells is generally associated with the shift to a ‘more excitable’ phenotype of their plasma membrane. This shift is manifested by the appearance of voltage-gated Na+ and Ca2+ channels which contribute to their enhanced apoptotic resistance together with downregulated store-operated Ca2+ influx, altered expression of different K+ channels and members of the Transient Receptor Potential (TRP) channel family, and strengthened capability for maintaining volume constancy. The present review examines channel types expressed by PCa cells and their involvement in metastatic behaviors.
Similar content being viewed by others
Main
Historically, the first important role ascribed to plasma membrane ion channels, over 60 years ago, was their participation in cellular electrogenesis and electrical excitability. However, numerous subsequent studies have firmly established the contribution of ion channels to virtually all basic cellular behaviors, including such crucial ones for maintaining tissue homeostasis as proliferation, differentiation, and apoptosis.1, 2 The major mechanisms via which ion channels contribute to these crucial processes include: providing the influx of essential signaling ions, regulating cell volume, and maintaining membrane potential. Malignant transformation of cells resulting from enhanced proliferation, aberrant differentiation, and impaired ability to die is the prime reason for abnormal tissue growth, which can eventually turn into uncontrolled expansion and invasion, characteristic of cancer. Such transformation is often accompanied by changes in ion channel expression and, consequently, by abnormal progression of the cellular responses with which they are involved (Figure 1).
Schematic representation of the malignant transformation of prostatic cells resulting from enhanced proliferation, NE differentiation, and apoptosis resistance. These are the prime reasons for abnormal tissue growth, which can eventually turn into uncontrolled expansion and invasion, characteristic of cancer. Such transformation is often accompanied by changes in ion channel expression and, consequently, by abnormal cellular responses
Distinctions between prostate cancer (PCa) cells of varying metastatic ability can be made according to their ion channel characteristics. Because of unrestricted accessibility and convenience of experimentation, most studies on ion channel involvement in prostate carcinogenesis have been conducted on PCa epithelial cell lines of varying metastatic potential. Many cell lines are presently established from primary tissue sources and clonal derivatives of previously established lines3 The data from native human PCa tissues is much sparser and are usually obtained to confirm major conclusions derived from cell line studies.
In this review, we describe the major types of ion channels in PCa epithelial cells, establish their role in apoptosis- and differentiation-related events, and track down how they evolve during transformation to apoptotic-resistant cell phenotypes typical of advanced androgen-independent PCa.
Potassium Channels
Potassium channels are involved in the maintenance of resting potential, thereby they represent an integral part of all cells. As K+ channels provide an efflux of K+, which is the dominant cation of the intracellular medium, they are also important regulators of cell volume. K+ channels represent one of the most diverse groups of channels, consisting of five major classes: (i) voltage-gated (Kv class), (ii) Ca2+-activated (KCa class), (iii) inwardly rectifying (Kir class), (iv) ATP-sensitive (KATP class), and (v) background two-pore domain-containing (K2P class).4 Some of them have been identified in various types of carcinomas where they are involved in the proliferation and apoptosis of tumor cells.4 This is consistent with the paradigm according to which the enhanced K+ efflux is associated with apoptosis promotion and, conversely, that apoptosis is attenuated if K+ efflux is decreased.4, 5, 6 The mechanisms for proapoptotic effects of enhanced K+ efflux include: (i) decay of the membrane potential and associated calcium (Ca2+) overload, (ii) apoptotic cell shrinkage (apoptotic volume decrease, AVD) and activation of intracellular proapoptotic effectors.4, 5, 6 In particular, decreases in intracellular K+ appear to promote critical events during the early phases of cell death, including proteolytic cleavage of pro-caspase-3 and enhanced endonuclease activity.5
Among numerous K+-channel types, a member of the Kv class eag1 (ether-a-go-go) (or Kv10.1), has been found to be involved in tumorigenesis.7, 8, 9 eag1 K+ channel expression is exaggerated in several human cancers, where it is invelved in cell proliferation.9 Inhibition of endogenous eag1 commonly reduces cell proliferation, whereas heterologous overexpression enhances proliferation rate.7
PCa epithelial cells are generally characterized by quite prominent voltage-gated K+ current (IK). However, the existing data on its molecular nature are quite diverse and sometimes conflicting. This probably reflects the multichannel origin of the current as well as the multiplicity of factors that influence the patterns of their expression. Historically, in prostatic androgen-dependent LNCaP cells, the inhibition of IK exerted antiprolifereative effects, although it did not induce apoptosis.10, 11, 12 Comparison of prostatic androgen-dependent LNCaP and androgen-independent PC-3 cell lines has shown that increased malignancy is associated with lower density of voltage-gated K+ current, which potentially makes their membrane ‘more excitable’.13 However, due to their combined biophysical properties and despite the fact that primary prostate carcinoma tissue has been shown to be highly enriched with eag1 mRNA and protein,9 the endogenous IK in PCa epithelial cells could not specifically be linked to the activity of a specific K+-channel type.
The existing data suggests that Kv1.3 is the dominant Kv-class channel expressed in normal and cancerous rat and human prostate tissues, as well as in prostatic cell lines with different metastatic potentials, with lesser contributions from Kv1.4 and Kv1.6.14, 15, 16 The difference between strongly metastatic rat MAT-LyLu and weakly metastatic AT-2 cell lines was again mostly found with regard to IK density, rather than biophysical properties.16 This is consistent with the altered expression of the same channel types as opposed to the appearance of new ones. Facilitation of K+ efflux by K+-channel openers, (minoxidil, 1-ethyl-2-benzimidazolinone (EBIO), or diazoxide) was able to increase growth of PC-3 cells by 30–50%, whereas K+-channel inhibitors (dequalinium, amiodarone, and glibenclamide) caused a dose-dependent, growth inhibition of both androgen-sensitive (LNCaP, MDA-PCA-2B) and androgen-insensitive (PC-3, DU-145) human PCa cell lines.15 The same blockers induced PC-3 apoptosis within 4 h treatment.15
Thus, we can conclude that PCa epithelial cells that preserve androgen sensitivity, and display relatively weak metastatic potential, are generally characterized by higher IK and K+-channel expression. On the one hand, this promotes their proliferation, but on the other hand it makes them more prone to programmed cell death. On the contrary, lower IK and K+-channel expression of highly metastatic, androgen-insensitive cells, although reducing their proliferative activity, contributes to their apoptotic resistance.
The importance of augmented K+ efflux in apoptosis was directly confirmed in experiments with KChAP, a K+-channel regulatory protein that increases K+-channel expression in a ‘chaperone-like’ fashion in heterologous expression systems.17 Overexpression of KChAP in LNCaP cells, decreased the average cell size due to enhanced AVD, promoted spontaneous cells apoptosis.18 Moreover, repetitive overexpression of KChAP during 19 days in LNCaP and DU-145 tumor xenografts in nude mice significantly suppressed tumor growth due to the apoptosis of infected tumor cells. The mechanism of proapoptotic KChAP action could be due to direct interaction with K+ channels, thereby increasing their expression. Overexpression of KChAP in LNCaP cells also produced G0/G1 cell-cycle arrest via the activation of p53 (the tumor suppressor protein) acting as a transcription factor. However, the involvement of p53 in proapoptotic KChAP activity was ruled out based on the fact that KChAP was able to induce similar apoptosis in DU-145 cells expressing mutated p53, rendering it nonfunctional as a transcription factor.18
Pharmacological data also suggest the presence of KCa-class channel representatives in PCa cells. Indeed, in LNCaP and PC-3 cells, the activation of KCa channels enhanced cell proliferation. The mechanism underlying the regulation of cell proliferation by IKCa channels remains to be elucidated, these results highlight the importance of Ca2+-dependent K+ efflux in general on IKCa channels, especially in the proliferation of human PCa cells.
Interestingly, a recent electrophysiological study has also identified large-conductance (BKCa) KCa channels in LNCaP cells, although with quite unusual voltage- and [Ca2+]in-dependence. This may be due to a unique subunit composition of the channel.19 BKCa channel expression was regulated by serum-derived factors, as serum deprivation strongly reduced whole-cell current density. Current decrease in serum-deprived medium was unaffected by either an antagonist (bicalutamide, Casodex®) or an agonist (R1881) of androgen receptor (AR), suggesting that these factors were apparently not androgens.19 It is known that serum starvation induces neuroendocrine (NE) differentiation of LNCaP cells.13, 14 Therefore, reduction of BKCa channels may play an important role in this process, especially in light of the simultaneous increase in the expression of low-voltage-activated (LVA) calcium channels in NE cells.13
In conclusion, K+ channels seem to play an important role in the control of PCa cells growth by regulating membrane potential and passive calcium influxes. However, further studies are needed to identify the precise role of each type of K+ channels in carcinogenesis for their potential utilization as diagnostic/prognostic markers and/or therapeutic targets.
Voltage-Gated Sodium and Calcium Channels
The notion that increased malignancy of PCa cells is associated with the shift to a ‘more excitable’ phenotype of their plasma membrane is supported not only by the decrease in K+ conductances, as described above, but also by the appearance of inward currents characteristic of excitable cells, such as voltage-gated Na+ and Ca2+ currents. Indeed, in several PCa epithelial cells, the expression of voltage-gated Na+ channels (VGSCs) on functional, protein and mRNA levels has been firmly established.20, 21, 22, 23 Moreover, VGSCs activity can enhance the metastatic behavior of cells, including their proliferation. VGSC opener veratrine has been shown to increase growth of not only androgen-insensitive PC-3 and DU-145 cells (for which functional channel activity was documented), but also of androgen-sensitive LNCaP and MDA-PCA-2B cell lines, which apparently do not display such activity.21 At the same time, VGSC blockers (flunarizine, and riluzole) induced dose-dependent growth-inhibition of all four cell lines.21
RT-PCR analysis identifies tetrodotoxin-(TTX)-sensitive Nav1.7 as the most upregulated (approximately 20-fold) Na+-channel α subunit in PCa.23 Furthermore, TTX has been shown to directly reduce the invasiveness of the cells,17 thus suggesting Na+ channels as a viable target for anti-PCa research. All this strongly supports the notion that expression of VGSCs and the metastatic behaviors of PCa cells are functionally related. However, the mechanism(s) responsible for VGSCs upregulation, as well as their pro-metastatic action, are still poorly understood. It is suggested that VGSCs expression may endow the membranes of PCa epithelial cells with electrophysiological properties that enhance their motility24 and/or secretory activities,25 as well as perturb intracellular ionic homeostasis. Indeed, it has been directly demonstrated that, whereas VGSC blockers (TTX and phenytoin) reduce, VGSC openers (aconitine, ATX II) enhance the migration of metastatic human PC-3 or rat MAT-LyLu cells without influencing the motility of weakly metastatic human LNCaP and rat AT-2 cells.24, 26 However, the questionability of pharmacological tools (i.e. specificity and side effects) may compromise the conclusions drawn; therefore, other approaches (i.e. siRNAs, overexpression studies) need to be used to conclude on the precise role of Na+ channels in PCa.
The prostate contains an abundance of high-affinity dihydropyridine (DHP)-binding sites.27 It has also been shown that the percentage of epithelial rat ventral prostate cells undergoing apoptosis in response to androgen ablation is reduced by administering voltage-gated Ca2+ channel (VGCC) blockers such as nifedipine and verapamil.28, 29 These observations have given rise to the hypothesis that calcium channel blockers, by inhibiting calcium signal-mediated apoptosis, may increase the risk of PCa.17 Despite this indirect evidence, the presence of VGCC activity has not been detected in PCa epithelial cells by means of electrophysiology. Therefore, as in the case of Na+ channels, the role of DHP-sensitive Ca2+ channels in PCa remains questionable until other experimental approaches rather than pharmacological ones, will confirm their expression and activity.
Nevertheless, the progression of Pca to the androgen-insensitivity stage is accompanied by the appearance of new apoptosis-resistant cell phenotypes. The enrichment of androgen-independent tumors with malignant NE cells should especially be noted. Fully differentiated, nonproliferating, neuron-like NE cells are a normal component of the prostate epithelium which, by releasing a variety of neurosecretory products, regulate the development and secretory activity of the prostate in the endocrine/paracrine manner.30, 31 Generally, prostatic NE cells express a variety of membrane ion channels characteristic of neurons, like TTX-resistant VGSCs, high-voltage-activated (HVA) Ca2+ channels of L- and N-type, Kv, KCa, and Kir representatives, and are also able to generate action potentials.32 However, an expanding population of NE cells beyond normal proportions due to the malignant transformation of epithelial/basal cells is a common characteristic of Pca progression.30 NE cells lack nuclear AR, thereby representing an androgen-insensitive cell phenotype in the prostate.33 They also exhibit high apoptosis resistance34 which, according to existing evidence, is unrelated to the common antiapoptotic Bcl-2 protein,35 and conferred instead by new survival proteins, survivin36 and clusterin.37
Findings showing the small proportion of undifferentiated LNCaP cells displaying an LVA Ca2+ current carried by T-type Ca2+ channels, and the number of cells showing this type of current, as well as the significantly increased current density during the NE differentiation of LNCaP cells induced by either long-term treatments with membrane permeable cAMP analogs or by steroid-deprived culture medium38 is of special importance. RT-PCR experiments demonstrated that only mRNA for Cav3.2 isoform of T-type Ca2+ channel α1 subunit is expressed in LNCaP cells, and becomes highly elevated during NE differentiation.38 It was also shown that basal Ca2+ entry through this channel at resting membrane potential due to the presence of a prominent ‘window current’ is likely to facilitate neurite elongation, thereby promoting NE differentiation. It was suggested that this channel could be also involved in the stimulation of mitogenic factor secretion, thus representing an attractive potential target for future therapeutic strategies.38 However, whether or not these channels contribute to the enhanced antiapoptotic potential of NE cells is not yet clear.
Store-operated Calcium Entry and TRP Channels
The role of Ca2+ in the majority of cell-signaling pathways involved in carcinogenesis is well established. Calcium homeostasis, the consequences of calcium signaling, is a steady state between influx, efflux, and storage of Ca2+. From a physiological point of view, Ca2+ signaling is involved in the manifestation of cell phenotype, proliferation, differentiation, apoptosis, and in cellular activities such as contraction or secretion or cell excitability. Thus, each cellular phenotype, whether normal or pathological, is characterized by a particular ‘Calcium Signature’ reflecting its kinetics, amplitude and subcellular localization of the calcium signals. Indeed, if the oscillations of the cytosolic calcium stimulate cell proliferation via activation of the Ca2+-dependent transcription factor, NFAT,39 a sustained elevation in cytosolic Ca2+ concentration induces apoptosis of cancer cells40 (Figure 2). Because the problem of Ca2+ homeostasis in cancer cells is too vast, even in relation to PCa cells, we will limit ourselves to characterizing channels only, and refer the reader to other comprehensive reviews for more in-depth information.41, 42, 43, 44, 45, 46
Spatio-temporal regulation of Ca2+ signaling. This regulation is characterized by a particular ‘Calcium Signature’ reflecting its kinetics (duration and frequency), amplitude and subcellular localization of the calcium signals. For example, if the oscillations of the cytosolic Ca2+ stimulate cell proliferation via activation of the Ca2+-dependent transcription factor, NFAT, a sustained elevation in cytosolic Ca2+ concentration induces apoptosis of cancer cells
In PCa epithelial cells, as in other nonexcitable cell types, Ca2+ entry from extracellular space is mainly supported by the ‘capacitative calcium entry’ (CCE) mechanism, also known as ‘store-operated calcium entry’ (SOCE) (reviewed by Parekh and Putney47). This mechanism is capable of monitoring edoplasmic reticulum (ER) Ca2+ filling, enabling influx only when ER content is essentially decreased. It is mediated via specialized plasma membrane store-operated Ca2+-permeable channels (SOC). The common physiological trigger for the activation of these channels is inositol trisphosphate-(IP3)-induced Ca2+ release from the ER in response to the stimulation of surface receptors coupled to the phospholipase C-(PLC)-catalyzed inositol phospholipid breakdown signaling pathway. This is why, when these channels have been identified for the first time by patch-clamp experiments, they were termed ‘Ca2+ release-activated channels’ (CRAC).48
Alterations in calcium homeostasis and in SOC activity seem to play a major role in the establishment of androgen-independent apoptosis-resistant phenotype of PCa. Indeed, the major features of Ca2+ homeostasis in androgen-independent apoptosis-resistant PCa cells (such as LNCaP cells stably transfected with Bcl-2 and NE differentiated LNCaP cells) compared to the wild-type androgen-dependent LNCaP cells are: (i) reduced basal Ca2+ filling of the ER pool, and (ii) reduced store-operated Ca2+ entry.49 These changes were accompanied by the increased resistance to TG- and TNFα-induced apoptosis with clear shift to higher importance of Ca2+ influx versus ER store depletion in apoptosis induction compared to the wild-type androgen-dependent LNCaP cells.49 Therefore, identification the molecular nature of SOC and the mechanisms of their activation/regulation is of great importance for understanding of what drives PCa to androgen-independence. However, years of frustration marked the quest for molecular basis of SOC and for molecules underlying the process of capacitative calcium entry. Fortunately, these questions seem to be resolved now due to the very recent series of publications on STIM1 (stomal interaction molecule 1), identified as the mammalian ER Ca2+ sensor,50, 51 closely followed by identification of Orai1/CRACM1 as a component of the mammalian CRAC channel.52 The role of these proteins in PCa progression is not yet studied, but it is obvious that STIM1 and ORAIs could represent new candidates for PCa research.
Last years, some members of the widely investigated family of mammalian homologs of the Drosophila TRP (transient receptor potential) channel were viewed as being involved in SOC formation (for recent reviews see Parekh and Putney,47 Pedersen et al.,53 Ramsey et al.54). Our own studies conducted on androgen-dependent LNCaP cells have suggested the involvement of the members of the ‘canonical’ TRP subfamily, TRPC1 and TRPC4, in prostate-specific endogenous SOCs.55, 56 However, the expression pattern of TRPC1 and TRPC4 was not modified in androgen-independent apoptosis-resistant PCa cells (Vanden Abeele et al.56). Interestingly, the activity of a member of the ‘vanilloid’ TRP subfamily, TRPV6, may also have some relation to the sequence of events following to ER depletion in LNCaP cells, as its antisense knockout decreases endogenous store-operated membrane current (ISOC),57, 58 but the mechanisms underlying such TRPV6 activation in LNCaP cells remain elusive. However, in PCa, TRPV6, formerly known as Ca2+ transporter type 1 (CaT1) or epithelial calcium channel 2 (ECaC2),59 attracts special attention even beyond its potential role in calcium influx, as its expression was shown to correlate with PCa grade.60, 61, 62 A study conducted on tissue samples from 140 patients with PCa demonstrated the association of TRPV6 with PCa progression and suggested it as a prognostic molecular marker in cancer classification.60 Moreover, it has been demonstrated that heterologous TRPV6 expression in HEK-293 cells promotes their proliferation in a Ca2+-dependent manner by increasing [Ca2+]in levels, which is a prerequisite for its potential role in tumor progression.63 It seems, however, that the functional role of endogenous TRPV6 in prostatic ISOC is closely linked to other potential SOC constituents and/or regulators, because heterologous TRPV6 overexpression in LNCaP cells resulted in the appearance of additional membrane current with properties distinct from endogenous ISOC.64 In any event, the problem of molecular basis for SOCE in PCa epithelial cells is still far from being resolved.
It is well established that various cellular Ca2+-dependent processes rely on the specific spatial and temporal patterns of Ca2+ signaling.65 However, the type and manner of their organization during carcinogenesis is not sufficiently defined. For instance, in PCa epithelial cells, stimulation of two receptors, α1-adrenoceptor (α1-AR) and metabotropic purinergic receptor (P2Y-R), produce divergent effects on cell proliferation: α1-AR stimulation enhances proliferation,39, 66 whereas P2Y-R stimulation results in growth arrest.40, 66 Such divergent effects on proliferation are quite surprising, given that both receptors act via a common PLC-catalyzed inositol phospholipid breakdown signaling pathway that results in the derivation of IP3 and diacylglycerol (DAG), two second messengers important for Ca2+ signaling. Our recent studies on primary human PCa epithelial cells provided some understanding of these puzzling observations.66 We have shown that Ca2+ signaling controlled by each receptor relies on different Ca2+-entry pathways, ultimately targeting various intracellular effectors. It appeared that stimulation of α1-AR activates plasma membrane nonspecific cationic channels via direct DAG gating,39, 66 without affecting ER Ca2+ stores, whereas P2Y-R stimulation brings about IP3 receptor-mediated ER store depletion and activation of SOCs.40, 66 Consistent with these peculiarities, the α1-AR agonist, phenylephrin, stimulated oscillatory-type intracellular Ca2+ signaling involving membrane current through DAG-gated cationic channels (IDAG), whereas the P2Y-R agonist, ATP, induced a transient [Ca2+]in increase, followed by a smaller sustained increase due to store depletion and SOC activation (Figure 3). The two Ca2+ entry pathways also appeared to have a different molecular nature, with the first one mostly relying on a DAG-gated TRP member, TRPC6, and the second one on TRPC1 and TRPC4.
Differential role of TRP channels in agonist-stimulated calcium signaling and PCa cell proliferation. (a) Typical pattern of cytosolic Ca2+ oscillations induced in primary cultured human PCa epithelial cells by the agonist of α1-adrenergic receptors (α1-AR), phenylephrine (PHE, 10 μM); the importance of Ca2+ entry for supporting oscillatory activity and the inability of PHE-to induced Ca2+ release is evidenced by the lack of any signal in the absence of extracellular Ca2+ (0Ca2+); cells incubated in the presence of PHE (10 μM) for 2 days enhanced proliferation by almost 40% compared to control conditions (CTL) (c). (b) The shape of cytosolic Ca2+ signal in primary cultured human PCa epithelial cells induced by the purinergic receptor (P2Y-R) agonist, ATP (10 μM); in the absence of extracellular Ca2+ (0Ca2+), ATP mobilizes of intracellularly stored Ca2+, followed by quasi-sustained store-operated Ca2+ entry upon re-exposure to Ca2+ (2Ca2+); cell culturing in the presence of ATP (100 μM) for 2 days delayed proliferation by 60% (c). (c) The effects of two agonists on human PCa epithelial cell proliferation. (d and e) Antisense knockout of store-independent, DAG-gated TRP member, TRPC6, does not affect ATP-induced Ca2+ signals (measured as maximal [Ca2+]i increase in the presence of 2 mM Ca2+), but greatly attenuates PHE-induced ones (because of its oscillatory nature measured as an integral of [Ca2+]i over a 30-min period) (d), and vice versa, similar knockout of a store-dependent TRP member, TRPC1, significantly reduces the ATP-evoked Ca2+ signal, but leaving the PHE-induced one unaffected (e)
Moreover, our data show that α1-AR stimulation enhances Pca epithelial cell proliferation by inducing store-independent, TRPC6-mediated Ca2+ entry resulting in the activation of NFAT transcription factor via its Ca2+/calmodulin/calcineurin nuclear translocation pathway.66 TRPC6 antisense knockout exerted effects similar to those of pharmacological α1-AR inhibition, that is, suppression of agonist-induced Ca2+ entry, cessation of oscillatory-type Ca2+ signaling, and consequent termination of cell proliferation. Furthermore, chronic treatment with α1-agonists enhanced TRPC6 protein expression, as well as altered the expression of two cell-cycle regulators, CDK4 and cyclin-dependent kinase inhibitor p27. This provides direct evidence for the α1-AR–TRPC6–NFAT–cell proliferation link. In contrast, Ca2+ entry associated with P2Y-R stimulation by extracellular ATP and related growth arrest did not involve either TRPC6 channel activation or NFAT translocation. Our findings demonstrate that the α1-AR-dependent Ca2+ signaling that promotes proliferation of Pca epithelial cells specifically requires the activation of TRPC6 channels coupled to NFAT, thereby suggesting TRPC6 as a promising new target for controlling Pca cell proliferation.
It should be noted that clinical studies also implicate α1-AR antagonists as proapoptotic agents capable of inducing apoptosis of human Pca epithelial and smooth muscle cells without affecting cellular proliferation.67 However, these effects seem to be unrelated to α1-AR68 and Ca2+ signaling associated with it.
Interestingly, the endogenous expression of TRPC1, TRPC3, and TRPV6 proteins per se in LNCaP cells was shown to controlled by the ER Ca2+ filling: after a prolonged (24–48 h) depletion of the stores with thapsigargin, a potent proapoptotic agent, their expression increased.69 Enhanced expression of apparently store-dependent TRP members under ER store depletion is difficult to reconcile with the findings that androgen-independent, apoptosis-resistant PCa cell phenotypes, for which chronic underfilling of the ER Ca2+ pool represents a new level of equilibrium helping them to withstand ER stress-mediated apoptosis, are characterized by reduced SOCE.49, 70, 71 It is, therefore, likely that native SOC in Pca epithelial cells is a much more complex entity, whose functional expression cannot be directly correlated with any of the implicated TRP members. In this respect, it is important to assess the role of STIM1 and CRACM1 (Orai1) proteins in PCa cell SOCE.
Cold/menthol-sensitive TRPM8 of the ‘melastatin’ TRP subfamily is yet another TRP member that has recently emerged as an important player in normal and pathological development of the prostate, whose real significance, however, is only beginning to unfold. Although TRPM8 was initially identified as a cold/menthol receptor mediating cold-evoked excitation in sensory neurons,72, 73 in fact, it was first cloned from the human prostate as a prostate-specific gene74 before its role in cold sensation was established. Our data,75 as well as those of others,76 indicate that TRPM8 is expressed not only in the plasma membrane of prostate cells, as initially anticipated, but also in the ER membrane, where it operates as an ER Ca2+ release channel involved in the activation of SOCE in response to cold/menthol stimulus. Moreover, whereas remaining at moderate levels in a normal prostate, TRPM8 expression strongly increases in Pca. For this reason, it has been proposed to be a pro-oncogenic actor in PCa cells.74 Other nonprostatic primary human tumors (breast, colon, lung, and skin) also become highly enriched in TRPM8, although it is virtually undetectable in corresponding normal tissues.74 Thus, even this initial information strongly pointed to much broader roles of TRPM8 beyond cold sensation, especially in the prostate and during carcinogenesis. The role of TRPM8 in organs not exposed to ambient temperatures, and especially in prostate gland, remains a gnawing mystery. However, the data accumulated last years allow hypothesizing on that.
In normal prostate, trpm8 gene expression seems to be directly controlled by AR,76, 77 positioning it as a primary androgen-response gene.77 Single-cell RT-PCR and immunohistochemical experiments conducted on primary human PCa cells have shown that TRPM8 is mainly expressed in androgen-dependent, apical secretory epithelial cells, and that its expression becomes downregulated in cells loosing the AR activity and regressing to the basal epithelial phenotype.77 Mature epithelial cells are nonproliferative cells, highly sensitive to apoptotic stimuli (due to the specific regulation of the expression of genes belonging to Bcl-2 family: antiapoptotic Bcl-2 gene expression is repressed, whereas proapoptotic Bax gene expression is stimulated by AR).78, 79, 80 Nevertheless, the secretion of products (including citric acid, prostate-specific antigen (PSA), acid phosphatase, several enzymes and lipids) is the major function of apical epithelial prostate cells. Therefore, considering the specific TRPM8 expression in these cells, we suggested the potential role of this channel in secretion.
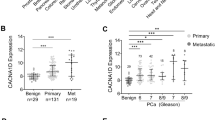
In PCa tumors, a significant difference in mRNA expression level of TRPM8 between malignant and nonmalignant tissue specimens has been detected.81 This was comparable to the currently used PCa marker, PSA, thus, qualifying TRPM8 as its potential competitor in PCa diagnosis and staging. A significant difference in TRPM8 expression between human benign prostate hyperplasia and PCa tissues is also obvious at protein level (Figure 4). According to Tsavaler's hypothesis defining trpm8 as an oncogene,74 TRPM8 overexpression and overactivity in circumscribed, androgen-dependent PCa may be correlated to the higher rate of growth of these cells compared to normal ones.82, 83 During the transition to androgen independence, TRPM8 is lost in xenograft model and also in PCA tissue from patients treated preoperatively with antiandrogen therapy, suggesting that its loss may be associated with a more advanced form of the disease.84 According to a clinical study describing that androgen-independent PCa metastasis proliferate more slowly than the androgen-dependent ones,83 our unpublished results demonstrated that LNCaP cells resistant to anti-androgen bicalutamide treatment (LNCaP-bicR) displayed a reduced doubling time. This is correlated to a decreased expression of AR, TRPM8 and the proliferating cell nuclear antigen (PCNA) mRNAs, whereas antiapoptotic Bcl-2 mRNA expression is increased (Figure 5). All these data reinforce the putative proproliferative role of TRPM8 in androgen-dependent PCa cells.
PCa-specific enhancement of cold/menthol-sensitive TRPM8 channel expression. (a and b) Confocal images of human benign prostate hyperplasia (BPH, a) and PCa (b) tissue samples stained with TRPM8-specific antibody (code: ab3243, Abcam, Cambridge, UK) showing much higher TRPM8 protein expression in PCa
Transition of metastatic PCa cells to androgen-independence leads to a decreased proliferation and strong shifts in gene expression. (a) Comparison of doubling time of LNCaP cell line and of an LNCaP subclone resistant to bicalutamide treatment (LNCaP-bicR obtained after a 10-month 100 μM bicalutamide selection). Addition of 20 μM bicalutamide increased the doubling time of LNCaP cells, but do not affect the proliferation of LNCaP-bicR. (b) Normalized expression of AR, TRPM8, Bcl-2, and PCNA mRNA in both LNCaP cells and LNCaP-bicR cells figured out with PCR experiment. LNCaP-bicR cells displayed a significant decrease of AR, TRPM8 and cell-cycle-associated PCNA expression, although antiapoptotic Bcl-2 mRNA level was increased
Finally, Barritt's group has demonstrated that both pharmacological activation of TRPM8 and siRNA-mediated TRPM8 silencing in LNCaP cells can decrease the cell viability,76 probably by perturbing the TRPM8-dependent intracellular Ca2+ homeostasis. However, it is still not clear whether TRPM8 involvement in cell viability is carried out through a proproliferative and/or an antiapoptotic mechanism.
Chloride Channels
Activation of the chloride current through specialized volume-regulated anion channels (VRACs) in response to cell swelling (ICl,swell) is one of the major mechanisms by which cells tend to restore their volume following hypo-osmotic stress – a process known as regulatory volume decrease (RVD) (reviewed by Furst et al.,85 Okada et al.86). Extracellular osmotic perturbations are not the only reason for alterations in cell volume. Effectively counteracting abrupt volume changes and maintaining relative volume constancy during active solute uptake, exocytosis, proliferation, and differentiation are major prerequisites for cell survival. Indeed, there is strong evidence that disordered or altered cell volume regulation is associated with apoptosis.86 Compelling support for such an association has been provided by demonstrating the direct causal link between apoptotic resistance conferred by antiapoptotic Bcl-2 protein and the strengthening of RVD capability due to upregulation of ICl,swell.87, 88
Using LNCaP cells, we have shown that PCa cells are endowed with the powerful ICl,swell, which provides an effective RVD under hypoosmotic stress,89, 90 and that the magnitude of this current, as well as the capability of an even further increase in RVD with cell transition to androgen-independence and apoptosis resistance.88, 91 Moreover, the enhancement of ICl,swell and the related strengthening of RVD appeared to be independent on the specific reasons for such a transition: overexpression of the common antiapoptotic Bcl-2 protein or NE differentiation, suggesting that it represents a general phenomenon.
Although the molecular nature of native ICl,swell-carrying VRACs is not known, and several membrane proteins are considered as potential candidates,85, 86 our data are also consistent with ClC-3 protein92 involvement in prostate-specific VRAC, as well as with its upregulation in androgen-independent PCa cell phenotypes.88, 91 Importantly, it appears that Ca2+ homeostasis and volume homeostasis of PCa cells are interrelated due to functional coupling of SOCs and VRACs in confined plasma membrane caveolae microdomains,56 enabling Ca2+ entering the cell via SOCs to exert inhibitory action on VRACs.90 Such coupling is partly responsible for the upregulation of ICl,swell in androgen-insensitive, apoptosis-resistant PCa cell phenotypes. Indeed, these cells are generally characterized by reduced ISOC, most likely due to the diminished number of functional SOCs.49, 70, 71 Therefore, less baseline inhibition of VRACs is expected. In turn, downregulation of SOCs and SOCE in androgen-insensitive, apoptosis-resistant PCa cells apparently represents an adaptive response to chronic underfilling of their ER Ca2+ pools resulting from enhanced ER leak, accompanied by the decreased expression of ER luminal Ca2+-binding protein, calreticulin, and SERCA2b Ca2+ pump isoform.49, 70
Conclusions
Figure 6 presents a summary of various membrane currents and associated ion channels identified in PCa cells, and their possible involvement in metastatic behavior. All of these channels potentially represent attractive targets for diagnosis, staging and/or treatment of PCa. However, more studies are needed, especially in in vivo systems, before any of them will result in practical implications.
Summary of membrane currents and respective ion channels in prostate cancer (PCa) epithelial cells and their involvement in metastatic behaviors of androgen-sensitive and androgen-insensitive cell phenotypes.'↑' denotes upregulation, ‘↓’ – downregulation, ‘?’ – information is not available; channel designations correspond to accepted nomenclatures; all other abbreviations are presented in the abbreviations list
Abbreviations
- AR:
-
androgen receptor
- AVD:
-
apoptotic volume decrease
- [Ca2+]in:
-
intracellular Ca2+ concentration
- CRAC:
-
Ca2+ release-activated channel
- DAG:
-
diacylglycerol
- ER:
-
endoplasmic reticulum
- ICl,swell:
-
swelling-activated Cl− current
- IDAG:
-
current through DAG-gated cationic channels
- IK:
-
K+ current
- Imenthol:
-
menthol-activated current through cold/menthol-sensitive TRPM8
- IP3:
-
inositol trisphosphate
- ISOC:
-
store-operated membrane current
- LVA:
-
low voltage-activated
- NE:
-
neuroendocrine
- PCa:
-
prostate cancer
- PLC:
-
phospholipase C
- RVD:
-
regulatory volume decrease
- SOC:
-
store-operated channel
- SOCE:
-
store-operated calcium entry
- TEA:
-
tetraethylammonium
- TTX:
-
tetrodotoxin
- VGCC, voltage-gated Ca2+ channel, VGSC:
-
voltage-gated sodium channel
- VRAC:
-
volume-regulated anion channel
References
Lang F, Foller M, Lang KS, Lang PA, Ritter M, Gulbins E et al. Ion channels in cell proliferation and apoptotic cell death. J Membr Biol 2005; 205: 147–157.
Razik MA, Cidlowski JA . Molecular interplay between ion channels and the regulation of apoptosis. Biol Res 2002; 35: 203–207.
Sobel RE, Sadar MD . Cell lines used in prostate cancer research: a compendium of old and new lines – part 1. J Urol 2005; 173: 342–359.
Wang Z . Roles of K+ channels in regulating tumour cell proliferation and apoptosis. Pflugers Arch 2004; 448: 274–286.
Remillard CV, Yuan JX . Activation of K+ channels: an essential pathway in programmed cell death. Am J Physiol Lung Cell Mol Physiol 2004; 286: L49–L67.
Yu SP . Regulation and critical role of potassium homeostasis in apoptosis. Prog Neurobiol 2003; 70: 363–386.
Hemmerlein B, Weseloh RM, Mello de Queiroz F, Knotgen H, Sanchez A, Rubio ME et al. Overexpression of Eag1 potassium channels in clinical tumours. Mol Cancer 2006; 5: 41.
Pardo LA, Contreras-Jurado C, Zientkowska M, Alves F, Stuhmer W . Role of voltage-gated potassium channels in cancer. J Membr Biol 2005; 205: 115–124.
Pardo LA, del Camino D, Sanchez A, Alves F, Bruggemann A, Beckh S et al. Oncogenic potential of EAG K(+) channels. EMBO J 1999; 18: 5540–5547.
Rybalchenko V, Prevarskaya N, Van Coppenolle F, Legrand G, Lemonnier L, Le Bourhis X et al. Verapamil inhibits proliferation of LNCaP human prostate cancer cells influencing K+ channel gating. Mol Pharmacol 2001; 59: 1376–1387.
Skryma R, Van Coppenolle F, Dufy-Barbe L, Dufy B, Prevarskaya N . Characterization of Ca(2+)-inhibited potassium channels in the LNCaP human prostate cancer cell line. Receptors Channels 1999; 6: 241–253.
Skryma RN, Prevarskaya NB, Dufy-Barbe L, Odessa MF, Audin J, Dufy B . Potassium conductance in the androgen-sensitive prostate cancer cell line LNCaP: involvement in cell proliferation. Prostate 1997; 33: 112–122.
Laniado ME, Fraser SP, Djamgoz MB . Voltage-gated K(+) channel activity in human prostate cancer cell lines of markedly different metastatic potential: distinguishing characteristics of PC-3 and LNCaP cells. Prostate 2001; 46: 262–274.
Abdul M, Hoosein N . Expression and activity of potassium ion channels in human prostate cancer. Cancer Lett 2002; 186: 99–105.
Fraser SP, Grimes JA, Diss JK, Stewart D, Dolly JO, Djamgoz MB . Predominant expression of Kv1.3 voltage-gated K+ channel subunit in rat prostate cancer cell lines: electrophysiological, pharmacological and molecular characterisation. Pflugers Arch 2003; 446: 559–571.
Ouadid-Ahidouch H, Van Coppenolle F, Le Bourhis X, Belhaj A, Prevarskaya N . Potassium channels in rat prostate epithelial cells. FEBS Lett 1999; 459: 15–21.
Anderson JD, Hansen TP, Lenkowski PW, Walls AM, Choudhury IM, Schenck HA et al. Voltage-gated sodium channel blockers as cytostatic inhibitors of the androgen-independent prostate cancer cell line PC-3. Mol Cancer Ther 2003; 2: 1149–1154.
Wible BA, Wang L, Kuryshev YA, Basu A, Haldar S, Brown AM . Increased K+ efflux and apoptosis induced by the potassium channel modulatory protein KChAP/PIAS3beta in prostate cancer cells. J Biol Chem 2002; 277: 17852–17862.
Gessner G, Schonherr K, Soom M, Hansel A, Asim M, Baniahmad A et al. BKCa channels activating at resting potential without calcium in LNCaP prostate cancer cells. J Membr Biol 2005; 208: 229–240.
Abdul M, Hoosein N . Voltage-gated sodium ion channels in prostate cancer: expression and activity. Anticancer Res 2002; 22: 1727–1730.
Bennett ES, Smith BA, Harper JM . Voltage-gated Na+ channels confer invasive properties on human prostate cancer cells. Pflugers Arch 2004; 447: 908–914.
Diss JK, Archer SN, Hirano J, Fraser SP, Djamgoz MB . Expression profiles of voltage-gated Na(+) channel alpha-subunit genes in rat and human prostate cancer cell lines. Prostate 2001; 48: 165–178.
Diss JK, Stewart D, Pani F, Foster CS, Walker MM, Patel A et al. A potential novel marker for human prostate cancer: voltage-gated sodium channel expression in vivo. Prostate Cancer Prostatic Dis 2005; 8: 266–273.
Fraser SP, Salvador V, Manning EA, Mizal J, Altun S, Raza M et al. Contribution of functional voltage-gated Na+ channel expression to cell behaviors involved in the metastatic cascade in rat prostate cancer: I. Lateral motility. J Cell Physiol 2003; 195: 479–487.
Mycielska ME, Fraser SP, Szatkowski M, Djamgoz MB . Contribution of functional voltage-gated Na+ channel expression to cell behaviors involved in the metastatic cascade in rat prostate cancer: II. Secretory membrane activity. J Cell Physiol 2003; 195: 461–469.
Scorey N, Fraser SP, Patel P, Pridgeon C, Dallman MJ, Djamgoz MB . Notch signalling and voltage-gated Na+ channel activity in human prostate cancer cells: independent modulation of in vitro motility. Prostate Cancer Prostatic Dis 2006; 9: 399–406.
Rosenthal E, Shapiro E, Lepor H . Characterization of 1,4, dihydropyridine calcium channel binding sites in the human prostate. J Urol 1990; 144: 1539–1542.
Connor J, Sawczuk IS, Benson MC, Tomashefsky P, O'Toole KM, Olsson CA et al. Calcium channel antagonists delay regression of androgen-dependent tissues and suppress gene activity associated with cell death. Prostate 1988; 13: 119–130.
Martikainen P, Isaacs J . Role of calcium in the programmed death of rat prostatic glandular cells. Prostate 1990; 17: 175–187.
Abrahamsson PA . Neuroendocrine cells in tumour growth of the prostate. Endocr Relat Cancer 1999; 6: 503–519.
di Sant'Agnese PA . Neuroendocrine differentiation in prostatic carcinoma: an update. Prostate Suppl 1998; 8: 74–79.
Kim JH, Shin SY, Yun SS, Kim TJ, Oh SJ, Kim KM et al. Voltage-dependent ion channel currents in putative neuroendocrine cells dissociated from the ventral prostate of rat. Pflugers Arch 2003; 446: 88–99.
Bonkhoff H . Neuroendocrine differentiation in human prostate cancer. Morphogenesis, proliferation and androgen receptor status. Ann Oncol 2001; 12 (Suppl 2): S141–S144.
Fixemer T, Remberger K, Bonkhoff H . Apoptosis resistance of neuroendocrine phenotypes in prostatic adenocarcinoma. Prostate 2002; 53: 118–123.
Xue Y, Verhofstad A, Lange W, Smedts F, Debruyne F, de la Rosette J et al. Prostatic neuroendocrine cells have a unique keratin expression pattern and do not express Bcl-2: cell kinetic features of neuroendocrine cells in the human prostate. Am J Pathol 1997; 151: 1759–1765.
Xing N, Qian J, Bostwick D, Bergstralh E, Young CY . Neuroendocrine cells in human prostate over-express the anti-apoptosis protein survivin. Prostate 2001; 48: 7–15.
July LV, Akbari M, Zellweger T, Jones EC, Goldenberg SL, Gleave ME . Clusterin expression is significantly enhanced in prostate cancer cells following androgen withdrawal therapy. Prostate 2002; 50: 179–188.
Mariot P, Vanoverberghe K, Lalevee N, Rossier MF, Prevarskaya N . Overexpression of an alpha 1H (Cav3.2) T-type calcium channel during neuroendocrine differentiation of human prostate cancer cells. J Biol Chem 2002; 277: 10824–10833.
Thebault S, Roudbaraki M, Sydorenko V, Shuba Y, Lemonnier L, Slomianny C et al. alpha1-adrenergic receptors activate Ca(2+)-permeable cationic channels in prostate cancer epithelial cells. J Clin Invest 2003; 111: 1691–1701.
Vanoverberghe K, Mariot P, Vanden Abeele F, Delcourt P, Parys JB, Prevarskaya N . Mechanisms of ATP-induced calcium signaling and growth arrest in human prostate cancer cells. Cell Calcium 2003; 34: 75–85.
Hajnoczky G, Davies E, Madesh M . Calcium signaling and apoptosis. Biochem Biophys Res Commun 2003; 304: 445–454.
Orrenius S, Zhivotovsky B, Nicotera P . Regulation of cell death: the calcium-apoptosis link. Nat Rev Mol Cell Biol 2003; 4: 552–565.
Rizzuto R, Pinton P, Ferrari D, Chami M, Szabadkai G, Magalhaes PJ et al. Calcium and apoptosis: facts and hypotheses. Oncogene 2003; 22: 8619–8627.
Lipskaia L, Lompre AM . Alteration in temporal kinetics of Ca2+ signaling and control of growth and proliferation. Biol Cell 2004; 96: 55–68.
Munaron L, Antoniotti S, Lovisolo D . Intracellular calcium signals and control of cell proliferation: how many mechanisms? J Cell Mol Med 2004; 8: 161–168.
Santella L, Ercolano E, Nusco GA . The cell cycle: a new entry in the field of Ca2+ signaling. Cell Mol Life Sci 2005; 62: 2405–2413.
Parekh AB, Putney Jr JW . Store-operated calcium channels. Physiol Rev 2005; 85: 757–810.
Hoth M, Penner R . Depletion of intracellular calcium stores activates a calcium current in mast cells. Nature 1992; 355: 353–356.
Vanden Abeele F, Skryma R, Shuba Y, Van Coppenolle F, Slomianny C, Roudbaraki M et al. Bcl-2-dependent modulation of Ca(2+) homeostasis and store-operated channels in prostate cancer cells. Cancer Cell 2002; 1: 169–179.
Zhang SL, Yu Y, Roos J, Kozak JA, Deerinck TJ, Ellisman MH et al. STIM1 is a Ca2+ sensor that activates CRAC channels and migrates from the Ca2+ store to the plasma membrane. Nature 2005; 437: 902–905.
Liou J, Kim ML, Heo WD, Jones JT, Myers JW, Ferrell Jr JE et al. STIM is a Ca2+ sensor essential for Ca2+-store-depletion-triggered Ca2+ influx. Curr Biol 2005; 15: 1235–1241.
Feske S, Gwack Y, Prakriya M, Srikanth S, Puppel SH, Tanasa B et al. A mutation in Orai1 causes immune deficiency by abrogating CRAC channel function. Nature 2006; 441: 179–185.
Pedersen SF, Owsianik G, Nilius B . TRP channels: an overview. Cell Calcium 2005; 38: 233–252.
Ramsey IS, Delling M, Clapham DE . An introduction to TRP channels. Annu Rev Physiol 2006; 68: 619–647.
Vanden Abeele F, Lemonnier L, Thebault S, Lepage G, Parys JB, Shuba Y et al. Two types of store-operated Ca2+ channels with different activation modes and molecular origin in LNCaP human prostate cancer epithelial cells. J Biol Chem 2004; 279: 30326–30337.
Vanden Abeele FV, Shuba Y, Roudbaraki M, Lemonnier L, Vanoverberghe K, Mariot P et al. Store-operated Ca(2+) channels in prostate cancer epithelial cells: function, regulation, and role in carcinogenesis. Cell Calcium 2003; 33: 357–373.
Vanden Abeele F, Roudbaraki M, Shuba Y, Skryma R, Prevarskaya N . Store-operated Ca2+ current in prostate cancer epithelial cells. Role of endogenous Ca2+ transporter type 1. J Biol Chem 2003; 278: 15381–15389.
Kahr H, Schindl R, Fritsch R, Heinze B, Hofbauer M, Hack ME et al. CaT1 knock-down strategies fail to affect CRAC channels in mucosal-type mast cells. J Physiol 2004; 557: 121–132.
Peng JB, Chen XZ, Berger UV, Vassilev PM, Tsukaguchi H, Brown EM et al. Molecular cloning and characterization of a channel-like transporter mediating intestinal calcium absorption. J Biol Chem 1999; 274: 22739–22746.
Fixemer T, Wissenbach U, Flockerzi V, Bonkhoff H . Expression of the Ca2+-selective cation channel TRPV6 in human prostate cancer: a novel prognostic marker for tumor progression. Oncogene 2003; 22: 7858–7861.
Peng JB, Zhuang L, Berger UV, Adam RM, Williams BJ, Brown EM et al. CaT1 expression correlates with tumor grade in prostate cancer. Biochem Biophys Res Commun 2001; 282: 729–734.
Wissenbach U, Niemeyer BA, Fixemer T, Schneidewind A, Trost C, Cavalie A et al. Expression of CaT-like, a novel calcium-selective channel, correlates with the malignancy of prostate cancer. J Biol Chem 2001; 276: 19461–19468.
Schwarz EC, Wissenbach U, Niemeyer BA, Strauss B, Philipp SE, Flockerzi V et al. TRPV6 potentiates calcium-dependent cell proliferation. Cell Calcium 2006; 39: 163–173.
Bodding M, Fecher-Trost C, Flockerzi V . Store-operated Ca2+ current and TRPV6 channels in lymph node prostate cancer cells. J Biol Chem 2003; 278: 50872–50879.
Thomas AP, Bird GS, Hajnoczky G, Robb-Gaspers LD, Putney Jr JW . Spatial and temporal aspects of cellular calcium signaling. FASEB J 1996; 10: 1505–1517.
Thebault S, Flourakis M, Vanoverberghe K, Vandermoere F, Roudbaraki M, Lehen'kyi V et al. Differential role of transient receptor potential channels in Ca2+ entry and proliferation of prostate cancer epithelial cells. Cancer Res 2006; 66: 2038–2047.
Kyprianou N, Chon J, Benning CM . Effects of alpha(1)-adrenoceptor (alpha(1)-AR) antagonists on cell proliferation and apoptosis in the prostate: therapeutic implications in prostatic disease. Prostate Suppl 2000; 9: 42–46.
Benning CM, Kyprianou N . Quinazoline-derived alpha1-adrenoceptor antagonists induce prostate cancer cell apoptosis via an alpha1-adrenoceptor-independent action. Cancer Res 2002; 62: 597–602.
Pigozzi D, Ducret T, Tajeddine N, Gala JL, Tombal B, Gailly P . Calcium store contents control the expression of TRPC1, TRPC3 and TRPV6 proteins in LNCaP prostate cancer cell line. Cell Calcium 2006; 39: 401–415.
Vanoverberghe K, Vanden Abeele F, Mariot P, Lepage G, Roudbaraki M, Bonnal JL et al. Ca2+ homeostasis and apoptotic resistance of neuroendocrine-differentiated prostate cancer cells. Cell Death Differ 2004; 11: 321–330.
Prevarskaya N, Skryma R, Shuba Y . Ca2+ homeostasis in apoptotic resistance of prostate cancer cells. Biochem Biophys Res Commun 2004; 322: 1326–1335.
McKemy DD, Neuhausser WM, Julius D . Identification of a cold receptor reveals a general role for TRP channels in thermosensation. Nature 2002; 416: 52–58.
Peier AM, Moqrich A, Hergarden AC, Reeve AJ, Andersson DA, Story GM et al. A TRP channel that senses cold stimuli and menthol. Cell 2002; 108: 705–715.
Tsavaler L, Shapero MH, Morkowski S, Laus R . Trp-p8, a novel prostate-specific gene, is up-regulated in prostate cancer and other malignancies and shares high homology with transient receptor potential calcium channel proteins. Cancer Res 2001; 61: 3760–3769.
Thebault S, Lemonnier L, Bidaux G, Flourakis M, Bavencoffe A, Gordienko D et al. Novel role of cold/menthol-sensitive transient receptor potential melastatine family member 8 (TRPM8) in the activation of store-operated channels in LNCaP human prostate cancer epithelial cells. J Biol Chem 2005; 280: 39423–39435.
Zhang L, Barritt GJ . Evidence that TRPM8 is an androgen-dependent Ca2+ channel required for the survival of prostate cancer cells. Cancer Res 2004; 64: 8365–8373.
Bidaux G, Roudbaraki M, Merle C, Crepin A, Delcourt P, Slomianny C et al. Evidence for specific TRPM8 expression in human prostate secretory epithelial cells: functional androgen receptor requirement. Endocr Relat Cancer 2005; 12: 367–382.
Bonkhoff H, Fixemer T, Remberger K . Relation between Bcl-2, cell proliferation, and the androgen receptor status in prostate tissue and precursors of prostate cancer. Prostate 1998; 34: 251–258.
Bruckheimer EM, Spurgers K, Weigel NL, Logothetis C, McDonnell TJ . Regulation of Bcl-2 expression by dihydrotestosterone in hormone sensitive LNCaP-FGC prostate cancer cells. J Urol 2003; 169: 1553–1557.
Nantermet PV, Xu J, Yu Y, Hodor P, Holder D, Adamski S et al. Identification of genetic pathways activated by the androgen receptor during the induction of proliferation in the ventral prostate gland. J Biol Chem 2004; 279: 1310–1322.
Fuessel S, Sickert D, Meye A, Klenk U, Schmidt U, Schmitz M et al. Multiple tumor marker analyses (PSA, hK2, PSCA, trp-p8) in primary prostate cancers using quantitative RT-PCR. Int J Oncol 2003; 23: 221–228.
Kiessling A, Fussel S, Schmitz M, Stevanovic S, Meye A, Weigle B et al. Identification of an HLA-A*0201-restricted T-cell epitope derived from the prostate cancer-associated protein trp-p8. Prostate 2003; 56: 270–279.
Berges RR, Vukanovic J, Epstein JI, CarMichel M, Cisek L, Johnson DE et al. Implication of cell kinetic changes during the progression of human prostatic cancer. Clin Cancer Res 1995; 1: 473–480.
Henshall SM, Afar DE, Hiller J, Horvath LG, Quinn DI, Rasiah KK et al. Survival analysis of genome-wide gene expression profiles of prostate cancers identifies new prognostic targets of disease relapse. Cancer Res 2003; 63: 4196–4203.
Furst J, Gschwentner M, Ritter M, Botta G, Jakab M, Mayer M et al. Molecular and functional aspects of anionic channels activated during regulatory volume decrease in mammalian cells. Pflugers Arch 2002; 444: 1–25.
Okada Y, Shimizu T, Maeno E, Tanabe S, Wang X, Takahashi N . Volume-sensitive chloride channels involved in apoptotic volume decrease and cell death. J Membr Biol 2006; 209: 21–29.
Shen MR, Yang TP, Tang MJ . A novel function of BCL-2 overexpression in regulatory volume decrease. Enhancing swelling-activated Ca(2+) entry and Cl(−) channel activity. J Biol Chem 2002; 277: 15592–15599.
Lemonnier L, Shuba Y, Crepin A, Roudbaraki M, Slomianny C, Mauroy B et al. Bcl-2-dependent modulation of swelling-activated Cl- current and ClC-3 expression in human prostate cancer epithelial cells. Cancer Res 2004; 64: 4841–4848.
Shuba YM, Prevarskaya N, Lemonnier L, Van Coppenolle F, Kostyuk PG, Mauroy B et al. Volume-regulated chloride conductance in the LNCaP human prostate cancer cell line. Am J Physiol Cell Physiol 2000; 279: C1144–C1154.
Lemonnier L, Prevarskaya N, Shuba Y, Vanden Abeele F, Nilius B, Mazurier J et al. Ca2+ modulation of volume-regulated anion channels: evidence for colocalization with store-operated channels. FASEB J 2002; 16: 222–224.
Lemonnier L, Lazarenko R, Shuba Y, Thebault S, Roudbaraki M, Lepage G et al. Alterations in the regulatory volume decrease (RVD) and swelling-activated Cl− current associated with neuroendocrine differentiation of prostate cancer epithelial cells. Endocr Relat Cancer 2005; 12: 335–349.
Duan D, Winter C, Cowley S, Hume JR, Horowitz B . Molecular identification of a volume-regulated chloride channel. Nature 1997; 390: 417–421.
Acknowledgements
This work was supported by grants from INSERM, the French Minsistry of Education, La Ligue Nationale Contre le Cancer, the Nord/Pas-de-Calais region, and INTAS 05-1000008-8223.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by P Nicotera
Rights and permissions
About this article
Cite this article
Prevarskaya, N., Skryma, R., Bidaux, G. et al. Ion channels in death and differentiation of prostate cancer cells. Cell Death Differ 14, 1295–1304 (2007). https://doi.org/10.1038/sj.cdd.4402162
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4402162
Keywords
This article is cited by
-
The Role οf Ion Channels in the Development and Progression of Prostate Cancer
Molecular Diagnosis & Therapy (2023)
-
Synthesis, Characterization and Employed Doxycycline Capped Gold Nanoparticles on TRP Channel Expressions in SKBR3 Breast Cancer Cells and Antimicrobial Activity
Journal of Cluster Science (2022)
-
Endolysosomal ion channel MCOLN2 (Mucolipin-2) promotes prostate cancer progression via IL-1β/NF-κB pathway
British Journal of Cancer (2021)
-
Modulatory Effect of Selected Dietary Phytochemicals on Delayed Rectifier K+ Current in Human Prostate Cancer Cells
The Journal of Membrane Biology (2019)
-
GABAB receptor regulates proliferation in the high-grade chondrosarcoma cell line OUMS-27 via apoptotic pathways
BMC Cancer (2018)