Abstract
Interleukin-1 (IL1) is a potent endogenous pyrogen and inducer of the acute phase response, and these innate immune responses are an important part of the human host's initial reaction to infection by the malaria parasite. In addition, several single-nucleotide polymorphisms (SNPs) in this region have previously been demonstrated to be associated with susceptibility to infectious disease. Therefore, a possible association with malaria susceptibility was investigated. A total of 13 polymorphic markers were used in a two-stage screening strategy to genotype a Gambian case–control study group by either restriction endonuclease digestion or the Sequenom MassARRAY™ assay. This involved an initial screen of 188 severe cases and 188 mild controls, and if there was a significant association with a malaria phenotype (P<0.05); this was followed by screening of the remaining 1044 samples. Two markers showed significant association with malaria: interleukin-1 alpha +4845 G → T (P=0.035 for mild malaria versus controls) and interleukin-1 beta +3953 C → T (P=0.030 for mild malaria versus severe malaria). Haplotypes constructed using the SNPHAP programme were not associated with any of the malaria phenotypes investigated. In summary, if IL1 variants are involved in malaria susceptibility in the Gambia at all, then the effects are small.
Similar content being viewed by others
Introduction
Malaria is a major health problem affecting hundreds of millions of people in sub-Saharan Africa. A meta-analysis of mortality and morbidity data resulted in an estimate that over 200 million clinical attacks of malaria occurred in 1995 in people resident in malaria-endemic regions, with nearly 1 million deaths directly attributable to malaria.1 With the emergence of antimalarial drug-resistant strains of Plasmodium falciparum2 and mosquitoes resistant to pyrethroid insecticides,3 the need to identify human genes that are involved in susceptibility to, or protection from, malaria has never been more pressing.
Genetic association studies utilising polymorphic markers in candidate genes have been successful in identifying a number of genes that are associated with susceptibility to malaria, or cerebral malaria. These include haemoglobin,4,5 tumour necrosis factor-alpha (TNFA),6 CD36,7 nitric oxide synthase-28 and the interferon-α receptor 1.9 Family-based studies have also demonstrated significant linkage to regions of the genome containing genes of interest such as MHC10 and cytokines.11
Increasing knowledge of host–parasite interactions has provided insights into the pathogenesis of malaria and hence the identification of new candidate genes. Interleukin-1 (IL1) is a potent endogenous pyrogen and inducer of the acute phase response,12 and these innate immune responses are an important part of the human host's initial reaction to infection by the malaria parasite. TNFA is also an endogenous pyrogen and variants of this gene have been associated with cerebral malaria,6,13,14 suggesting that functionally similar molecules, such as IL1, are good candidate genes for susceptibility to malaria.
IL1 is encoded by two separate genes, interleukin-1 alpha (IL1A) and interleukin-1 beta (IL1B) located at chromosomal band 2q14 in a cluster that also contains the genes for the IL1 receptors type 1 and 2 (IL1R1 and IL1R2), the IL1 receptor antagonist (IL1RN) and at least six other less well-characterised homologues, the interleukin-1 family members 5–10 (see, Dunn et al15, for review). IL1A, IL1B and IL1RN proteins are not closely related at the level of the primary amino-acid sequence, with 22 and 26% homology to IL1B for IL1A and IL1RN, respectively. However, they are all ligands for IL1R1 and show significant three-dimensional homology, each one consisting of a single structural domain formed from 12 beta strands, arranged in a beta-trefoil structure. IL1A and IL1B bind to the IL1R1, in conjunction with the IL1 receptor accessory protein, initiating a signalling cascade resulting in nuclear factor-kappa B activation. IL1RN binds to IL1R1, preventing IL1 binding, blocking the signalling pathway and downregulating the response to the IL1 signal (see, Hanada and Yoshimura16, for review).
Genetic association of IL1A, B and RN gene variants to infectious and autoimmune disease has been demonstrated in a large number of studies. An IL1A single-nucleotide polymorphism (SNP), IL1A −889 C to T, has been associated with myasthenia gravis,17 sarcoidosis,18 age of onset of migraine19 and juvenile rheumatoid arthritis.20 Two SNPs in IL1B have reported genetic associations with disease. IL1B −511 C to T has been associated with gastric cancer,21 Parkinson's disease,22 asthma,23 increased risk of febrile seizures24 and inflammatory bowel disease,25 while IL1B +3953 C to T has been associated with periodontitis26 and inflammatory bowel disease.25 An 86 bp repeat in the IL1RN gene has also been associated with a number of clinical conditions, including ankylosing spondylitis,27 susceptibility to sepsis,28,29 increased risk of death due to sepsis,30 increased risk of febrile seizures31 and susceptibility to tuberculosis.32
One of the major factors contributing to mortality due to malaria infection is cerebral complications. It has been previously demonstrated in experimental animal models that IL1 is produced in response to cerebral injury (see, Touzani et al33, for review) and that antagonising IL1 activity reduces the brain damage occurring after physical or ischaemic insult.34,35 Since sequestration of infected red blood cells in the cerebral microvasculature occurs during malaria infection, it has been proposed that one mechanism for the brain pathology observed in cerebral malaria may be obstruction of blood flow and localised ischaemia. This suggests the possibility that if a polymorphism in the IL1 gene reduces its biological activity or expression, it may lead to a reduction in this damaging inflammatory response to ischaemia.
The objective of this study was to assess, in a Gambian case–control sample of 1420 individuals, possible association of polymorphic markers in the IL1 gene cluster with susceptibility to malaria and development of severe anaemia and cerebral malaria.
Materials and methods
The details of this case–control study have been described previously.4
Screening strategy
A two-stage screening strategy was adopted. A set of DNA samples was screened initially, containing 188 severe malaria samples and 188 mild nonmalaria controls. If statistically significant association could be demonstrated for a marker using these extremes of phenotype, then the whole set of DNA samples were screened using that polymorphic marker and the data reanalysed as a whole (total of 528 severe malaria samples, 338 mild malaria samples and 554 controls).
Sample typing
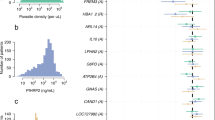
A total of 13 polymorphic markers were studied, chosen on the basis of previous associations in the literature and availability of data from online databases. Eight were SNPs, four were dinucleotide repeat microsatellite markers and one was a variable number of tandem repeats (VNTR) marker (Figure 1). For the IL1B −511 and 1903 SNPs and the microsatellite markers, PCR was performed in a 15 μl reaction mixture containing 50 ng of genomic DNA, 10 mM Tris-HCl, 50 mM KCl, pH 8.3 (GeneAmp 10 × Buffer II, Perkin-Elmer), 1.0–3.0 mM MgCl2, 50–200 μ M of each dNTP, 0.5–0.75 U AmpliTaq Gold DNA polymerase (Perkin-Elmer) and 0.2–0.33 μ M each of forward and reverse primers (Sigma-Genosys Ltd). Amplification reactions were performed using an MJ Research tetrad thermal cycler as follows: 94°C for 15 min, 35–39 cycles (94°C for 30 s, 53–63°C for 45 s, 72°C for 60 s) and finally 72°C for 10 min. For the microsatellite markers, one of each primer pair was fluorescently labelled using FAM, HEX (Sigma-Genosys Ltd) or NED (Applied Biosystems), and PCR products were analysed on an ABI 3700 sequencer (Applied Biosystems).
The IL1 gene cluster (genes are denoted by filled boxes. Abbreviations are as follows: IL1R1=interleukin-1 receptor type 1, IL1A=interleukin-1 alpha, IL1B=interleukin-1 beta and IL1RN=interleukin-1 receptor antagonist, kb=kilobases. Distances are obtained from the UCSC Golden Path Genome browser, December 2002 build).
For the IL1B −511 SNP, genotyping was carried out by Ligase Detection Reaction (LDR).36 The allele-specific oligonucleotide probe pairs were distinguished both by different fluorescent labels (FAM/HEX or FAM/TET) and their length in bases. LDR reactions were performed in a final volume of 15 μl containing 20 mM Tris-HCl, 25 mM potassium acetate, 10 mM magnesium acetate, 10 mM DTT, 1 mM NAD, 0.1% Triton X-100, pH 7.6 (Taq DNA Ligase Buffer, New England Biolabs, USA), 10 nM of 5′-phosphorylated common probe, 10 nM of each allelic probe, 2 μl of Proteinase K-treated PCR product and 4 U of Taq DNA Ligase (New England Biolabs). The LDR reactions were cycled as follows: 95°C for 1 min followed by 15 cycles of 95°C for 15 s, 54–72°C for 4 min. LDR reactions were stopped by the addition of 3 μl of 100 mM EDTA pH 8.0, and LDR products were analysed using an ABI 3700 sequencer (Applied Biosystems).
For the IL1b 1903 SNP, the PCR product was digested using the restriction endonuclease AluI (New England Biolabs, USA) as recommended by the supplier. Digestion products were then size separated by electrophoresis on a 2% (w/v) agarose gel containing ethidium bromide and photographed using a Stratagene Eagle Eye capture system.
For the other SNPs in IL1A and Il1B, genotyping was performed using the Sequenom MassARRAY™ (Sequenom Inc., San Diego, USA) MALDI-TOF system. PCR was performed as follows: 0.5 μl of 10 × Qiagen HotStarTaq PCR Buffer, 0.2 μl 25 mM MgCl2, 0.05 μl 8 mM dNTP mix, 0.25 μl of each 1 μ M PCR primer, 0.1 U Qiagen HotStarTaq polymerase, 1 μl of 2.5 ng/μl genomic DNA and water to a final volume of 5 μl. PCR cycling was carried out in an ABgene 384-well plate using an MJ tetrad thermal cycler. Thermal cycling conditions were as follows: 95°C for 15 min, 45 cycles (94°C for 20 s, 56°C for 30 s, 72°C for 60 s) and finally 72°C for 3 min. The Sequenom MassEXTEND reaction was then carried out using the conditions described on http://www.well.ox.ac.uk/core-genotyping/sequenom/sequenom.shtml.
Statistical analysis
Initially, SNP markers were analysed individually. Data were analysed using a Pearson's 3 × 2 χ2 test for the overall difference in genotype frequencies between malaria cases and controls. Microsatellite markers were analysed by inspecting allele frequencies and carrying out a Fisher's exact χ2 test on each allele where there was an apparent difference between cases and controls. Haplotype construction was performed using the SNPHAP programme (see http://www-gene.cimr.cam.ac.uk/clayton/software/), which is designed for haplotype estimation from SNP marker data derived from case–control study groups. Linkage disequilibrium (LD) was visualised using the GOLD programme.37
Results
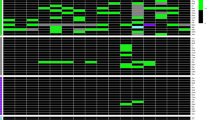
The results of the screening for association between the polymorphic markers and malaria are shown in Table 1 and Figure 2. Utilising the two-stage screening strategy, all markers were typed using the first-stage 376 samples. On analysis of the first-stage screen, several markers were associated with malaria at P-values lower than P=0.1 (data not shown). The remaining samples were then typed using these markers. The highest frequency allele of the IL1R1 microsatellite marker was significantly associated (P<0.05) in the initial screen with susceptibility to malaria, but when the whole set was genotyped this association became nonsignificant. None of the other microsatellite alleles were significantly associated with malaria in the initial screen. The IL1A +4845 SNP was bordering on statistical significance in the initial screen, but the association with severe malaria was not significant in the full set. Significant association was observed between mild malaria and controls (P=0.035), and mild malaria and severe malaria cases (P=0.042). Two of the SNPs in IL1A, rs1801715 and rs17562 (dbSNP reference numbers), were non-polymorphic in the initial screening set.
Allele distributions of the five non-SNP markers genotyped (key to shading: black=severe malaria; grey=mild malaria; white=control. Markers are IL1RN VNTR (N=492 severe malaria/339 mild malaria/550 controls), D2S1895 (N=158 severe malaria/155 nonmalaria), D2S2269 (N=180 severe malaria/178 nonmalaria), IL1R1 (N=451 severe malaria/301 mild malaria/512 nonmalaria) and IL1A 222/223 (N=185 severe malaria/184 nonmalaria)).
The analysis of association with the severe malaria phenotypes of severe anaemia and cerebral malaria was also carried out. With the reduction in numbers of subjects involved in analysing these severe malaria phenotypes only the biallelic SNP markers were included in the analysis (data not shown). For severe anaemia, no significant associations were detected. For cerebral malaria, only one association was detected to the IL1B +3953 TaqI SNP where the rare allele was significantly associated with cerebral malaria (P=0.030) when the allele frequencies were compared using a 2 × 2 χ2 test.
SNP haplotypes were constructed using the IL1A and IL1B SNPs with the SNPHAP programme. SNPHAP 1.0 is freely available from http://www-gene.cimr.cam.ac.uk/clayton/software/ and it performed equally well or better than PHASE,38 with test data (results not shown). SNPHAP was the programme of choice by virtue of its ease of use and short analysis times compared to PHASE. The microsatellite data were not used in order to minimise the total number of haplotypes analysed and maximise the power to detect association. Samples with missing genotypes due to PCR failure were removed prior to haplotype construction. Using GOLD to construct a LD map demonstrated that in the Gambian subjects, the SNPs in IL1A and IL1B were not in significant LD, in spite of the relatively short physical distance between them of 48 kb. The analysis of the LD across the IL1B gene also demonstrated that the IL1B +3953 C to T (TaqI) SNP was not in LD with the other three IL1B SNPs (−511, −31 and 1903 (AluI)) (data not shown). None of the derived haplotypes of the linked SNPs in either IL1A or IL1B were significantly associated with disease (data not shown).
Discussion
The IL1 gene cluster contains the IL1A and IL1B genes, which are among the most potent immunostimulatory proteins known. With their prominent roles in the acute phase response, variants of these genes, the IL1 receptor type 1 and the receptor antagonist molecule might be associated with autoimmune and infectious disease susceptibility, and this is indeed the case for conditions such as septic shock,28,29 ankylosing spondylitis,27 juvenile rheumatoid arthritis20 and myasthenia gravis.17 Malaria pathogenesis might also be expected to be affected by variation in these genes for the same reason. Since IL1 may also have a role to play in exacerbating inflammatory damage following an ischaemic event in the brain and since sequestration of malaria parasites in the cerebral microvasculature may cause ischaemia, variants of IL1 may also be associated with cerebral malaria.
The current study is the first to analyse multiple polymorphic markers in the IL1 gene cluster for association with malaria and related phenotypes. The study consisted of a group of 1420 Gambians who were genotyped using 13 polymorphic markers located within a 1.4 Mb region containing the IL1 gene cluster. For the IL1A +4845 SNP, the genotype frequencies were significantly different between mild malaria cases and controls (P=0.035) or severe malaria cases (P=0.042), suggesting that the variant or a variant in LD with it, might predispose to malaria but actually be protective for severe symptoms.
The IL1B +3953 SNP also showed a similar significant difference between the genotype frequencies for mild malaria and severe malaria cases (P=0.030). The difference between severe malaria cases and controls is only just nonsignificant (P=0.087), suggesting that this may possibly be a predisposing allele for severe malaria of small effect. No significant association to severe anaemia or cerebral malaria was observed for the six SNPs in the IL1A and IL1B genes, but there was one significant association between the IL1B +3953 C to T SNP allele frequency and cerebral malaria (P=0.030). The IL1B +3953 C to T SNP was not in LD with other SNPs in the gene, so it is possible that this effect is due to another more strongly associated SNP that has yet to be identified.
There is currently only one reported genetic association between an IL1B polymorphism and a malaria-associated phenotype.39 The reported association was between parasitaemia in uncomplicated malaria cases in Ghana and carriage of the IL1B +3953T allele. The analysis of parasitaemia on admission for the mild malaria cases in the Gambia demonstrated no significant association (P=0.965). However, it is worth noting that carriage of the T allele in the mild malaria groups is at a much lower frequency in our Gambian study group compared to the Ghanaian group (23.4 versus 40.2%).
It is worth noting that the Sequenom MassARRAY system (see, Jurinke et al40, for a recent review) produced similar high-quality results to the restriction digestion analysis of PCR products. The IL1B +3953 C to T SNP was typed using the restriction enzyme TaqI in the initial set and then the whole set of samples using the Sequenom system. The Sequenom assay gave complete agreement with all but one sample and this was due to an error in the manual entry of the restriction digest results (data not shown). This validated the data produced by the Sequenom system as of comparable quality to other established techniques and improves on them by being both high throughput and requiring less manual involvement, with a concomitant reduction in the potential for errors in data input. The introduction of pooling genomic DNA41 will increase the throughput further and make very large-scale studies achievable.
In summary, although the IL1 gene cluster contains several genes that can be put forward as likely candidates for association with malaria, these results demonstrate that if there is a genetic effect it is small, since it is barely significant in a screen involving over 1400 individuals. In addition, although it is not clear how to correct for the effect of multiple testing when the tests use related phenotypes and genetic markers in LD with each other, if the Bonferroni correction is applied to this data then there are no significant results (P⩽0.05). However, screening of further case–control groups would be useful to explore whether IL1 variants are involved in malaria susceptibility in other sub-Saharan African populations. In addition, an appropriately designed family study may provide useful linkage information, have more power to detect association and allow haplotypes to be constructed with more confidence.
References
Snow RW, Craig MH, Deichmann U, le Sueur D : A preliminary continental risk map for malaria mortality among African children. Parasitol Today 1999; 15: 99–104.
Wongsrichanalai C, Pickard AL, Wernsdorfer WH, Meshnick SR : Epidemiology of drug-resistant malaria. Lancet Infect Dis 2002; 2: 209–218.
Hougard JM, Fontenille D, Chandre F, Darriet F, Carnevale P, Guillet P : Combating malaria vectors in Africa: current directions of research. Trends Parasitol 2002; 18: 283–286.
Hill AV, Allsopp CE, Kwiatkowski D et al: Common west African HLA antigens are associated with protection from severe malaria. Nature 1991; 352: 595–600.
Modiano D, Luoni G, Sirima BS et al: Haemoglobin C protects against clinical Plasmodium falciparum malaria. Nature 2001; 414: 305–308.
McGuire W, Hill AV, Allsopp CE, Greenwood BM, Kwiatkowski D : Variation in the TNF-alpha promoter region associated with susceptibility to cerebral malaria. Nature 1994; 371: 508–510.
Aitman TJ, Cooper LD, Norsworthy PJ et al: Malaria susceptibility and CD36 mutation. Nature 2000; 405: 1015–1016.
Kun JF, Mordmuller B, Lell B, Lehman LG, Luckner D, Kremsner PG : Polymorphism in promoter region of inducible nitric oxide synthase gene and protection against malaria. Lancet 1998; 351: 265–266.
Aucan C, Walley AJ, Hennig BJW et al: Interferon-alpha receptor-1 (IFNAR1) variants are associated with protection against cerebral malaria in The Gambia. Genes Immun 2003; 4: 275–282.
Jepson A, Sisay-Joof F, Banya W et al: Genetic linkage of mild malaria to the major histocompatibility complex in Gambian children: study of affected sibling pairs. BMJ 1997; 315: 96–97.
Rihet P, Traore Y, Abel L, Aucan C, Traore-Leroux T, Fumoux F : Malaria in humans: Plasmodium falciparum blood infection levels are linked to chromosome 5q31–q33. Am J Hum Genet 1998; 63: 498–505.
Merriman CR, Pulliam LA, Kampschmidt RF : Comparison of leukocytic pyrogen and leukocytic endogenous mediator. Proc Soc Exp Biol Med 1977; 154: 224–227.
Knight JC, Udalova I, Hill AV et al: A polymorphism that affects OCT-1 binding to the TNF promoter region is associated with severe malaria. Nat Genet 1999; 22: 145–150.
Stirnadel HA, Stockle M, Felger I, Smith T, Tanner M, Beck HP : Malaria infection and morbidity in infants in relation to genetic polymorphisms in Tanzania. Trop Med Int Health 1999; 4: 187–193.
Dunn E, Sims JE, Nicklin MJ, O'Neill LA : Annotating genes with potential roles in the immune system: six new members of the IL-1 family. Trends Immunol 2001; 22: 533–536.
Hanada T, Yoshimura A : Regulation of cytokine signaling and inflammation. Cytokine Growth Factor Rev 2002; 13: 413–421.
Sciacca FL, Ferri C, Veglia F et al: IL-1 genes in myasthenia gravis: IL-1A −889 polymorphism associated with sex and age of disease onset. J Neuroimmunol 2002; 122: 94–99.
Hutyrova B, Pantelidis P, Drabek J et al: Interleukin-1 gene cluster polymorphisms in sarcoidosis and idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2002; 165: 148–151.
Rainero I, Pinessi L, Salani G et al: A polymorphism in the interleukin-1alpha gene influences the clinical features of migraine. Headache 2002; 42: 337–340.
McDowell TL, Symons JA, Ploski R, Forre O, Duff GW : A genetic association between juvenile rheumatoid arthritis and a novel interleukin-1 alpha polymorphism. Arthritis Rheum 1995; 38: 221–228.
Machado JC, Pharoah P, Sousa S et al: Interleukin 1B and interleukin 1RN polymorphisms are associated with increased risk of gastric carcinoma. Gastroenterology 2001; 121: 823–829.
Schulte T, Schols L, Muller T, Woitalla D, Berger K, Kruger R : Polymorphisms in the interleukin-1 alpha and beta genes and the risk for Parkinson's disease. Neurosci Lett 2002; 326: 70–72.
Karjalainen J, Nieminen MM, Aromaa A, Klaukka T, Hurme M : The IL-1beta genotype carries asthma susceptibility only in men. J Allergy Clin Immunol 2002; 109: 514–516.
Virta M, Hurme M, Helminen M : Increased frequency of interleukin-1beta (−511) allele 2 in febrile seizures. Pediatr Neurol 2002; 26: 192–195.
Nemetz A, Kope A, Molnar T et al: Significant differences in the interleukin-1beta and interleukin-1 receptor antagonist gene polymorphisms in a Hungarian population with inflammatory bowel disease. Scand J Gastroenterol 1999; 34: 175–179.
McDevitt MJ, Wang HY, Knobelman C et al: Interleukin-1 genetic association with periodontitis in clinical practice. J Periodontol 2000; 71: 156–163.
McGarry F, Neilly J, Anderson N, Sturrock R, Field M : A polymorphism within the interleukin 1 receptor antagonist (IL-1Ra) gene is associated with ankylosing spondylitis. Rheumatology (Oxford) 2001; 40: 1359–1364.
Fang XM, Schroder S, Hoeft A, Stuber F : Comparison of two polymorphisms of the interleukin-1 gene family: interleukin-1 receptor antagonist polymorphism contributes to susceptibility to severe sepsis. Crit Care Med 1999; 27: 1330–1334.
Ma P, Chen D, Pan J, Du B : Genomic polymorphism within interleukin-1 family cytokines influences the outcome of septic patients. Crit Care Med 2002; 30: 1046–1050.
Arnalich F, Lopez-Maderuelo D, Codoceo R et al: Interleukin-1 receptor antagonist gene polymorphism and mortality in patients with severe sepsis. Clin Exp Immunol 2002; 127: 331–336.
Tsai FJ, Hsieh YY, Chang CC, Lin CC, Tsai CH : Polymorphisms for interleukin 1 beta exon 5 and interleukin 1 receptor antagonist in Taiwanese children with febrile convulsions. Arch Pediatr Adolesc Med 2002; 156: 545–548.
Bellamy R, Ruwende C, Corrah T, McAdam KP, Whittle HC, Hill AV : Assessment of the interleukin 1 gene cluster and other candidate gene polymorphisms in host susceptibility to tuberculosis. Tuberc Lung Dis 1998; 79: 83–89.
Touzani O, Boutin H, Chuquet J, Rothwell N : Potential mechanisms of interleukin-1 involvement in cerebral ischaemia. J Neuroimmunol 1999; 100: 203–215.
Loddick SA, Rothwell NJ : Neuroprotective effects of human recombinant interleukin-1 receptor antagonist in focal cerebral ischaemia in the rat. J Cereb Blood Flow Metab 1996; 16: 932–940.
Touzani O, Boutin H, LeFeuvre R et al: Interleukin-1 influences ischemic brain damage in the mouse independently of the interleukin-1 type I receptor. J Neurosci 2002; 22: 38–43.
Day DJ, Speiser PW, Schulze E et al: Identification of non-amplifying CYP21 genes when using PCR-based diagnosis of 21-hydroxylase deficiency in congenital adrenal hyperplasia (CAH) affected pedigrees. Hum Mol Genet 1996; 5: 2039–2048.
Abecasis GR, Cookson WO : GOLD – graphical overview of linkage disequilibrium. Bioinformatics 2000; 16: 182–183.
Stephens M, Smith NJ, Donnelly P : A new statistical method for haplotype reconstruction from population data. Am J Hum Genet 2001; 68: 978–989.
Gyan B, Goka B, Cvetkovic JT et al: Polymorphisms in interleukin-1beta and interleukin-1 receptor antagonist genes and malaria in Ghanaian children. Scand J Immunol 2002; 56: 619–622.
Jurinke C, van den Boom D, Cantor CR, Koster H : The use of MassARRAY technology for high throughput genotyping. Adv Biochem Eng Biotechnol 2002; 77: 57–74.
Werner M, Sych M, Herbon N, Illig T, Konig IR, Wjst M : Large-scale determination of SNP allele frequencies in DNA pools using MALDI-TOF mass spectrometry. Hum Mutat 2002; 20: 57–64.
Acknowledgements
This work was funded by the Wellcome Trust. AVSH is a Wellcome Trust Principal Research Fellow. We would like to thank the many investigators involved in the original case–control study in the Gambia for their contributions. AW and CA would also like to thank Dr Ioannis Ragoussis and his group, especially Mr Aaron Abbott, for their continuing advice and support and for carrying out the assay stage of the Sequenom genotyping.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walley, A., Aucan, C., Kwiatkowski, D. et al. Interleukin-1 gene cluster polymorphisms and susceptibility to clinical malaria in a Gambian case–control study. Eur J Hum Genet 12, 132–138 (2004). https://doi.org/10.1038/sj.ejhg.5201084
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201084
Keywords
This article is cited by
-
Risk score prediction model based on single nucleotide polymorphism for predicting malaria: a machine learning approach
BMC Bioinformatics (2022)
-
Leveraging Mann–Whitney U test on large-scale genetic variation data for analysing malaria genetic markers
Malaria Journal (2022)
-
Host genetic polymorphisms and serological response against malaria in a selected population in Sri Lanka
Malaria Journal (2018)
-
IL1B, IL4R, IL12RB1 and TNF gene polymorphisms are associated with Plasmodium vivax malaria in Brazil
Malaria Journal (2012)
-
Variation in human genes encoding adhesion and proinflammatory molecules are associated with severe malaria in the Vietnamese
Genes & Immunity (2012)