Abstract
Aims
To determine the efficacy and safety of trabeculotomy in congenital glaucoma patients operated on within first 3 months of birth.
Methods
A total of 36 eyes of 24 patients with congenital glaucoma, who underwent primary trabeculotomy within first 3 months of birth were included. Preoperative and postoperative intraocular pressures (IOP), corneal clarity, diameter, axial length, success rates, and complications were evaluated in this study.
Results
The mean follow-up was 38.38±11.77 months (range 12–48 months). Mean IOP was 33.16±7.28 mmHg (range 23–50 mmHg) preoperatively. At the final follow-up visit, the mean IOP was 21.41±7.34 mmHg (range 8–38 mmHg). Pre-and postoperative IOP differences were statistically significant at all examination periods (P<0.001). A12-, 24-, and 36-month success rates were 92, 82, and 74%, respectively. Survival analysis regarding to gender, preoperative corneal diameter and consaguinity were not statistically significant. Only preoperative axial length was a statistically significant parameter (P=0.024) for success. Postoperatively normal corneal clarity was achieved in 29 eyes (80.5%). The main complications were shallow anterior chamber in one (4.2%) eye and detachment of Descement's membrane in two (8.4%) eyes.
Conclusions
Primary trabeculotomy is a safe and effective procedure for congenital glaucoma patients when operated within 3 months of birth. It has a favourable IOP control and a low rate of complications in three year period.
Similar content being viewed by others
Introduction
Developmental glaucoma is responsible for 2. 5–15% of all documented cases of pediatric blindness.1, 2 This poor prognosis of congenital glaucoma has changed recently with early diagnosis and introduction of microsurgical techniques.3, 4, 5, 6 However, only a few studies exist on the trabeculotomy results in congenital glaucoma patients who were operated within first months of birth.
This study was undertaken to evaluate the 3-year success of congenital glaucoma patients, who underwent primary trabeculotomy within first 3 months of birth.
Patients and methods
Patients
We evaluated retrospectively 36 eyes of 24 patients who underwent primary trabeculotomy within first 3 months of birth, between January 1999 and February 2003. Ethichs Committee for Human Research at the Ankara Research and Education Hospital approved this study.
All patients underwent a complete ocular examination under general anesthesia (halothane, nitrous oxide, and oxygen) before, during and after surgery. Ketamine was not used as an anesthetic agent. Corneal diameter, anterior segment evaluation, intraocular pressure (measured with the Tonopen-XL®) were recorded in the early phase of inhalation anesthesia in all cases, and gonioscopy, cyclopegic refraction (by cyclopentolate 1%) and fundoscopy were performed when the media were sufficiently clear. Axial length was measured by ultrasound biometer before and at each visit after surgery. Visual acuity and visual field testing were not included due to lack of reliability in our patient population.
Surgical technique
The surgical technique used in all cases was primary trabeculotomy under general anesthesia. All trabeculotomy procedures performed by one surgeon (ISY), using a fornix-based conjunctival flap in the superior quadrant, followed by 4 × 4 mm triangular partial thickness scleral flap, which was prepared by dissecting the sclera forward into the clear cornea. A 2 mm radial incision was performed at the corneoscleral transition zone to find Schlemm's canal (Figure 1). A modified Harms trabeculotome was inserted into the lumen on either side of the incision, and carefully rotated into the anterior chamber with the other parallel arm as a guide. The scleral flap was sutured with two 10-0 nylon sutures. The conjunctiva was closed with two 10-0 nylon sutures. The patients that their Schlemm's canal were not identified during trabeculotomy were not included in this study.
Postoperative follow-up
All the patients were treated with topical pilocarpine HCL 1% twice daily for 2 weeks and the prednisolone acetate 1% six times a day, tapered gradually over 8-week period and were examined 1 day, 1 week, and 1 month after surgery, followed by examination at every 2 months thereafter. Patients who could not be examined properly at the outpatient conditions were programmed for examination under anaesthesia.
Criteria for success and failure
Criteria for success were defined as intraocular pressure (IOP) >18 mmHg and <5 mmHg without additional further glaucoma surgery, stabilization of cup-to-disc ratio, and lack of further corneal enlargement. Postoperative use of antiglaucoma medications was not a criterion of success or failure.
Statistical analysis
Results are expressed as mean±standard deviation (SD). With the SPSS (SPSS for Windows, version 12.0, SPSS, Chicago, IL, USA) software, analyses of continuously scaled variables before and after surgery were made using the paired t-test. The cumulative probability of success was analysed by Kaplan–Meier life-table analysis. The Pearson χ2 and Fisher's Exact test was used to asses the significance of the differences among gender, preoperative corneal diameter, IOP level and consaguinity in surgical success. P-values <0.05 were considered statistically significant.
Results
Patient characteristics
A total of 36 eyes of 24 patients were included in the study. Eight (33.3%) patients were female and 16 (66.6%) patients were male (male/female=2/1). Mean age at presentation was 65.19±26.82 days (range 25–90 days). The mean duration between age of onset and surgery was 19.3±8.9 days (range 10–30 days). The study population primarly had congenital glaucoma. The mean follow-up was 38.38±11.77 months (range 12–49 months). A history of consaguinity among the parents was present in 19 (79.2%) out of 24 patiens. The glaucoma was unilateral in 12 patients (50%) and bilateral in 12 patients (50%) (Table 1).
Intraocular pressure
Mean intraocular pressure was 33.2±7.28 mmHg (range 23–50 mmHg) preoperatively. Mean intraocular pressures were 14.80±3.53 mmHg (range 10–25 mmHg) at 6 months, 17.02±4.89 mmHg (range 8–32 mmHg) at 1 year, 19.06±5.08 mmHg (range 11–36 mmHg) at 2 years, 19.62±4.74 mmHg (range 12–31 mmHg) at 3 years and 21.41±7.34 mmHg (range 8–38 mmHg) and 4 years postoperatively. Pre-and postoperative IOP differences were statistically significant at all periods, respectively, (P<0.001). The percentage of reduction in IOP was 36.4±3.4 mmHg (Table 2, Figure 2).
Glaucoma medications
The mean antiglaucoma medication were 2.52±0.77 (range 2–4) preoperatively and 1.77±0.98 (range 0–3) postoperatively at the most recent follow-up examination (P<0.05). At the last follow-up, two eyes (5.5%) eyes were on three medications whereas, 10 eyes (27%) were free of antiglaucoma medications.
Surgical success
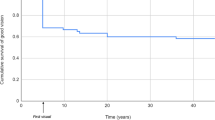
Figure 3 shows the cumulative probability of success (Kaplan–Meier life table analysis) following primary trabeculotomy operation, with 97% success at 6 months, 92% success at 1 year, 82% success at 2 years, 74% success at 3 years after surgery.
Factors associated with surgical success
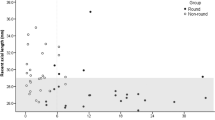
Gender (P=NS), consaguinity (P=NS), preoperative IOP>30 mmHg (P=NS), corneal diameter >12.5 mm (P=NS) were not determining factors for surgical success. Buphthalmic eyes with axial length >22 mm had a significantly worse outcome from remaining eyes (P=0.024).
Corneal diameter, clarity, and axial length
Mean horizontal corneal diameters at presentation were 12.30±0.85 mm (range 11–14 mm) and at last visit were 12.95±0.75 mm (range 12–15 mm). The increase in corneal diameters as measured an the last visit was statistically significant (P<0.001).
Before surgery 30 eyes (83.3%) had corneal oedema. One eye (4.2%) had corneal scarring and remained same despite the effective IOP control postoperatively. At the final follow-up visit 29 eyes (80.5%) had clear corneas.
Mean axial lengths at presentation were 20.43±2.03 mm (range 18–24 mm) and at last visit were 22.92±2.20 mm (range 20–26 mm). The increase in axial length as measured at the last visit was statistically significant (P<0.001).
Complications
Complications occured in three eyes. Shallow anterior chamber was seen in one eye (4.2%). It resolved within 2 weeks. Transient hypotonia was seen in this case also. Detachment of Descement's membrane was occured in two (8.4%) eyes. Reattachment of Descement's membrane was achieved with injection of viscoelastics. Intraocular haemorrhage was managed by using cohesive viscoelastics and leaving it in the anterior chamber.
Discussion
The main pathology in congenital glaucoma is the developmental malformations of the trabecular meshwork and the iris, which create a pathologically increased resistance to aqueous outflow.1, 2 In the management of congenital glaucoma, surgical treatment is required to restore outflow facility by opening the abnormal trabecular meshwork and two procedures are generally used; trabeculotomy or goniotomy. Goniotomy has remained the primary surgical treatment of choice for congenital glaucoma since Otto Barkan first applied the technique in 1938 but it is a technically challenging procedure and used only if the cornea is clear.7 Russell-Eggitt et al.8 reported a long-term follow-up study of patients with congenital glaucoma in which they showed that a single goniotomy was successful in achieving IOP control in 71% of eyes and 93.5% success was achieved by one or more goniotomies. The main advantage of goniotomy is the preservation of conjunctiva for any future drainage surgery. In our patient population, 83.3% of the eyes presented with severe corneal oedema, and goniotomy was technically not feasible.
Trabeculotomy is an alternative technique, more predictable than goniotomy and can easly be performed in the presence of severe corneal edema. Anderson3 reported that both goniotomy and trabeculotomy were equally effective in terms of IOP control but Akimoto,4 Mc Pherson,9 and Meyer10 reported a higher success rate with trabeculotomy as the initial procedure.
This is the first study for comparing the 3-year results of trabeculotomy for congenital glaucoma patients who were operated within first 3 months of birth. Kaplan–Meier survival analysis demonstrated the success probabilities of 92 , 82, and 74% at the first, second and third year, respectively, in our study (Figure 3). According to these results, early trabeculotomy is an effective procedure for IOP control especially first 3-year of life for congenital glaucoma patients which is a critical period for anterior segment development. Performing a filtration surgery such as trabeculectomy during this period is technically difficult and gives invitation to devastating complications such as inadvertent scleral perforation, prolapse of vitreous and late retinal detachment.11 Also trabeculectomy is generally considered to have poor outcome in childhood glaucoma and this is generally due to a thick Tenon's capsule, rapid wound healing response, lower scleral rigidity and a large buphthalmic eye with thin sclera in children. There have been few reports on the use of Mitomycin-C (MMC) during trabeculectomy in childhood glaucoma.12, 13, 14, 15, 16 Despite achieving good results with the use of MMC, it is not recommendable its use in children with early postnatal period because long-term results and complications of MMC use are not yet known.
Beck and Lynch17 described a technique of performing 360° trabeculotomy in a single procedure using a 6-0 polypropylene suture and reported an 87% success rate. Recently Mendicino et al18 reported the long-term surgical results of 360° trabeculotomy and goniotomy with a significantly better IOP control with the former technique. They commented that the actual placement of the suture into Schlemm's canal may be determined by gonioscopic visualization of the blue suture, which is possible in cases of mild corneal oedema. However, this technique is highly demanding compared with traditional trabeculotomy and severity of corneal oedema can preclude gonioscopic view of blue suture. Filous and Brunova19 reported the results of modified trabeculotomy in the treatment of congenital glaucoma by use of trabeculotomy probes more closely corresponding to the variable course of Schlemm's canal.
Combined trabeculotomy-trabeculectomy is another surgical alternative in newborn congenital glaucoma patients. The combined procedure theoretically provides for two major outflow pathways; the trabeculotomy creates a direct passage between the anterior chamber and Schlemm's canal, whereas the trabeculectomy allows the aqueous humor to bypass Schlemm's canal. Recently Mandal et al20, 21, 22 reported encouraging results with trabecolotomy-trabeculectomy procedure for congenital glaucoma patients when performed within a few months of birth. They reported the success probabilities of 94, 92, 87, 79, 73, and 63% at the first, second, third, fourth fifth, and sixth year, respectively.20 But Biedner and Rotkoff23 found no difference between trabeculotomy and combined trabeculotomy-trabeculectomy in a small series of 7 Arab Bedouin patients with congenital glaucoma. Also Mullaney et al24 reported 78% success rate in eyes with no coexistent anterior segment anormalies and 45% success rate in eyes with associated anterior segmen anormalies at 1 year and they used MMC in this procedure.
Criteria for surgical success in treatment of congenital glaucoma mostly comprise resolution of the corneal edema, stabilization of the corneal diameters, axial length, and cup-disc ratio. Corneal edema cleared in 29 eyes (80.5%) at the final follow-up in our study. Mean horizontal corneal diameters at presentation were 12.30±0.85 mm and at last visit were 12.95±0.75 mm (P<0.001). Mean axial lengths at presentation were 20.43±2.03 mm and at last visit were 22.92±2.20 mm (P<0.001). Prior studies3, 12, 25 have shown that successful surgery is more associated with a smaller corneal diameter. But, we found that axial length of the eye is a critical factor whereas corneal diameter, IOP, gender, and consaguinity were not found to influence outcome in our study. Dietlein et al11 have also shown that successful surgery is more associated with axial length <24 mm. They concluded that because of the streched limbal anatomy, the reading of the corneal diameter by calipers is not as precise as A-scan measurement of the axial length in congenital glaucoma patients. Also most anesthetic agents have lowering effect on IOP measurements. Lack of prognostic power for the preoperative IOP mainly be attributed to these factors in our study. Therefore, IOP readings obtained with the use of anaesthesia should never solely decide the diagnosis and prognosis of congenital glaucoma. The rate of consaguinity was 79.2% in our study. Consaguinity has been suggested to be correlated with an accelerated clinical course.26, 27 But it was not found to influence of surgical success in our study. This result is probably related to high proportion of consaguinty in our study group.
Visual acuity measurements are difficult in congenital glaucoma, with a mean presenting age 65.19±26.82 days and a mean follow-up of 38.38±11.77 months. Therefore, final rate of ambliyopia in these cases cannot be presented at the present follow-up.
There were no significant intraoperative and postoperative complications in any patients in the present study. Detachment of Descement's membrane occured in two (8.4%) eyes. It was cleared with injection of viscoelastics simultaneously. Shallow anterior chamber occured in one (4.2%) eye and the anterior chamber deepened spontaneously. Intraocular hemorrhage was also managed by using cohesive viscoelastics intraoperatively (Table 3).
Our study shows that, primary trabeculotomy appears to be effective for the control of intraocular pressure in eyes with congenital glaucoma operated within three months of birth during 3 years follow-up. As resurgery is often inevitable in congenital glaucoma owing to long life expectancy, a step-wise surgical strategy has to be keep in mind. This procedure was largely free from complications, and IOP was effectively controlled in these patients during 3 years of period. Also our study indicates that, preoperative large axial length is the key to a limited prognosis of surgery more than level of IOP, corneal diameters, gender, and consanguinity in congenital glaucoma patients.
References
Duke-Elder S ed. System of Ophthalmology, Vol. 3, Part 2, Congenital deformities. St. Louis: CV Mosby, 1969.
DeLuise VP, Anderson DR . Primary infantile glaucoma (Congenital Glaucoma). Survival Ophthalmol 1983; 28 (1): 1–19.
Anderson DR . Trabeculotomy compared to goniotomy for glaucoma in children. Ophthalmology 1983; 90: 805–806.
Akimoto M, Tanihara H, Negi A, Nagata M . Surgical results of trabeculotomy ab externo for developmental glaucoma. Arch Ophthalmol 1994; 112: 1540–1544.
Debnath SC, Teichmann KD, Salamah K . Trabeculectomy vs trabeculotomy in congenital glaucoma. Br J Ophthalmol 1989; 73: 608–611.
Hoskins Jr HD, Shaffer RN, Hetherington J . Goniotomy vs trabeculotomy. J Pediatr Ophthalmol Strabismus 1984; 21: 153–158.
Barkan O . Technique of goniotomy. Arch Ophthalmol 1938; 19: 217–223.
Russell-Eggitt IM, Rice NSC, Jay B, Wyse RKH . Relapse following goniotomy for congenital glaucoma due to trabecular dysgenesis. Eye 1992; 6: 197–200.
Mc Pherson Jr SD, McFarland D . External trabeculotomy for developmental glaucoma. Ophthalmology 1980; 87: 302–305.
Meyer G, Schwenn O, Pfeiffer N, Grehn F . Trabeculotomy in congenital glaucoma. Graefe's Arch Clin Exp Ophthalmol 2000; 238: 207–213.
Dietlein TS, Jacobi PC, Krieglstein GK . Prognosis of primary ab externo surgery for primary congenital glaucoma. Br J Ophthalmol 1999; 83: 317–322.
Song J, Stinnett SS, Whitson JT, Kooner KS . Ten-year surgical experience with childhood glaucoma. J Pediatr Ophthalmol Strabismus 2003; 40: 11–18.
Mandal AK, Prasad K, Naduvilath TJ . Surgical results and complications of Mitomycin-C augmented trabeculectomy in refractory developmental glaucoma. Ophthalmic Surg Lasers 1999; 30: 473–480.
Rodrigues AM, Paranhos Jr A, Montezano FT, Melo PAA, Prata Jr J . Comparision between results of trabeculectomy in primary congenital glaucoma with and without the use of Mitomycin C. J Glaucoma 2004; 13: 228–232.
Yalvac IS, Nurozler A, Kahraman C, Kasim R, Duman S . The results of trabeculectomy with and without Mitomycin-C in young patients. Ophthalmologica 1998; 212: 399.
Ikeda H, Ishigooka H, Muto T, Tanihara H, Nagata M . Long-term outcome of trabeculectomy for the treatment of developmental glaucoma. Arch Ophthalmol 2004; 122: 1122–1128.
Beck AD, Lynch MG . 360 degrees trabeculotomy for primary congenital glaucoma. Arch Ophthalmol 1995; 113: 1200–1202.
Mendicino ME, Lynch MG, Drack A, Beck AD, Harbin T, Pollard Z et al. Long-term surgical and visual outcomes in primary congenital glaucoma. 360 degrees trabeculotomy versus goniotomy. J AAPOS 2000; 4: 205–210.
Filous A, Brunova B . Results of the modified trabeculotomy in the treatment of primary congenital glaucoma. J AAPOS 2002; 6: 182–186.
Mandal AK, Bhatia PG, Bhaskar A, Nutheti R . Long-term surgical and visual outcomes in Indian children with developmental glaucoma operated on within 6 months of birth. Ophthalmology 2004; 111: 283–290.
Mandal AK, Gothwal VK, Bagga H, Nutheti R, Mansoori T . Outcome of surgery on infants younger than 1 month with congenital glaucoma. Ophthalmology 2003; 110: 1909–1915.
Mandal AK, Naduvilath TJ, Jayagandan A . Surgical results of combined trabeculotomy- trabeculectomy for developmental glaucoma. Ophthalmology 1998; 105: 974–982.
Biedner BZ, Rothkoff L . Combined trabeculotomy-trabeculectomy compared with primary trabeculotomy for congenital glaucoma. J Pediatr Ophthalmol Strabismus 1998; 35: 49–50.
Mullaney PB, Selleck C, Al-Awad A, Al-Mesfer S, Zwaan J . Combined trabeculotomy and trabeculectomy as an initial procedure in uncomplicated congenital glaucoma. Arch Ophthalmol 1999; 117: 457–460.
Quigley HA . Childhood glaucoma: results with trabeculotomy and study of reversible cupping. Ophthalmology 1982; 89: 219–226.
Akarsu AN, Turacli ME, Aktan SG, Barsoum-Homsy M, Chevrette L, Sayh BS et al. A second locus (GLC3B) for primary congenital glaucoma (buphthalmus) maps to the 1p36 region. Hum Mol Genet 1996; 5: 1199–1203.
Ho CL, Walton DS . Primary congenital glaucoma:2004 Update. J Pediatr Ophthalmol Strabismus 2004; 41: 271–288.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary interest in any of the materials or techniques used in this study
Presented in part as a poster presentation at the Annual Meeting of the American Academy of Ophthalmology, New Orleans, Louisiana; October 2004
Rights and permissions
About this article
Cite this article
Yalvac, I., Satana, B., Suveren, A. et al. Success of trabeculotomy in patients with congenital glaucoma operated on within 3 months of birth. Eye 21, 459–464 (2007). https://doi.org/10.1038/sj.eye.6702223
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702223
Keywords
This article is cited by
-
Combined trabeculotomy–trabeculectomy with and without augmentation in primary congenital glaucoma: triple-armed randomized controlled trial
International Ophthalmology (2022)
-
Combined trabeculotomy-trabeculectomy using the modified Safer Surgery System augmented with MMC: its long-term outcomes of glaucoma treatment in Asian children
Graefe's Archive for Clinical and Experimental Ophthalmology (2018)
-
Retrospective observation on trabeculectomy of primary congenital glaucoma by applying biological amniotic membranes soaked with 5-fluorouracil
International Ophthalmology (2018)
-
Combined trabeculotomy and trabeculectomy: outcome for primary congenital glaucoma in a West African population
Eye (2011)
-
Clinical outcomes after Ahmed valve implantation in refractory paediatric glaucoma
Eye (2009)