Abstract
Data sources
Medline, Cochrane Library, Embase, Cinahl and the reference lists of published articles were used to identify relevant studies.
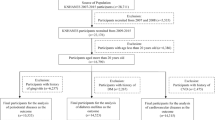
Study selection
Studies were included if the sample sizes were >80 cases, cases were defined as people with fatal or nonfatal coronary artery disease (CAD); described either self-reported periodontal disease (PD) or that diagnosed by clinical assessment of oral health; and provided relative risks (RR) and odds ratios (OR,) or sufficient information for the calculation of RR or OR. Letters, unpublished articles, animal studies, duplicate reports and those providing association between different markers of CAD or particular pathogens involved in PD were excluded.
Data extraction and synthesis
Data was extracted by two investigators using a standard protocol. Cohort studies, case–control studies and cross-sectional studies were analysed separately using the Comprehensive Meta-Analysis software package (version CM 2.2; Biostat, Englewood, New Jersey, USA). Heterogeneity of the studies was assessed using the Cochrane Q test. As the studies were homogeneous the Mantel-Haenszel fixed-effect model was used to compute common RR and OR.
Results
Meta-analysis of the five prospective cohort studies (86 092 patients) found people with PD had a 1.14-fold higher risk of developing coronary heart disease (CHD) than controls [RR, 1.14; 95% confidence interval (CI), 1.07–1.21; P<0.001]. Case–control studies (1423 patients) showed an even greater risk of developing CHD (OR, 2.22; 95% CI, 1.59–3.117; P<0.001). The prevalence of CHD in the cross-sectional studies (17 724 patients) was significantly greater in individuals with PD than in those with no PD (OR, 1.59; 95% CI, 1.33–1.91; P<0.001). Analysing the relationship between number of teeth and incidence of CHD found a 1.24-fold increased risk (95% CI, 1.14–1.36; P<0.0001) of development of CHD in people who had <10 teeth.
Conclusions
This study suggests a possible association between PD and CHD. Elevated levels of inflammatory mediators in people who have PD suggest a role in atherothrombogenesis leading to CHD. Well-designed prospective cohort studies, with uniform definitions of PD and CHD, investigating the role of periodontal pathogen-burden on the occurrence of CHD and the management of patients with PD to reduce the future risk of development of CHD, are necessary.
Similar content being viewed by others
Commentary
Much of the current periodontal literature seems to be focused on the importance of oral health by demonstrating its impact on systemic health. Although we know that the health of the oral cavity is not a separate component of general health, proving an association is difficult. The challenge is that the mechanism underlying chronic diseases such as cardiovascular disease and PD are not completely understood. Thus, we must rely on observational studies in order to draw inferences about the potential effect of a suspected causative factor on the development or progression of a disease. In designing studies to examine the strength of the relationship between oral and systemic diseases, a number of conditions must be met. These include biological plausibility, temporality, specificity and a dose–response gradient.
Scientists are beginning to piece together some of the pieces of this puzzle. Periodontal pathogens have been found in atherosclerotic plaques. Atherothrombogenic mediators such as C-reactive protein are elevated in periodontal disease. Periodontal disease and CAD share many common risk factors including age, smoking, socio-economic status and glycaemic control. Thus the specificity of the association between the two is not clear cut. There is some evidence of a dose–response gradient. For example, the findings of this meta-analysis suggest the risk of CAD may be related to the number of remaining teeth (tooth loss being the ultimate outcome of untreated PD).
Bahekar and colleagues have produced a high-quality systematic review. It is both methodologically and statistically sound. Only studies that had adjusted for confounding variables known to contribute to CAD were included in the meta-analysis. The more robust statistic of RR (versus OR) was used where appropriate. Unlike previous systematic reviews and meta-analyses, they also analysed cohort, case–control and cross-sectional studies separately. This provides an excellent example of how evidence from lower quality trials can overestimate effect. Nonetheless, the findings reflect those of earlier systematic reviews: that PD may contribute to the risk of CAD. The mechanism underlying the association between periodontal infection and CAD remains unclear.
The authors point out several weaknesses in the current literature. The most glaring is the lack of a standardised protocol to determine PD and CAD. Some studies used self-report, which probably under-reports levels of disease, whereas others included gingivitis and periodontitis, which would overestimate disease prevalence. In reality, these studies are not comparing similar predictor variables. The research community needs to address this issue and develop consensus so that results from future meta-analyses have some weight.
Practice point
This review adds strength to the hypothesis that PD is a risk factor for CAD. Given the high mortality rate of cardiovascular diseases, and the relatively minor morbidity of periodontal therapy, maintenance of periodontal health should be among the recommendations for prevention of heart disease.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Amol Ashok Bahekar, Department of Cardiology, Chicago Medical School — North Chicago Veterans Affairs Medical Center, 3001 Green Bay Road, North Chicago IL 60064, USA. E-mail: abaheker@yahoo.com.
Bahekar AA, Singh S, Saha S, Molnar J, Arora R. The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am Heart J 2007; 154:830–837.
Rights and permissions
About this article
Cite this article
Matthews, D. Possible link between periodontal disease and coronary heart disease. Evid Based Dent 9, 8 (2008). https://doi.org/10.1038/sj.ebd.6400560
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400560
This article is cited by
-
Relationship between the burden of major periodontal bacteria and serum lipid profile in a cross-sectional Japanese study
BMC Oral Health (2018)
-
Access to special care dentistry, part 8. Special care dentistry services: seamless care for people in their middle years – part 2
British Dental Journal (2008)
-
Studies suggest an association between maternal periodontal disease and pre-eclampsia
Evidence-Based Dentistry (2008)