Abstract
Purpose
To determine the outcome of dacryocystorhinostomy (DCR) for nasolacrimal duct obstruction (NLDO) in children.
Methods
A review of medical records of 104 cases (82 patients) of paediatric DCR who underwent DCR at the Sydney Eye Hospital from 1995 to 2004. The main outcome measures included post-operative symptomatic relief of presenting symptoms, complications, subjective visibility of any scar, and general satisfaction. Statistical methods included χ2 tests, and Student's t-tests for the comparison of variables among groups.
Results
Ninety-four external, 10 endoscopic primary procedures, and five revision procedures were included. Fifty-six of the cases were primary NLDO, and 48 were secondary NLDO. The mean follow-up was 1.44 years. Average age at surgery was 6.6±4.2 years (mean±SD). Ninety-one eyes needed DCR for the involvement of the lower lacrimal outflow system, and 13 eyes were NLDO associated with congenital punctual/canalicular dysgenesis.
Most of the complications of external DCR were related to Jones tube placement. Five cases (4.8%) needed DCR revision. There was a significantly higher incidence of revision surgery in the non-stented group (P<0.01), and the Jones tube group (P<0.001) as compared with the silicone intubation stent group.
Conclusions
External DCRs have acceptable long-term clinical and cosmetic results, and low post-operative complication rate. Cases with punctal stenosis or those requiring Jones tube insertion are associated with a higher complication rate. Silicone intubation is associated with a lower need for operative revision.
Similar content being viewed by others
Introduction
The most common indication for dacryocystorhinostomy (DCR) in the paediatric age group is congenital nasolacrimal duct obstruction (NLDO). Conservative medical therapy with hydrostatic pressure on the lacrimal sac, topical antibiotics, probing, and silicone intubation if necessary, are usually effective in clearing the obstruction.1, 2, 3, 4, 5, 6 DCR is required only rarely for recalcitrant cases. Other indications for paediatric DCR are traumatic obstructions, punctal/canalicular agenesis; cases associated with other systemic (eg cleft) anomalies, and acquired cases of NLDO.1, 4
In recent years, DCRs in adults have increasingly been performed endoscopically and studies have shown that the success rates of external and endoscopic DCRs have been comparable.7, 8 The reports on endoscopic DCR in children are limited. Recent works have shown favourable results with success rates of 82–88% for endoscopic DCR in children,1, 2, 5, 6, 7 with no added difficulties or differences in the procedure as compared with adults.1 The aetiology of NLDO is mostly different for the paediatric group, and there are some important anatomical differences to consider, including a narrowed nasal cavity.9, 10
The present study is a review of paediatric external and endoscopic DCRs performed to address various etiologies of NLDO and surgical outcome in the paediatric group of a tertiary referral centre.
Materials and methods
A medical record search was conducted for all patients under the age of 16 who underwent DCR for NLDO of different etiologies at our facility over a period of 10 years from 1995 to 2004. One hundred and four operations in 82 patients were identified. Patients lost to follow-up were not included. Patient records were analyzed retrospectively and the following parameters were documented: age at first presentation; age at operation; laterality; the aetiology of the lacrimal obstruction; type of surgery; post-operative success rate, and complications.
Prior surgical treatment of patients with congenital NLDO included probing and syringing usually on at least two occasions and with silicone intubation. The decision was made to proceed to DCR if symptoms persisted following probing and intubation. Probing, syringing and dacryocystography were also performed in NLDO cases with associated syndromes, and where possible in cases of post-traumatic and post-inflammatory obstruction. Computerized tomography was performed in cases following trauma and craniofacial disorders. Surgery was judged to be successful by subjective reporting of either the patient, if older than 16 years of age, or by a parent of the patient. Objective confirmation of free fluorescein flow to the nose and endoscopic osteotomy patency was performed in cases of symptoms or following silicone tube insertion, as they were under general anaesthesia, for stent removal.
A direct telephone survey was performed by two of the authors (JT and AF) at the end of the follow-up period of external DCRs cases to ascertain functional and aesthetic results. Among other questions, either the patient or one of their parents were asked about the post-operative course since the last office visit, post-operative symptoms of epiphora, or signs of infection. They were also asked to assess the visibility of the scar (in cases of external DCR) on a scale of 1 (least) to 5 (greatest), and grade their general satisfaction on a similar scale. The research was approved by the South Eastern Sydney Area Health Service Research Ethics Committee.
Surgical technique
All cases of external DCR were performed by an experienced consultant lacrimal surgeon under hypotensive general anaesthesia. The surgical technique of external DCR are described elsewhere.9, 10 Nasal packing was performed with a combination of lignocaine 4% topical solution (AstraZeneka, North Ride, Australia) with oxymetazoline hydrochloride (0.05%, Drixine Paediatric, Schering-Plough Auckland, New Zealand) pledgetts or with cocaine 4% pledgetts for nasal anaesthesia and vasoconstriction. In cases of canalicular stenosis where more than 8 mm of canaliculus was identified from the punctum, canalicular trephination was performed with silicone stenting, and when it was less than 8 mm, a Jones tube was inserted. Silicone canalicular stenting was performed in some cases with normal canaliculi. The superficial part of the medial canthal tendon and periosteum was reconstituted and then the skin was closed with interrupted fast absorbing catgut 6-0 or polyglactin 6-0. Self-adhesive dressing was taped over the wound.
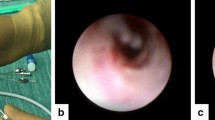
Endoscopic DCR is described in detail elsewhere.11 Intraoperatively systemic antibiotics were given in cases of mucocele, or following lacrimal pathway infection.
Antibiotic ointment and drops were prescribed for ocular use for up to 14 days following surgery. The patients were reviewed in the outpatient clinic one week after surgery, and then according to the history and clinical findings. The patients were assessed for the resolution of preoperative symptoms and signs, and the clinical examination included a fluorescein dye disappearance test, and slit-lamp external examination. Whenever silicone intubation was performed during the operation, tube removal was performed after 6 months, and the patency of the DCR ostium was examined during the procedure of tube removal, which was performed under general anaesthesia for young children. In cases of children of 8 years old or more, it was performed in the office under local anaesthesia when possible.
Associations between categorical variables were analyzed using χ2 tests. Comparison of normally distributed variables among groups was performed using t-tests and analyses of variance. Exact 95% confidence intervals were calculated for the recurrence rates. Analyses were performed using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) and SPSS (SPSS, Inc., Chicago, Illinois, USA).
Results
A total of 104 eyes in 82 patients met the inclusion criteria and were included in this study. There were 42 (51.2%) males, and 40 (48.8%) females (Table 1). The mean follow-up period was 1.44 years (range, 6 months–8 years). External DCR was performed in 94 cases, and endoscopic DCR in 10 cases.
Simultaneous bilateral surgery was performed in one patient, and sequential bilateral surgery in 21 patients. Bilateral operations were performed in 11 of 45 congenital NLD obstruction patients (24.5%), in seven of 10 patients (70%) with associated syndromes, in two of 10 (20%) with punctual atresia, in one of six (16.7%) with acquired obstruction, and in none of the patients with post-trauma obstruction.
Ninety-one eyes in 72 patients needed DCR for the involvement of the lower lacrimal outflow system (the lacrimal sac or duct), and 13 eyes of 10 patients were secondary to congenital punctual/canalicular dysgenesis with associated NLDO. If punctal agenesis was not associated with NLDO, then punctoplasty was performed alone. Nine of these 13 had an external DCR and four had an endoscopic DCR. There were six cases in which a Jones tube was placed, four in which canalicular trephination, and silicone intubation was performed, one case in which canaliculo-DCR (C-DCR), and silicone stenting was performed, one case in which monocanalicular intubation was performed in association with the DCR, and one case in which no tube was inserted.
Ten children had associated systemic syndromes. Of those three had ectrodactyly-ectodermaldysplasia-clefting syndrome, two had oculo-cephalic syndrome, two had associated cleft palate, two had cystic fibrosis, and one had Down's syndrome.
Age at surgery ranged from 11 months to 16 years (mean±SD, 6.6±4.2 years). The age distribution was different for different etiological groups: 3.5±2.1 years for syndrome-associated NLDO; 5.6±3.8 years for congenital obstruction; and 11.6±3.1 years for non-traumatic acquired cases (Table 2).
Silicone stenting was performed in 70 patients, 45 of these were with O'Donoghue silicone rods (Visitec, Sarasota, FL, USA), 22 with fine silicone tubing (0.012 inches internal and 0.025 inches external diameter), and three with Mini-Monoka monocanalicular tubes (FCI, Issy-Les-Moulineaux Cedex, France). Jones tube insertion was performed in 14 cases in which canalicular reconstruction was not possible. In 20 cases with normal canaliculi, no canalicular stent was inserted.
Operative procedures are outlined in Table 2.
Thirty-three percent of admissions (34 of 104) were day cases, while the other 70 admissions were in-patient cases.
Early complications (<6 months post-operatively) were documented in eight (8.8%) cases without Jones tubes. Mild, controlled haemorrhage was observed in four cases, three patients had stent retraction, and one patient had medial trichiasis. Six cases (37.5%) with Jones tubes had early complications involving Jones tubes migration or early blockage. Late complications (6 months or more, postoperatively) included one case of wound infection, and one case of ptosis. Six cases (37.5%) with Jones tubes had late complications: tube extrusion in three cases, and tube loss in three cases. The results of Jones tubes in children are summarized in Table 3.
Objective confirmation of free fluorescein flow was performed in 62 cases, and 59 of them confirmed patency of syringing (95.2%). Five cases (4.8%) needed a DCR revision, two of these being performed endoscopically. Three of five cases which required a revision were secondary to primary congenital NLDO, with no significant difference (P>0.05) from the other indications. Of the other two cases, one had punctal atresia and one had craniofacial syndrome.
Three of the cases requiring a revision DCR followed Jones tube insertion, and two followed cases with normal canaliculi, which did not have silicone stenting. No case having silicone canalicular stenting required a revision. A significant difference regarding the need for revision was found between those groups (Linked variables, P<0.01, χ2=12.99). Both the Jones tube group and the non-intubated cases showed a statistically significant revision rate as compared to the silicone stented group. (P<0.001, χ2=15.34, and P<0.01, χ2=7.1, respectively).
All complications occurred in the external DCR group. No complication or need for revision was observed in the endoscopic DCR group, which comprised only of 10 cases (χ2=0.25, P⩽1).
In the telephone interview, 44 of the external DCRs patients (60.3%) were contactable and interviewed. The mean follow-up post DCR was in this group was 5.2 years (range 1–13 years). The average range of scar visibility (subjective) was 1.79 of five, and the average satisfaction rate was 4.53 of five. The telephone interview results of postoperative symptoms, visibility of the scar, and general satisfaction are outlined in Figure 1.
Discussion
The optimal postoperative course following DCR is the achievement of an asymptomatic eye without epiphora or discharge, and no recurrence in the long-term. Paediatric DCR differs from adult DCR for various reasons. At birth, up to one-third of infants have an underdeveloped tear-duct drainage system, which as a result of blockage, can lead to excess tearing and infection. Some believe that lacrimal surgery is not as successful in children owing to poorly-defined and changing anatomy, rapidly growing facial bone centers and a tendency toward vigorous repair processes producing hyperplastic scar tissue.9
Several series describing outcomes of paediatric lacrimal surgery have been published. Most of these described the surgical outcome in refractory primary congenital NLDO.5, 12, 13 However, a significant percentage of paediatric DCR cases had an aetiology other than congenital NLDO. Previously reported studies of paediatric DCR patients showed that 35–50% of cases were of unresolved congenital NLDO, with the remainder including punctal agenesis, lacrimal fistula, post-traumatic NLDO, and post-inflammatory canalicular obstruction.10, 11, 14 A similar distribution was observed in our series in which 56 cases (54.8%) were of refractory primary congenital NLDO, and the others were of different etiologies. It should be emphasized that underlying pathology, approaches and outcomes of puncta/canaliculi dysgenesis, and lower lacrimal outflow system are quite different . However we included in our study those congenital punctal dysgenesis only with associated NLDO.
External DCR is a very successful operation in adults, with a success rate of 90% or greater in most series.15, 16 The success rate for endonasal DCR (endo-DCR) has been reported as comparable to external DCR by some authors,17, 18, 19, 20 but less successful than external DCR by others.21, 22, 23, 24 The primary procedure success rate in our series was 95.2%. Five of 104 cases needed revision DCR for resolution of symptoms, and 84% of our patients were asymptomatic or had occasionally mild epiphora after the initial procedure. The success rate for the primary procedure of external DCR cases was 93.6% (88 of 94). The primary procedures were successful in 21 of 24 cases with canalicular disease (87.5%), and in 68 of 70 cases without canalicular disease (97.1%). The endo-DCRs were successful in 100% of patients. These figures are comparable to previous paediatric studies of external DCR in children with 90–96% success rates reported.10, 13 Most of the reports of paediatric endo-DCR are of small series.2, 3, 6 However, endo-DCR in children has been reported to be safe with a success rate of 89% or better regardless of age, comparable to that achieved with external DCR and that of endo-DCR in adults.1
The main advantage of external DCR is visualization of the anatomy, allowing precise removal of bone in the lacrimal sac fossa, and accurate suture-fixated anastomosis of the nasal mucosa and lacrimal sac.25 In addition, surgeons are able to excise any membrane covering the opening of the common canaliculus into the sac and can inspect the sac for unexpected pathology.26 In cases of paediatric DCR where bony facial abnormalities are common, the nasal space might be narrow for endoscopic procedures, and an external approach theoretically has the benefit of better visualization of the bony structures to be removed.
The endoscopic surgical route avoids a facial scar, causes less disruption (albeit temporary) of the medial canthal anatomy, may decrease operative time, and may decrease post-operative discomfort. Additionally, it can simultaneously treat any associated nasal pathology,3, 24, 27and can be performed simultaneously on both sides under general anaesthesia as a day procedure. A recent report indicated that despite a narrower nasal cavity in children, removal of bone was relatively easy and no difficulty or difference in the procedure was found in comparison with adults.1 The reported complications were of three cases of operative orbital opening, two cases of postoperative synechiae, seven cases of granulations in the rhinostomy, three cases of premature loss of the silicone stent, and six cases of rhinostomy scarring.1 We did not experience any complications in our endo-DCR cases, however, we had relatively few (10) of these in our overall sample. In our series, all cases which were performed endoscopically were successful and without complications or need for further operations. The lack of statistical significance between the endo-DCR and normal canaliculi external DCR success rate (χ2=0.25, P⩽1), can be attributed to a relatively small endoscopic sampling.
Silicone canalicular-DCR stenting is often used to keep patency of the system and is used preferentially by some surgeons.1, 4, 6 The advantage of stenting is that it secures the patency of the newly created pathway. The disadvantage is the potential for canalicular trauma and subsequent stenosis,10 which we believe is rare, and the need to perform an additional procedure for the removal of the silicone stent, usually requiring general anaesthesia.
Paediatric canalicular NLD silicone stenting without DCR is advocated by many as the procedure of choice following failed probing, and has a success rate of 82–94%.10, 28, 29, 30 The success rate has been reported as being higher for children who undergo surgery between 1 and 4 years of age,30 for patients with no acute dacryocystitis, and for cases of mild obstruction.29
Silicone stenting in paediatric DCR cases is controversial. Hakin et al10 have reported a very high cure rate of 96% for external DCR without canalicular pathology without silicone intubation, and a low complication rate.10 Other authors have advocated the use of silicone stenting for paediatric DCR if both upper and lower canaliculi are present.1, 26
In our series, despite the overall low revision rate, significantly less revisions were needed for cases in which silicone stenting was used. We believe that silicone stenting should be considered for all paediatric DCRs, and is essential in the presence of canalicular disease. Prospective and more cases are needed to conclude that stent usage was responsible for the higher success rate.
Cases involving monocanalicular or bicanalicular obstructions and those with punctal atresia present with added challenges. In such cases, DCR can be performed with recreation of one or both canaliculi by canalicular trephination,26 C-DCR31 or by a retrograde probing from the DCR.32 Many of the cases however, were reported not to have reduction of symptoms using these methods and instead, required a Jones tube insertion in order to achieve the best possible tear drainage.26 Jones tubes have a lower retention rate, are associated with a higher complication rate,33 and have a lower overall success rate in children (79%).10, 13
Previous reports of Jones tubes in adults have shown a 45–50% complication rate.30, 34 These included malposition (18.0%), infection (10.8%), and obstruction (6.3%).30 In a recent study performed by our group, complications occurred eventually in most cases following Jones tube placement in adults such that the tube required replacement, repositioning, or cleaning, with thirty-five percent of the patients reporting tube maintenance to be troublesome.34 It has been reported that patients who have had radiation therapy to the medial canthal area, or those with a history of medial canthal trauma, and resulting scarring, have a higher rate of Jones tube displacement. Radiation therapy slows or prevents the normal tissue contraction that occurs around the Jones tube, and extensive trauma or scar tissue can cause the tube to be hyper mobile for a prolonged period of time.35 Children have a tendency for a vigorous repair process producing scar tissue,11 which may be associated with a more mobile tube and associated migration.
In the present series the majority of complications were related to the presence of a Jones tube, with five cases of early tube migration, and six cases of late tube extrusion or loss. However, the early migration rate of 35.7%, and the late extrusion or loss rate of 21.4% is no higher than that found in the adult group.
We did not find that early or late post-operative complications or the need for DCR revisions were related to the aetiology of the obstruction. Surgical outcomes for indications other than congenital NLDO have been reported to be worse.13 However, our results were comparable for all etiologies (congenital NLDO, secondary to trauma or associated with a systemic or facial anomaly), with the exception of the need for canalicular bypass. Three of five cases which required revision were of primary congenital NLDO, there being no significant difference (P<0.05) from the other indications.
A presence of a cutaneous scar has been reported as the major disadvantage of an external DCR from the patient's perspective.36 In the telephone interview, a low average visibility of scar for external DCR of 1.79 out of five, and a high average satisfaction rate of 4.53 out of five was found. It has been shown recently by our group that only a low percentage of adult patients (10.5%), felt the scarring to be cosmetically significant (>1, on a scale of 1–5) following external DCR.36 The average age of patients with a ‘visible’ scar was less than the average age of patients who reported an ‘invisible’ scar. Using the same scale, we found that for paediatric patients, there was a higher significance of the visibility of scarring noted by patients or their parents, as compared with the elderly group. Previous reports have also found surgical skin scars at other sites to be less prominent in elderly patients, when compared with younger patients.37, 38
There are some limitations for the present study. The need for revision was highest in patients not undergoing silicone stent placement. Possible confounding factors including learning curve effect of DCR surgeries without stents relatively early in the series with use of stents in subsequent patients. The procedures were performed by surgeons using different surgical techniques, and it is thus possible that technical factors beyond the use or lack of use of stents may have influenced the success rates. The phone interview was carried out retrospectively with only a partial response rate.
Our results showed a high success rate in a paediatric lacrimal drainage system/DCR surgery, and that the use of silicone stenting in this group was associated with a higher success rate. Further studies are required to draw definite evidence-based conclusions on the relative efficacy of endo-DCRs vs ext-DCR in paediatric patients.
References
Kominek P, Cervenka S . Pediatric endonasal acryocystorhinostomy: a report of 34 cases. Laryngoscope 2005; 115: 1800–1803.
Cunningham MJ, Woog JJ . Endonasal endoscopic dacryocystorhinostomy in children. Arch Otolaryngol Head Neck Surg 1998; 124: 328–333.
Woog JJ . Endonasal dacryocystorhinostomy. A report by the American academy of ophthalmology. Ophthalmology 2001; 108: 2369–2377.
Freitag SK, Woog JJ . Congenital nasolacrimal obstruction. Ophthalmol Clin North Am 2000; 13: 705–718.
Vanderveen DK, Jones DT, Tan H, Petersen RA . Endoscopic dacryocystorhinostomy in children. J AAPOS 2001; 5: 143–147.
Berlucchi M, Staurenghi G, Brunori P, Tomenzoli D, Nicolai P . Transnasal endoscopic dacryocystorhinostomy for the treatment of lacrimal pathway stenoses in pediatric patients. Int J Pediatr Otorhinolaryngol 2003; 67: 1069–1074.
Sprekelsen MB, Barberan MT . Endoscopic dacryocystorhinostomy: surgical technique and results. Laryngoscope 1996; 106: 187–189.
Weidenbecher M, Hosemann W, Buhr W . Endoscopic endonasal dacryocystorhinostomy: results in 56 patients. Ann Otol Rhinol Laryngol 1994; 103: 363–367.
Nowinski TS, Flanagan JC, Mauriello J . Pediatric dacryocystorhinostomy. Arch Ophthalmol 1985; 103: 1226–1228.
Hakin KN, Sullivan TJ, Sharma A, Welham RAN . Paediatric dacryocystorhinostomy. Aust NZ J Ophthalmol 1994; 22: 231–235.
Tsirbas A, Davis G, Wormald PJ . Mechanical endonasal dacryocystorhinostomy vs external dacryocystorhinostomy. Ophthal Plast Reconstr Surg 2004; 20: 50–56.
Ciftci F, Akman A, Sonmez M, Unal M, Gungor A, Yaylali V . Systematic, combined treatment approach to nasolacrimal duct obstruction in different age groups. Eur J Ophthalmol 2000; 10: 324–329.
Barnes EA, Abou-Rayyah Y, Rose GE . Pediatric dacryocystorhinostomy for nasolacrimal duct obstruction. Ophthalmology 2001; 108: 1562–1564.
Welham R, Hughes SM . Lacrimal surgery in children. Am J Ophthalmol 1985; 99: 27–34.
Benger R . Day-surgery external dacryocystorhinostomy. Aust NZ J Ophthalmol 1992; 20: 243–245.
Duffy MT . Advances in lacrimal surgery. Curr Opin Ophthalmol 2000; 11: 352–356.
McDonogh M . Endoscopic transnasal dacryocystorhinostomy. Results in 21 patients. S Afr J Surg 1992; 30: 107–110.
Dolman PJ . Comparison of external dacryocystorhinostomy with nonlaser endonasal dacryocystorhinostomy. Ophthalmology 2003; 110: 78–84.
Ben Simon GJ, Joseph J, Lee S, Schwarcz RM, McCann JD, Goldberg RA . External vs endoscopic dacryocystorhinostomy for acquired nasolacrimal duct obstruction in a tertiary referral center. Ophthalmology 2005; 112: 1463–1468.
Benger R, Forer M . Endonasal dacryocystorhinostomy–primary and secondary. Aust NZ J Ophthalmol 1993; 21: 157–159.
Metson R, Woog JJ, Puliafito CA . Endoscopic laser dacryocystorhinostomy. Laryngoscope 1994; 104: 269–274.
Hehar SS, Jones NS, Sadiq SA, Downes RN . holmium:YAG laser dacryocystorhinostomy-safe and effective as a day-case procedure. J Laryngol Otol 1997; 111: 1056–1059.
Hartikainen J, Grenman R, Puukka P, Seppa H . Prospective randomized comparison of external dacryocystorhinostomy and endonasal laser dacryocystorhinostomy. Ophthalmology 1998; 105: 1106–1113.
Bakri SJ, Carney AS, Robinson K, Jones NS, Downes RN . Quality of life outcomes following dacryocystorhinostomy: external and endonasal laser techniques compared. Orbit 1999; 18: 83–88.
Yung MW, Hardman-Lea S . Analysis of the results of surgical endoscopic dacryocystorhinostomy: effect of the level of obstruction. Br J Ophthalmol 2002; 86: 792–794.
Cahill KV, Burns JA . Management of epiphora in the presence of congenital punctal and canalicular atresia. Ophthal Plast Reconstr Surg 1991; 7: 167–172.
Malhotra R, Wright M, Olver JM . A consideration of the time taken to do dacryo-cystorhinostomy (DCR) surgery. Eye 2003; 17: 691–696.
Anderson RL, Edwards JJ . Indications, complications and results with silicone stents. Ophthalmology 1979; 86: 1474–1487.
Dortzbach RK, France TD, Kushner BJ, Gonnering RS . Silicone intubation for obstruction of the nasolacrimal duct in children. Am J Ophthalmol 1982; 94: 585–590.
Lim C, Martin P, Benger R, Kourt G, Ghabrial R . Lacrimal canalicular bypass surgery with the lester jones tube. Am J Ophthalmol 2004; 137: 101–108.
Hurwitz JJ, Rutherford S . Computerized survey of lacrimal surgery patients. Ophthalmology 1986; 93: 14–19.
Wearne MJ, Beigi B, Davis G, Rose GE . Retrograde intubation dacryocystorhinostomy for proximal and midcanalicular obstruction. Ophthalmology 1999; 106: 2325–2328.
Klapper SR, Jordan DR . Jones tube insertion in children with canalicular agenesis. Ophthalmic Surg Lasers 1999; 30: 495–498.
Zilelioglu G, Gunduz K . Conjunctivodacryocystorhinostomy with Jones tube. A 10-year study. Doc Ophthalmol 1996-97; 92: 97–105.
Gladstone GJ, Putterman AM . A modified glass tube for conjunctivodacryocystorhinostomy. Arch Ophthalmol 1985; 103: 1229–1230.
Sharma V, Martin PA, Benger R, Kourt G, Danks JJ, Deckel Y et al. Evaluation of the cosmetic significance of external dacryocystorhinostomy scars. Am J Ophthalmol 2005; 140: 359–362.
Booth AJ, Murray A, Tyers AG . direct brow lift: efficacy, complications, and patient satisfaction. Br J Ophthalmol 2004; 88: 688–691.
Kearney CR, Holme SA, Burden AD, McHenry P . Long-term patient satisfaction with cosmetic outcome of minor cutaneous surgery. Australas J Dermatol 2001; 42: 102–105.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial interest in any of the materials used in this study
The addresses of the institutions at which the work was carried out: Department of Ophthalmology, Sydney Hospital and Sydney Eye Hospital, Macquarie Street, Sydney, NSW 2000, Australia
Rights and permissions
About this article
Cite this article
Nemet, A., Fung, A., Martin, P. et al. Lacrimal drainage obstruction and dacryocystorhinostomy in children. Eye 22, 918–924 (2008). https://doi.org/10.1038/sj.eye.6702769
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702769
Keywords
This article is cited by
-
Minimalinvasive Diagnostik und Therapie der konnatalen Tränenwegsstenose
Der Ophthalmologe (2017)
-
Konnatale Dakryostenose bei Persistenz der Hasner-Membran
Monatsschrift Kinderheilkunde (2017)
-
Pediatric endocanalicular diode laser dacryocystorhinostomy: results of a minimally invasive surgical technique
European Archives of Oto-Rhino-Laryngology (2011)