Abstract
Purpose
To establish whether the effect of improved glaucoma detection in the community suggested by an intervention study is maintained when intervention is extended to include all optometrists in the area.
Methods
Optometrists’ in the Ealing, Hammersmith, and Hounslow area were invited to ongoing training sessions following completion of an intervention study. The number of optometrist initiated referrals to Ealing Hospital Eye Clinic (EHEC) for suspect glaucoma was assessed over a 12-month period. The positive predictive value (PPV) of those referrals was calculated and a historical comparison made with the results of the original study.
Results
A total of 376 new referrals for suspected glaucoma were assessed at EHEC during the 12-month period of data collection. This represents an increase in the number of referrals of 58% compared with an equivalent 12-month period during the initial intervention trial (376 vs238). The PPV was maintained at 0.45 (95% CI 0.41–0.51).
Conclusion
The rising number of new referrals for glaucoma together with maintenance of the PPV suggests an impact on the number of new cases of glaucoma detected in the community. The increase in referral numbers was limited to glaucoma when compared with new referrals for cataract. This implies a targeted effect of the intervention in terms of glaucoma detection. We believe the next step is to perform the study in an alternative location to see if the effect is repeatable elsewhere. If proven to be the case, there is a coherent argument for widespread adoption of this strategy to improve glaucoma case finding.
Similar content being viewed by others
Introduction
It is well established in the literature that the detection of glaucoma in the UK is largely dependent on the appropriate referral of patients who visit their optometrist.1, 2, 3, 4, 5 There is a wide variation of optometric practice across the profession for glaucoma detection, with tests such as tonometry and visual fields, being left to the discretion of the optometrist.6, 7, 8 Several approaches have been reported in the literature aimed at improving glaucoma case-finding.8, 9, 10, 11 At the Ealing Hospital Eye Clinic (EHEC), the glaucoma department has been working with local optometrists to improve case finding for glaucoma.6, 9
An intervention study was conducted at EHEC and has been reported previously.9 The local optometric practices that routinely referred to EHEC were divided into two groups taking into consideration those practices, which shared an optometrist (a cluster) and the number of optometrist days worked per week. One group of practices acted as controls, while the other practices were invited to receive intervention.
The intervention had three components.
-
1
Training in optic disc assessment with systematic evaluation of the optic nerve head.
-
2
Provision of standardised referral guidelines for all intervention clusters.
-
3
Ophthalmologist feedback sent to each referring optometrist in the intervention clusters, detailing the ophthalmologist's findings, diagnosis and management plan for each patient who presented with suspect glaucoma to EHEC.
The study looked at the number of optometrist referrals for suspected glaucoma and the positive predictive value (PPV) of those referrals before and during the cluster randomised intervention.6, 9
The outcome of this trial suggested that an intervention resulted in an increase in numbers referred with suspected glaucoma with no significant change in the PPV of the referrals. This means that intervention may result in an increased number of glaucoma cases detected in the community.9
In response to this finding the intervention was extended to include all optometric practices in the Ealing, Hammersmith, and Hounslow areas (ie those randomised in the original intervention study (intervention and control practices) and nonrandomised practices ie outside the original trial group). This is a historical comparison study following the intervention study.9
For this phase of the study, we looked at all the referrals for suspected glaucoma over a 12-month period, commenced 14 months after the end of the first trial. The intervention and training continued on a smaller scale, but was directed to the whole group (rather than only to the intervention group as in the previous study). The goal was to identify the impact of this ongoing training with the local optometrists. There were two aspects to this. Firstly, we aimed to determine if the effect already suggested in the intervention arm of the first study was maintained. Secondly, we wished to see if the impact of increased numbers of glaucoma cases detected was achieved in the original control group and those optometric practices not randomised in the first study.
Methods
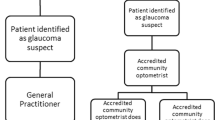
All patients referred by an optometrist for suspected glaucoma over a 12-month period (June 2002–May 2003) were identified and data entered on a bespoke database. Patients excluded from analysis were those referred by an ophthalmic medical practitioner (OMP), general practitioner (GP) (not initiated by an optometrist), or other hospital departments with suspected glaucoma, or those referred for other conditions and were subsequently found to have glaucoma. Also excluded from analysis were patients who failed to attend appointments within the 12-month period. The resultant database of attendees was cross checked with details of all new patients attending from the clinical profiles over the same period to ensure maximal data capture.
Each patient had a structured assessment, which included history, visual acuities, Goldmann applanation tonometry, gonioscopy, and optic disc assessment with biomicroscopy through dilated pupils. Visual fields examination was performed on a Humphrey Fields Analyser.
All information obtained at the first assessment was presented to the consultant at a later date for classification as confirmed glaucoma, suspect glaucoma, ocular hypertension or not glaucoma. The definitions for all diagnostic categories have been previously reported.9
Intervention/training
The continued intervention comprised of lectures and practical sessions every 4 months, which commenced in May 2002. The lectures were linked and organised with the Local Optometric Committee of Ealing, Hammersmith, and Hounslow. For each lecture an invitation was sent to each optometric practice in these areas. During the period of the data collection and prior to this period all the lectures were given on glaucoma related topics by consultants with a special interest in glaucoma.
To promote the communication between ophthalmologists and optometrists, every effort was made to reply to each referring optometrist, detailing the findings, diagnosis, and management plan for the patient.
Data analysis
The impact of the continued intervention was assessed by examining the number of referrals for suspected glaucoma from all the practice categories and the PPV of those referrals.
Results
Number of referrals
During the 12-month data collection period from June 2002 to May 2003 inclusive, 414 patients were referred for suspected glaucoma. In all, 31 (7.5%) patients did not attend their clinical appointment and seven sets of clinical notes were not found. The remaining 376 patients’ clinical data were assessed.
In view of the outcomes of interest in this study the numbers referred are presented by practice group from which they originated. During the original intervention study three groups of practices were identified. Those not included in the intervention study (nonrandomised), those in the intervention group of the study and those in the control group of the study. In the original study, 397 patients were assessed over a 20-month period, which over a 12-month period averages out to 238 patients, 126 from the intervention group, 72 from the control group and 40 from practices outside the original trial area.
In this study, out of the 376 patients assessed, 183 were from the intervention group, 86 from the control group, 59 from practices outside the original trial area and 50 from optometrists who could not be identified. An increase in referral numbers was seen in all three groups of practices. Overall there was a 58% (376/238) increase in the referral numbers.
Positive predictive value
The same definition was used for an appropriate referral as in the previous reports, namely a diagnosis of confirmed or suspected glaucoma.9 On this basis, 171/376 of all assessed referrals resulted in a positive outcome (PPV=0.45 (95% CI 0.41–0.51)). The PPV of referrals were similar for each of the groups of practices. From the intervention group 93/183 resulted in a positive referral (PPV=0.51 (95% CI 0.44–0.58)) and from the control group 35/86 were positive referrals (PPV=0.41 (95% CI 0.31–0.51)). From the nonrandomised trial group 22/59 resulted in positive referral (PPV=0.37 (95% CI 0.26–0.50)). 21/48 (PPV=0.44 (95% CI 0.31–0.58)) resulted in positive referrals from optometrists who could not be identified.
From the original intervention study, the number of referrals that resulted in a positive outcome was 102/210 from the intervention group (PPV=0.49 (95% CI 0.42–0.55)) and 55/119 from the control group (PPV=0.46 (95% CI 0.38–0.55)). From the nonrandomised trial group 37/68 resulted in positive referral (PPV=0.54 (95% CI 0.43–0.66)).
This signifies that despite a rise in number of referrals, there is no change to the PPV in the intervention study compared to the post intervention.
Diagnosis
About a quarter of those referred for suspected glaucoma reported a family history of the disease. Over half (251/415) of the patients who were referred had referring Intraocular pressures <22 mmHg in both eyes.
The breakdown of diagnoses following an initial clinic visit for those referred with suspected glaucoma are presented in Figure 1. The most frequent abnormal finding was glaucoma suspect with open angle glaucoma (POAG+NTG) the second most common abnormal findings.
Discussion
This study is a continuation from our previous intervention study.9 The findings again show that the intervention has had a positive effect on the number of glaucoma referrals from optometric practices. There is an increase in referral numbers and the PPV is maintained. This suggests that the number of new cases of glaucoma detected in the community may have increased further.
It is difficult to comment fully regarding the different groups since we were unable to determine the optometrist for 50 referrals. This means all estimates of effect on referral numbers are likely to be underestimates. The fact that there are more referrals from the intervention group compared to the control group (183 vs 86) suggests that the length of time of intervention maybe important.
It could be that the increase in glaucoma referrals is due to other factors, such as changing GP referral patterns in the area. In order to investigate this possibility, we looked at the referrals over an equivalent 6-month period (between August and February) for each stage of the study. The results are shown in Tables 1 and 2. An increase in cataract referrals from before the original intervention study to during the original intervention study is seen suggesting a change in GP referral practices into the clinic. The numbers of glaucoma referrals, however, rose more markedly than the cataract referrals during this period (χ2=18.4, P<0.001). This suggests an effect in addition to a change in GP referral practice reflected in the cataract referrals. Between the original intervention study period and the current intervention period there was no change in cataract referrals into the clinic. The numbers of glaucoma referrals, however, rose markedly implying a continuing effect (χ2=14.4, P<0.001).
These findings suggest that there may be a benefit in implementing an intervention programme to improve glaucoma case detection. It is important to know if the findings are generalisable hence a repeat study of similar design needs to be undertaken in an alternative location. If the findings were confirmed a coherent argument could be made for the wider adoption of an intervention strategy.
References
Sheldrick JH, Ng C, Austin DJ, Rosenthal AR . An analysis of referral routes and diagnostic accuracy in cases of suspected glaucoma. Ophthal Epidemiol 1994; 1: 31–39.
Bell RWD, O’Brien C . Accuracy of referral to a glaucoma clinic. Ophthal Physiol Opt 1997; 17 (1): 7–11.
Newman DK, Anwar S, Jordan K . Glaucoma screening by optometrists: positive predictive value of visual field testing. Eye 1998; 12: 921–924.
Pooley JE, Frost EC . Optometrists’ referrals to the Hospital Eye Service. Ophthal Physiol Opt 1999; 19: S16–S24.
Lash SC . Assessment of information included on the GOS 18 referral form used by optometrists. Ophthal Physiol Opt 2003; 23: 21–23.
Theodossiades J, Murdoch IE . Positive predictive value of optometrist initiated referrals for glaucoma. Ophthal Physiol Opt 1999; 19: 62–67.
Vernon SA, Henry DJ . Do optometrists screen for glaucoma? Eye 1989; 3: 131–134.
Tuck MW, Crick RP . Efficiency of referral for suspected glaucoma. BMJ 1991; 302 (6783): 998–1000.
Theodossiades J, Murdoch IE, Cousens S . Glaucoma case finding: a cluster-randomised intervention trial. Eye 2004; 18: 483–490.
Vernon SA, Ghosh G . Do locally agreed guidelines for optometrists concerning the referral of glaucoma suspects influence referral practice? Eye 2001; 15: 458–463.
Henson DB, Spencer AF, Harper R, Cadman EJ . Community refinement of glaucoma referrals. Eye 2003; 17: 21–26.
Acknowledgements
We thank the Ealing, Hammersmith and Hounslow optometrists for their ongoing interest and support. The International Glaucoma Association supported the original intervention study. Frank Munroe kindly provided the information for cataract referral numbers for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patel, U., Murdoch, I. & Theodossiades, J. Glaucoma detection in the community: does ongoing training of optometrists have a lasting effect?. Eye 20, 591–594 (2006). https://doi.org/10.1038/sj.eye.6702000
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702000
Keywords
This article is cited by
-
Systematic review of the appropriateness of eye care delivery in eye care practice
BMC Health Services Research (2019)
-
Optometrists referrals for glaucoma assessment: a prospective survey of clinical data and outcomes
Eye (2010)
-
The influence of socioeconomic and clinical factors upon the presenting visual field status of patients with glaucoma
Eye (2009)