Abstract
Aims To estimate the prevalence of low bone density and osteoporosis in a population of patients with uveitis taking systemic steroid treatment; to clarify the risks of steroid-induced fracture and to suggest a protocol for the prevention and management of bone loss in patients with ophthalmic inflammatory disease.
Methods Bone densitometry was performed on 129 adult patients with prednisolone-treated uveitis from four centres. Information on uveitis diagnosis, associated risk factors, steroid dosage and treatment duration, prophylaxis and management, was collected. Juveniles, patients with scleritis and those who had used deflazacort, were excluded.
Results Steroid treatment time varied from 13 weeks to 31 years, and the total dosage from 1.29 g to 166.5 g. Twenty-six percent of patients also used one or more immunosuppressives. Forty-eight percent had additional risk factors for bone loss. Bone density was abnormally low in 44.2%, and 15.5% had osteoporosis. Osteoporosis was substantially more common in males (20.6%, all under 60 yrs) than in females (9.8%). Seven symptomatic fractures occurred in patients on treatment. Bone loss correlated with total steroid dose, mean dose, duration of treatment and the presence of pre-existing risk factors.
Conclusions The prevalence of steroid-induced osteoporosis and fracture is low for patients with uveitis but young males are at risk. Patients at high risk should be identified, and prophylaxis and treatment should be used as required. The guideline of the National Osteoporosis Society is recommended as a management protocol.
Similar content being viewed by others
Introduction
Osteoporosis is a reduction in bone density which increases its fragility and therefore the risk of fracture. Bone density can be quantified by a variety of methods, and is usually expressed either as a variation from a sex and age-matched mean (Z-score) or from an optimal, sex-matched young adult mean (T-score). If the bone density is worse than one standard deviation below an optimal mean (T-score <−1.0), the term osteopenia is used; if the T-score is <−2.5, the patient has osteoporosis. If an osteoporotic person has already suffered a fracture, the term established osteoporosis is used. Osteoporosis may be primary (age- and/or sex-related) or secondary to a variety of other factors; the most common of these is systemic steroid therapy.
Ophthalmologists use systemic steroid treatment regularly, to treat intraocular and orbital inflammatory disease, scleritis, optic neuritis and thyroid eye disease. A 1997 survey of consultant ophthalmologists1 showed that three quarters prescribed steroids in significant doses but that only 25% of these gave advice to patients on the prevention of osteoporosis. A 1999 study in general practice2 showed that only 14% of steroid users were prescribed prophylactic treatment against bone loss. Although the literature on steroid-induced osteoporosis is now extensive, it has been largely confined to the rheumatological and specialist medical literature. Two informative papers on the side-effects of steroids have been produced, by Stanbury & Graham3 and by Jabs et al,4 but information on osteoporosis has not been readily accessible to the ophthalmological community.
Systemic steroid therapy is most frequently used by ophthalmologists to treat uveitis. Although steroid-induced bone loss in some diseases has been well-documented, it is clear that there is an intrinsic risk of osteoporosis in those diseases most studied, including inflammatory arthropathies, asthma and inflammatory bowel disease. It may be unjustified to extrapolate the perceived risks to a population of uveitis patients, particularly those without associated systemic disease. No previous study has examined bone loss in any population of ophthalmic patients. We therefore retrospectively evaluated bone density in steroid-treated patients attending uveitis clinics in order to quantify bone loss in these patients, and suggest an approach to the prevention or minimisation of this potentially serious complication.
Patients and methods
From an adult population of patients attending the Uveitis Clinics at the Manchester Royal Eye Hospital, St Thomas’ Hospital, Birmingham & Midland Eye Centre and Moorfields Eye Hospital, those using systemic prednisolone for 3 months or longer who had undergone bone densitometry, were identified. Data were retrieved from medical records including age, sex, race and diagnosis.
Bone density was assessed using dual-emission X-ray absorptiometry (DEXA) of lumbar spine and proximal femur (Figure 1). Patients were categorised as normal (T-score −1.0 or better), osteopenia (T-score −2.5 ≤ −1.0) or osteoporosis (T-score < −2.5).
Detailed information on steroid usage was noted for the entire duration of treatment up to the date of DEXA. From these data the total duration of steroid treatment between commencement and DEXA, total dose and mean daily dose were calculated. The coexistence of other risk factors for osteoporosis was noted, as was the use of prophylaxis, if any, against bone loss. Patients were excluded if steroids had been used at any time under the age of 16 years, if data were incomplete, if they had scleritis, or if they had used deflazacort. If intravenous or depot intramuscular methylprednisolone or other immunosuppressive treatment had been used, such events were noted.
Results
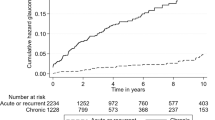
One hundred and twenty-nine patients were included in the study, of whom 68 (53%) were male and 61 (47%) female. One hundred and nine (84.5%) were Caucasian, six (4.6%) black and 14 from other racial groups. The age at densitometry ranged from 19 to 88, and the age distribution for both sexes is shown in Figure 2a and b. The causes of uveitis where known, or the main manifestations of inflammation, are shown in Table 1.
Treatment time varied from 13 weeks to 31 years (mean 3.6 years). The cumulative dose ranged from 1290 mg to 166 559 mg (mean 16849 mg) and the mean dose ranged from 2.8 mg/day to 41 mg/day (mean 13.6 mg/day).
At some time during treatment a total of 34 patients (26.4%) also received treatment with immunosuppressives (up to three drugs) as steroid-sparing or preferred medication. The drugs involved are shown in Table 2. In addition, eight patients received intramuscular depot injections and four patients intravenous pulses, of methylprednisolone.
A total of 62 patients (48%) had one to four potential risk factors for osteoporosis prior to the commencement of steroid treatment, as shown in Table 3. Seventeen patients (13.2%) used prophylaxis against bone loss; 12 with Calcium ± Vitamin D3; four with hormone replacement therapy (HRT) and one with both of these.
Bone densitometry was within the normal range in 72 patients (55.8%) but was low in the remainder, 37 (28.7%) having osteopenia and 20 (15.5%) osteoporosis. Of the 20 osteoporotics, 14 were male and six female. Comparing these two groups, pre-existing risk factors were identified in 6/6 osteoporotic women and 9/14 men; the mean steroid dose was 13.6 mg/day for men, but 18.9 mg/day for women. The total steroid dose was 30.1 g for men compared to 20.4 g for women; the mean treatment duration was 6.4 yrs for osteoporotic men, but 4 yrs for women. None of these treatment parameters were significantly different between males and females.
Overall 57 patients (44.2%) had low bone density; in 32 of these cases the maximally-affected site was specified in the densitometry report; in 23 of these the lower spine was most affected, and the hip in nine. Eight symptomatic fractures occurred in seven patients (five men, two women) during steroid treatment; three had normal bone densitometry, one had osteopenia and three had (established) osteoporosis.
Discussion
Systemic steroid treatment induces bone loss in several ways; doses greater than 10 mg/day inhibit dietary calcium absorption; suppression of androgen production depresses oestrone levels and suppresses the calcitonin response, leading to increased bone reabsorption; osteoclasis is stimulated; and bone formation is reduced. Bone loss is inevitable during steroid therapy and commences within days of starting treatment. The rate of loss is greatest within the first 6 months, during which time typically 4–5% of bone is lost.5 Eventually osteoporosis occurs in up to 50% of patients.6 Trabecular bone is particularly affected, so effects are more marked in the spine (where steroid treatment is responsible for up to 20% of all crush fractures7) and proximal femur. Overall, the prevalence of symptomatic or asymptomatic fractures in patients treated with systemic steroids is between 11 and 20%;8 this represents a 2.5–3 times increased risk of fracture compared with a control population.9
Bone density may be assessed by plain radiography, quantitative computed tomography, ultrasonography or absorptiometry using photons or X-rays.10 DEXA scanning is now the most widely available technique in the UK and was used in this study. It is rapid, taking less than 5 min per site, uses little radiation (less than 1 μSv for a spine scan) and is relatively inexpensive. There are problems of reproducibility in any method of bone densitometry, between machines and longitudinally in a single patient. Data should therefore be interpreted within these limitations, and it should be noted that DEXA assessments in this series were made on at least four different machines.
Our study of 129 patients has shown a high incidence of bone loss but a low incidence of fracture. The presence of pre-existing risk factors correlated strongly with bone loss (Table 4). There was also a trend towards higher total steroid dose (normal = 14.8 g, osteoporosis = 27.2 g), mean steroid dose (normal 13.6 mg, osteoporosis 15.2 mg) and treatment time (normal 2.8 yrs, osteoporosis 5.6 yrs), in association with bone loss (Table 4). However, none of these parameters reached statistical significance for this sample.
Some diseases have an intrinsic risk of bone loss. Steroid-treated rheumatoid arthritis has a high rate of osteoporosis in comparison to asthma or polymyalgia rheumatica, but these also carry some intrinsic risk.11,12,13 The prevalence of low bone density has not been investigated in patients with ophthalmic inflammatory disease, but one previous study examined 15 patients with steroid-treated thyroid eye disease14 and found that four were osteoporotic, and a study of 602 patients with various ocular inflammatory diseases identified 17 pathological fractures (2.8%).15 The selection of patients for our study was neither comprehensive nor prospective and the results cannot reliably be extrapolated to a wider population. However, it is likely that patients included were selected for perceived risk. Because of this sampling bias, it is most unlikely that these 129 patients represented an underestimate of steroid-induced bone loss in uveitis patients. In our cohort the prevalence of osteoporosis was 15% and the symptomatic fracture rate, 6%. Indeed, only four patients with low bone density suffered a fracture (3% of all patients), which represents one such event per 118 patients treatment years. The reported prevalence of osteoporosis and fracture in other disease groups is substantially higher, including a 34% rate of vertebral fracture in rheumatoid arthritis treated with 5 mg/day or more of prednisolone over 5 yrs16 and a 42% rate of fracture in asthmatics on high-dose prednisolone.17 Uveitis per se shows no evidence of an intrinsic risk of bone loss.
Some patients (indeed, nearly half of our patients) taking systemic steroid treatment had additional risks for osteoporosis and it is important to identify these (Table 3). Eighteen women were post-menopausal and nine had pregnancies during treatment. Three had previous episodes of amenorrhoea or had undergone oophorectomy, both of which are potent causes of osteoporosis.18 Smoking (11% of this cohort) accelerates bone resorption and in women, accelerates the menopause and catabolises oestrogens thereafter. Some patients with sarcoidosis have hypercalcuria and lose bone. Osteoporosis is weakly associated with inflammatory bowel disease, partly because of malabsorption.19 Inflammatory arthropathy, particularly rheumatoid arthritis20 leads to bone loss, not least because of decreased mobility; total immobilisation leads to bone resorption at a rate of 1% per week. Type 1 diabetics have on average a 10% reduction in bone mass;21 type 2 diabetics are less severely affected. Anorexia or poor diet, low body weight, associated amenorrhoea and hypercortisolism can cause rapid osteoporosis.22 Bone loss also occurs in hypogonadal males, in hyperparathyroidism, after heparin treatment23 and in alcoholism24 (it is now recognised that bone loss may occur with only moderate alcohol intake, at least in women,25 implying that patients should be encouraged to reduce intake if necessary).
The value of drug prophylaxis against bone loss in those at risk has been the subject of intensive research, and as yet firm conclusions are lacking. Calcium and vitamin D supplementation have been shown to ameliorate bone loss26 and bisphosphonates unarguably reduce bone loss and replenish bone once lost.5,27 Other drugs such as calcitriol28 and calcitonin29 prove beneficial in some circumstances. However, the only adverse event associated with bone loss is bone fracture, and the effect of prophylaxis on fracture prevalence has not been conclusively established. Nevertheless there is now a medical consensus on the need to treat in some circumstances.
The National Osteoporosis Society (NOS), in association with The British Society for Rheumatology, the Royal Society of Medicine and others, has published guidelines on the prevention and management of steroid-induced osteoporosis.30 Although this is only one of a plethora of published guidelines, it has the benefit of clarity, conciseness and a practical approach. It is possible that further studies will confirm our impressions that the risks of bone loss are low for patients with uveitis, but pending such studies the NOS guideline provides a useful safety protocol for the ophthalmologist.
Patients using 5 mg of prednisolone or more per day for several months or more should be considered at risk of bone loss. This will exclude, for instance, those taking steroids for an average 8–10 weeks in the management of acute ocular toxoplasmosis. All such patients should be informed about bone loss and other complications. Adequate dietary calcium and vitamin D should be maintained (deficiency in a Western diet is unusual but guidelines are readily available). If there is any doubt about dietary intake or if the patient is relatively immobile, supplementary calcium and vitamin D3 should be taken. Alcohol intake should be limited to recommended norms. Smokers should be encouraged to stop. Walking for the equivalent of two miles or more per day should be encouraged if possible. Post-menopausal women already using HRT should be encouraged to continue if risks are acceptable. Patients should be screened for additional risk factors. If there are none, if the patient is under 65 and the dosage is under 15 mg/day, no further action is necessary. If the steroid dosage is >15 mg/day, if the patient is over 65, or if there are additional risk factors, the NOS guideline should be followed.
If treatment is considered necessary, the drug of choice for all patients is a bisphosphonate. The optimum form of treatment for steroid-induced bone loss is still subject to review, the two main choices being cyclical etidronate with calcium, or weekly alendronate. Post-menopausal women alternatively can use HRT, which will require the agreement and cooperation of the general practitioner. Patients requiring treatment also require assessment for additional risk factors. If any patient has suffered a fracture, we recommend referral to a physician with an expertise in the management of osteoporosis. We also recommend such referral if a patient is intolerant of bisphosphonate treatment (typically because of heartburn) or for any patient under 65 with osteoporosis (T < −2.5).
Systemic steroids remain the mainstay of treatment for most severe inflammatory diseases despite the increasing availability of immunosuppressives. However, immunosuppressives (most frequently cyclosporin) were used in over one quarter of our patients in order to lower steroid dosage. These drugs allow a reduction in steroid dose in most patients, often by 50% or more and thus bone loss may be ameliorated. However, it is known that cyclosporin itself causes high-turnover bone loss, possibly by reducing testosterone in combination with other effects.31,32,33 The combination of prednisolone and cyclosporin could theoretically increase bone loss, but in this series only one of 27 patients using cyclosporin was osteoporotic.
The frequency of male osteoporosis (14/68, 20.6%) in this study is striking, and all of these were 60 yrs or below. In contrast only 6/61 women (9.8%) were osteoporotic, and four of these were over 60 yrs. There is no significant difference between the treatment parameters of males and females in this study. The use of T < −2.5 to define osteoporosis in men is not universally accepted as it is for women, because of the technicalities of the interpretation of bone density.34,35 Young men have the greatest risk of high-impact fracture, and osteoporosis is common in those with associated risk factors,36 especially hypogonadism. Men are also more susceptible to bone loss at equivalent doses of steroid, than are premenopausal women.6 They should be considered an at-risk group37,38 and it is reasonable to define both male and female osteoporosis using the same criteria.
In conclusion, steroid-induced osteoporosis is an important cause of morbidity. This study suggests that its prevalence is lower in patients with uveitis than in some other disease groups but has highlighted the risk to young men. Bone loss can be reduced by optimising lifestyle and diet, by the identification of pre-existing risk factors and by the use of appropriate prophylaxis and treatment.
References
Hodgkins P, Hull RG, Evans AR, Jeffrey MN . Osteoporosis: a survey of consultant ophthalmologists. Br J Ophthalmol 1997; 81: 260
Walsh LJ, Wong CA, Pringle M, Tattersfield AE . Use of oral corticosteroids in the community and the prevention of secondary osteoporosis: a cross sectional study. Br Med J 1996; 313: 344–346
Stanbury R, Graham EM . Systemic corticosteroid therapy – side effects and their management. Br J Ophthalmol 1998; 82: 704–708
Jabs DA, Rosenbaum JT, Foster CS, Holland GN, Jaffe GJ, Louie JS et al. Perspective: guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol 2000; 130: 492–513
Mulder H, Struys SA . Intermittent cyclical etidronate in the prevention of corticosteroid-induced bone loss. Br J Rheumatol 1994; 33: 439–447
Lukert BP, Raisz LG . Glucocorticoid induced osteoporosis; pathogenesis and management. Ann Intern Med 1990; 112: 353–3564
Baillie SP, Davison CE, Johnson FJ, Francis RM . Pathogenesis of vertebral crush fractures in men. Age Ageing 1992; 21: 139–141
Reid DM . Corticosteroid osteoporosis. In: Francis RM (ed). Osteoporosis: Pathogenesis and Management Kluwer: Lancaster 1990 103–144
Cooper C, Coupland C, Mitchell M . Rheumatoid arthritis, corticosteroid therapy and hip fracture. Ann Rheum Dis 1995; 54: 49–52
Lees B, Banks LM, Stevenson JC . Bone mass measurements In: Stevenson JC, Lindsay R (eds) Osteoporosis Chapman & Hall: London 1998 pp 137–155
Hahn TJ, Boisseau VC, Avioli LV . Effect of chronic corticosteroid administration on diaphyseal and metaphyseal bone mass. J Clin Endocrinol Metab 1974; 39: 274–282
Mueller MN . Effects of corticosteroids on bone mineral in rheumatoid arthritis and asthma. Am J Roentgenol 1976; 126: 1300
Reid DM, Nicoll JJ, Smith MA et al. Corticosteroids and bone mass in asthma: comparisons with rheumatoid arthritis and polymyalgia rheumatica. Br Med J 1986; 293: 1463–1464
Baschieri L, Antonelli A, Nardi S et al. Intravenous immunoglobulin versus corticosteroid in treatment of Graves’ ophthalmopathy. Thyroid 1997; 7: 579–585
Tamesis RR, Rodriguez A, Christen WG, Akova YA, Messmer E, Foster CS . Systemic drug toxicity trends in immunosuppressive therapy of immune and inflammatory ocular disease. Ophthalmology 1996; 103: 768–775
Michel BA, Bloch DA, Fries JF . Predictors of fractures in early rheumatoid arthritis. J Rheumatol 1991; 18: 804–808
Adinoff AD, Hollister JR . Steroid-induced fractures and bone loss in patients with asthma. N Engl J Med 1983; 309: 265–268
Aitken JM, Hart DM, Anderson JB et al. Osteoporosis after oophorectomy for malignant disease in premenopausal women. Br Med J 1973; 2: 325–328
Greenstein AJ, Janowitz HD, Sachar DB . The extra-intestinal complications of Crohn’s disease and ulcerative colitis: a study of 700 patients. Medicine 1976; 55: 401–412
Hahn TJ, Boisseau VC, Avioli LV . Effect of chronic corticosteroid administration on diaphyseal and metaphyseal bone mass. Clin Endocrinol Metab 1974; 39: 274–282
Selby PL . Osteopenia and diabetes. Diabetic Med 1988; 94: 257–264
Rigotti NA, Neer RM, Skates SJ, Herzog DB, Nussbaum SR . The clinical course of osteoporosis in anorexia nervosa. A longitudinal study of cortical bone mass. JAMA 1991; 265: 1133–1138
Griffith GC, Nicholas G, Asher JD, Flanagan B . Heparin osteoporosis. JAMA 1965; 193: 91–94
Saville PD . Changes in bone mass with age and alcoholism. J Bone Joint Surg 1965; 47B: 492–499
Nordin BEC, Polley KJ . Metabolic consequences of the menopause. Calcif Tissue Int 1987; 41(suppl): 1–59
Buckley LM, Leib ES, Cartularo KS, Vacek PM, Cooper SM . Calcium and vitamin D3 supplementation prevents bone loss in the spine secondary to low-dose corticosteroids in patients with rheumatoid arthritis. Ann Intern Med 1996; 125: 961–968
Struys A, Snelder AA, Mulder H . Cyclical etidronate reverses bone loss of the spine and proximal femur in patients with established corticosteroid-induced osteoporosis. Am J Med 1995; 99: 235–242
Sambrook P, Birmingham J, Kelly P et al. Prevention of corticosteroid osteoporosis. A comparison of calcium, calcitriol, and calcitonin. N Engl J Med 1993; 328: 1747–1752
Cranney A, Welch V, Adachi JD et al. Calcitonin for the treatment and prevention of corticosteroid-induced osteoporosis. Cochrane Database Syst Rev 2000; 2: CD001983
Anon. Guidance on the Prevention and Management of Corticosteroid Induced Osteoporosis National Osteoporosis Society: Bath 1998
Thiebaud D, Krieg MA, Gillard-Berguer D, Jacquet AF, Goy JJ, Burckhardt P . Cyclosporine induces high bone turnover and may contribute to bone loss after heart transplantation. Eur J Clin Invest 1996; 26: 549–555
Bowman AR, Sass DA, Dissanayake IR et al. The role of testosterone in cyclosporine-induced osteopenia. J Bone Miner Res 1997; 12: 607–615
Stekelenburg J, Klein BY, Ben-Bassat H, Rojansky N . Opposing effects of cyclosporin A and tryphostin AG-1478 indicate a role for Src protein in the cellular control of mineralisation. J Cell Biochem 1998; 71: 116–126
Anderson FH . Osteoporosis in men. Int J Clin Pract 1998; 52: 176–180
Melton LJ, Khosla S, Achenbach SJ, O’Connor MK, O’Fallon WM, Riggs BL . Effects of body size and skeletal site on the estimated prevalence of osteoporosis in women and men. Osteoporos Int 2000; 11: 977–983
Kelepouris N, Harper KD, Gannon F, Kaplan FS, Haddad JG . Severe osteoporosis in men. Ann Intern Med 1995; 123: 452–460
Legrand E, Chappard D, Pascaretti C, Duquenne M, Rondeau C, Simon Y et al. Bone mineral density and vertebral fractures in men. Osteoporos Int 1999; 10: 265–270
Melton LJ, Atkinson EJ, O’Connor MK, O’Fallon WM, Riggs BL . Bone density and fracture risk in men. J Bone Miner Res 1998; 13: 1915–1923
Acknowledgements
We wish to acknowledge the support of the Iris Fund for Mr Stanford.
The authors have no financial or proprietary interest in any device or medication reported in this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jones, N., Anderton, L., Cheong, F. et al. Corticosteroid-induced osteoporosis in patients with uveitis. Eye 16, 587–593 (2002). https://doi.org/10.1038/sj.eye.6700163
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700163
Keywords
This article is cited by
-
Systemic corticosteroid use in UK Uveitis practice: results from the ocular inflammation steroid toxicity risk (OSTRICH) study
Eye (2021)
-
Nurse-led formal health review for immunosuppressed patients with uveitis
Eye (2009)
-
Strategien zur immunsuppressiven Therapie intraokularer Entz�ndungen
Der Ophthalmologe (2005)