Abstract
Purpose
To compare the visual fields (VFs) and optic nerve head changes between obstructive sleep apnoea (OSA) in normotensive patients and an age-matched non-OSA population.
Design
Case–control study.
Participants
A total of 41 ethnic Chinese patients diagnosed with moderate to severe OSA referred from the Sleep Laboratory, ENT Department, Tuen Mun Hospital. A total of 35 age–matched non-OSA subjects recruited from the Ophthalmology Department, North District Hospital.
Methods
Comprehensive ophthalmological and systemic history, complete ophthalmological examination, including central-30 computerized perimetry for all studied patients.
Main outcome measures
Polysomnographic data, VF indices, optic disc changes
Results
In the OSA arm, VF indices were significantly subnormal and the incidence of suspicious glaucomatous disc changes was four times higher than that of the control arm. None of the studied patients suffered from any form of anterior segment complications.
Conclusions
Moderate to severe OSA is associated with a higher incidence of VF defect and glaucomatous optic nerve changes.
Similar content being viewed by others
Introduction
Obstructive sleep apnoea (OSA) is a disease that is characterized by repetitive episodes of upper airway collapse during sleep. Apnoea is defined as cessation of oro-nasal flow for a duration of 10 s or more. Hyponoea is defined as reduction of oro-nasal flow for greater than 50% associated with a 4% of oxygen desaturation. The apnoeic hypopnoeic index (AHI) is the sum of the apnoea and hypopnoea events during an hour of sleep and is used to grade the severity of OSA. Patient is diagnosed to have OSA if the AHI is ⩾5. Mild OSA has an AHI between 5 and 20. Moderate OSA has an AHI of 20 to less than 40. Severe OSA has an AHI ⩾40.1, 2, 3, 4 OSA is well known to result in a number of health consequences: fragmentation of sleep leads to chronic sleep deprivation and daytime somnolence, hence affecting the patients' daily cognitive function and quality of life, increasing incidences of work-related and motor vehicle accidents; cardio-respiratory disturbances lead to elevated risks of complications such as hypertension, pulmonary hypertension, cardiac arrhythmia, myocardial infarction, congestive cardiac failure, and stroke.1, 2, 3, 4, 5, 6 Recently, possible ocular manifestations, including optic neuropathy in the form of visual field (VF) defect and disc oedema, normal-tension glaucoma (NTG), pseudotumour cerebri, nonarteritic anterior ischaemic optic neuropathy (NAAION); and anterior segment complications such as floppy eyelid syndrome, upper lid ptosis, lower lid ectropion, blepharochalasis, trichiasis, chronic conjunctivitis, keratoconus, exposure keratopathy, dry eyes, recurrent corneal erosion (RCE), keratitis, and progressive endotheliopathy have aroused ophthalmologists' concern.7, 8, 9, 10, 11, 12, 13, 14, 15 However, there are limited evidences in published articles of causal relationship between OSA and the various ocular manifestations, especially in the Chinese locality. Therefore, we designed a prospective case–control study to continuously recruit OSA patients, follow them up to determine the prevalence of ocular manifestations, and observed their progress. To detect any presence of suspected OSA-related optic neuropathy, we focus only on confirmed moderate to severe OSA cases and exclude high-tension glaucomatous cases. VF indices and the glaucomatous disc changes in the group of asymptomatic normotensive OSA patients were compared with a group of age- and sex-matched non-OSA patients. We believed that continuous collection and follow-up of OSA patients would give valuable information on whether the VF and optic disc changes are progressive and associated with OSA, and whether they are reversible with treatment of the OSA condition. We might also be able to demonstrate causal relationship between OSA and NTG, ischaemic optic neuropathy or other disease entities.
Method
We recruited 41 Chinese patients consecutively referred from the Sleep laboratory, Department of ENT, Tuen Mun Hospital from November, 2002 to July, 2003. They were confirmed to have moderate to severe OSA (AHI ⩾20) on polysomnography (Alice 3 Healthdyne Technologies, USA). 35 consecutive age- and gender-matched non-OSA subjects with negative history of snoring or excessive daytime somnolence were recruited as control subjects from the Ophthalmology Clinic, North District Hospital. A comprehensive history and a thorough ophthalmological examination was conducted by a single ophthalmologist (SL). Cup : disc ratio was measured under slit-lamp biomicroscope. A central-30 Humphery perimetry with undilated pupils and corrected refractive errors were obtained. Spot applanation tonometry was performed to all recruited subjects. If suspicious VF or optic disc was found, a 24-hours' phasing test using tonopen would be performed in supine posture (rechecked using applanation tonometry in upright posture if intraocular pressure >21 mmHg).16 Exclusion criteria for both arms included patients with known conditions which might affect VF result—high-tension glaucoma with intraocular pressure ⩾21 mmHg, intracranial or intraorbital space occupying lesions, optic neuropathies, arteritic AION, optic disc abnormalities, significant media opacity, known history of hypotensive crisis, and vasospastic diseases. Unreliable VF tests with fixation loss >15%, false positives or false negatives >15% were excluded. Patients with suspicious VF or disc changes were followed up and VF tests were repeated 2 months later for consistency. The more reliable field would be taken into account. Objective VF indices including the mean deviation (MD) and pattern standard deviation (PSD) were recorded. We studied the distribution of VF indices among the OSA and control arm and analysed the difference between the two arms using unpaired t-test. Within the OSA arm, Spearman's correlation test controlled for age and body mass index (BMI) was used to find if VF indices were significantly correlated to AHI and untreated duration of OSA, respectively. Incidence of suspicious disc changes with cup : disc ratio greater than 0.5, signs of pathological disc changes like vertical cupping, rim notching, disc haemorrhage, or disc swelling in the two arms were compared using χ2 test. All statistic calculations were carried out using SPSS soft-ware Version 11.0 (SPSS Inc., Chicago, IL, USA).
Results
In all, 72 eyes of 36 OSA patients (OSA arm) are compared with 59 eyes of 30 age- and sex-matched non-OSA subjects (Control arm). Demographic data are summarized in Table 1. Ten eyes in the OSA arm and nine eyes in the control arm were excluded according to the above-stated exclusion criteria. Within the OSA arm, 30% of studied eyes were in the group of patients with moderate (AHI<40), and 70% with severe (AHI⩾40) OSA. The mean duration of OSA symptoms without treatment was 5.6 years (range 0.5–20.0 years).
Figures 1 and 2 compare the distribution of VF indices between the OSA and control arm. There was a second peak of suboptimal MD at −3.5 MD in the OSA arm as compared to the normally distributed MD in the control arm. The distribution of PSD in the OSA arm was skewed away from the norm when compared to the control arm. The differences in VF indices (both MD and PSD) between the OSA and control arms were statistically significant (P<0.01).
Table 2 shows the results of statistical analysis of the VF indices within the OSA arm. No statistically significant correlation was found between the VF indices, the AHI, and the untreated duration of OSA in our study.
In Table 3, the incidence of suspicious glaucomatous disc changes in OSA arm was four times higher when compared to its control arm (26.39 against 6.78%), which was found to be statistically significantly different (P=0.001, 99% CI). However, there was no statistically significant difference found within the subgroups with moderate against severe OSA as shown in Table 4 (P=0.944). Table 5 shows that there was no statistically significant difference between the incidences of high-tension glaucoma in OSA and Control arm (P=0.765).
None of the studied patients had anterior segment complications like floppy eyelid syndrome, upper lid ptosis, lower lid ectropion, blepharochalasis, trichiasis, chronic conjunctivitis, keratoconus, exposure keratopathy, significant dry eyes, RCE, keratitis, or progressive endotheliopathy.
Discussion
Our study is the relatively largest sample-sized, case–control study comparing 72 eyes in confirmed moderate to severe OSA patients with a normal control group of 59 eyes. The results in our study showed a significant deviation of VF indices from norm and a higher incidence of suspicious glaucomatous optic disc in the OSA arm when compared to the age- and gender-matched non-OSA control arm. Argument on possibility of suboptimal VF performance by an OSA patient due to sleepiness during the test is excluded in our study as the entire examination was observed by a single, experienced technician. Moreover, VFs with fixation losses, false positives or false negatives of more than 15% were excluded and repeated. Although our current study is limited by its short duration and observational nature, a hypothesis that OSA causes the optic neuropathies is not without rationale. Repetitive apnoeas might lead to direct anoxic damage to the optic nerve, or indirect effect on optic nerve head blood flow. The latter might be secondary to (1) sympathetic surge-induced arterial hypertension and hypertensive arteriosclerosis, (2) vascular dysregulation due to imbalance between nitric oxide (vasodilator) and endothelin (vasoconstrictor), (3) abnormal platelet aggregation and activation leading to microinfarcts in the optic nerve, or (4) episodic-raised intracranial pressure.6, 15, 17, 18 The absence of statistically significant differences between the incidences of high-tension glaucoma in the OSA arm (3.66%) and control arm (2.94%) in our study, speaks against the hypothesis of unrecognized, nocturnal high-tension glaucoma as a cause of the optic neuropathy, which was suggested by Marcus et al.12
If the above hypothesis stands, logical questions follow: whether more severe form and longer duration of OSA would lead to more severe neuropathies, and whether the optic neuropathies can be reversible with treatment? In our study, we did not find any statistically significant positive correlation between the AHI and VF performance/disc changes as reported by Mojon et al9, 10 However, we have only included the moderate to severe OSA patients while leaving out the mild cases. Moreover, the majority (70%) of our studied cases suffered from severe OSA. Thus our study cannot rule out the presence of such a correlation. We did not find any statistically significant correlation between the duration of OSA and VF performance. However, the data duration of OSA was subjectively recalled by the patients and may not be totally reliable. Longer follow-up of more OSA patients would give valuable information on the progress of their VF and disc changes, whether the changes are reversible with treatment of the OSA condition, and whether OSA is associated causally with NTG, ischaemic optic neuropathy, or other disease entities.
Nevertheless, as found in our demographic data and Mohsenin et al paper, moderate to severe OSA most commonly occurs in middle aged male, who constitute the productive population in a society. 19 Therefore, the role of ophthalmologists in early screening for potentially blinding optic neuropathies in this group of patients is worthwhile from an economic standpoint. On the contrary, while encountering patients with unknown cause of optic neuropathies, some of them being diagnosed with and treated as NTG, it might be worthwhile to ask for a sleep history and refer suspicious cases for further investigations for OSA.
Conclusion
OSA is associated with a higher incidence of VF defect and glaucomatous optic disc changes in a group of Chinese normotensive patients.
References
Krug P . Snoring and obstructive sleep apnea. Ass Operating Room Nurses J 1999; 69: 792–801.
Guilleminault C, Stoohs R, Clerk A, Cetel M, Maistros P . A cause of excessive daytime sleepiness. The upper airway resistance syndrome. Chest 1993; 104: 781–787.
Masood A, Phillips B . Sleep apnoea. Curr Opin Pulmonary Med 2000; 6: 479–484.
Flemons WW . Obstructive sleep apnea. New Engl J Med 2002; 34: 498–504.
Akashiba T, Kawahara S, Akahoshi T, Omori C, Saito O, Majima T et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest 2002; 22: 861–865.
Siebler M, Nachtmann A . Cerebral hemodynamics in obstructive sleep apnea. Chest 1993; 103: 1118–1119.
Walsh JT, Montplaisir J . Familial glaucoma with sleep apnoea: a new syndrome? Thorax 1982; 37: 845–849.
Wolin MJ, Brannon WL . Disk edema in an overweight woman. Surv Ophthalmol 1995; 39: 307–314.
Mojon DS, Mathis J, Zulauf M, Koerner F, Hess CW . Optic neuropathy associated with sleep apnea syndrome. Ophthalmology 1998; 105: 874–877.
Mojon DS, Hess CW, Goldblum D, Fleischhauer J, Koerner F, Bassetti C et al. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology 1999; 106: 1009–1012.
Mojon DS, Hess CW, Goldblum D, Boehnke M, Koerner F . Normal-tension glaucoma is associated with sleep apnea syndrome. Ophthalmologica 2002; 216: 180–184.
Marcus DM, Costarides AP, Gokhale P, Papastergiou G . Sleep disorders: a risk factor for normal-tension glaucoma? J Glaucoma 2001; 10: 177–183.
Mojon DS, Hedges TR, Ehrenberg B, Karam EZ, Goldblum D et al. Association between sleep apnea syndrome and nonateritic anterior ischaemic optic neuropathy. Arch Ophthalmol 2002; 120: 601–605.
Lee AG, Golnik K, Kardon R, Wall M, Eggenberger E, Yedavally S . Sleep apnea and Intracranial Hypertension in Men. Ophthalmology 2002; 109: 482–485.
Mojon DS, Goldblum D, Fleischhauer J, Chiou AGY, Frueh BE, Hess CW et al. Eyelid, conjunctival, and corneal findings in sleep apnea syndrome. Ophthalmology 1999; 106: 1182–1185.
Santos MG, Makk S, Berghold A, Eckhardt M, Hass A . Intraocular pressure difference in Goldmann applanation tonometry versus Perkins hand-held applanation tonometry in overweight patients. Ophthalmology 1998; 105: 2260–2263.
Hayreh SS, Zimmerman MB, Podhajsky P, Alward WL . Nocturnal arterial hypotension and its role in optic nerve head and ocular ischemic disorders. Am J Ophthalmol 1994; 117: 603–624.
Bokinsky G, Miller M, Ault K, Husband P, Mitchell J . Spontaneous platelet activation and aggregation during obstructive sleep apnea and its response to therapy with nasal continuous positive airway pressure. A preliminary investigation. Chest 1995; 108: 625–630.
Mohsenin V . Gender differences in the expression of sleep-disordered breathing: role of upper airway dimensions. Chest 2001; 120: 1442–1447.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interest: Nil.
Financial support: Nil.
Rights and permissions
About this article
Cite this article
Tsang, C., Chong, S., Ho, C. et al. Moderate to severe obstructive sleep apnoea patients is associated with a higher incidence of visual field defect. Eye 20, 38–42 (2006). https://doi.org/10.1038/sj.eye.6701785
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701785
Keywords
This article is cited by
-
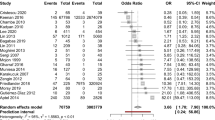
Ocular manifestations of obstructive sleep apnea: a systematic review and meta-analysis
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Retinal microcirculation characteristics in obstructive sleep apnea/hypopnea syndrome evaluated by OCT-angiography: a literature review
International Ophthalmology (2022)
-
Evaluation of retinal fiber thickness and visual pathways with optic coherence tomography and pattern visual evoked potential in different clinical stages of obstructive sleep apnea syndrome
Documenta Ophthalmologica (2020)
-
Evaluation of effects of positive airway pressure treatment on retinal fiber thickness and visual pathways using optic coherence tomography and visual evoked potentials in the patients with severe obstructive sleep apnea syndrome
International Ophthalmology (2020)
-
Correlation between structural progression in glaucoma and obstructive sleep apnea
Eye (2019)