Abstract
Disturbances in the serotonin (5-HT) system are associated with various neuropsychiatric disorders. The 5-HT system can be studied in vivo by measuring 5-HT transporter (SERT) densities using 123iodine-labeled 2β-carbomethoxy-3β(4-iodophenyl)tropane ([123I]β-CIT) and single photon emission computed tomography (SPECT). Validation of this technique is important because [123I]β-CIT does not bind selectively to SERTs. Some studies have validated this technique in vivo in the human brain in SERT-rich areas, but the technique has not been validated yet in SERT-low cortical areas. The aim of this study was to further validate [123I]β-CIT SPECT in assessing SERTs in vivo in humans in both SERT-rich and SERT-low areas. A double-blind, placebo-controlled, crossover design was used with the selective 5-HT reuptake inhibitor (SSRI) citalopram. Six male subjects underwent two [123I]β-CIT SPECT sessions: one after pretreatment with citalopram and one after placebo. Scans were acquired 4 h and 22–27 h p.i., and both region-of-interest and voxel-by-voxel analyses were performed. Citalopram reduced [123I]β-CIT binding ratios in SERT-rich midbrain and (hypo)thalamus. Binding ratios were also lower after citalopram in SERT-low cortical areas, but statistical significance was only reached in several cortical areas using voxel-by-voxel analysis. In addition, citalopram increased binding ratios in the DAT-rich striatum and increased absolute uptake in the cerebellum. The results show that [123I]β-CIT SPECT is a valid technique to study SERT binding in vivo in human brain in SERT-rich areas. Although we provide some evidence that [123I]β-CIT SPECT may be used to measure SERTs in SERT-low cortical areas, these measurements must be interpreted with caution.
Similar content being viewed by others
INTRODUCTION
Nowadays, it is possible to study the serotonergic system in the living human brain by visualizing the serotonin (5-HT) transporter (SERT) at the terminus of the 5-HT axon. The SERT is a plasma membrane and a structural element of the presynaptic membrane of the 5-HT axon. Therefore, it is used as a reliable marker for the 5-HT axon (Scheffel et al, 1992). SERT density can be assessed using a radioligand that binds to SERT in combination with positron emission tomography (PET) or single photon emission computed tomography (SPECT).
The serotonergic system modulates many neuropsychological processes, such as mood and memory, through the neurotransmitter 5-HT. Disturbances in the 5-HT system are associated with neuropsychiatric disorders including depression, eating disorders, and Alzheimer's disease (Lucki, 1998; Wenk, 2003). There is also evidence that the popular recreational drug ecstasy (3,4-methelenedioxymethamphetamine, MDMA) causes damage to the 5-HT axons both in animals (eg Hatzidimitriou et al, 1999; Ricaurte et al, 2000) and humans (Gerra et al, 1998; Kish et al, 2000). The use of ecstasy is associated with decreased memory function and increased symptoms of depression (Parrott, 2000; Verbaten, 2003; Thomasius et al, 2003). SERT is also the primary site of action for selective 5-HT reuptake inhibitors (SSRIs), the most frequently prescribed antidepressants. Therefore, visualization and quantification of SERT is important for studying neuropsychiatric disorders in which the serotonergic system is involved and for studying occupancy of SERTs by SSRIs in vivo.
One of the SPECT ligands that is used for studying SERTs is 123iodine-labeled 2β-carbomethoxy-3β(4-iodophenyl)tropane ([123I]β-CIT), a cocaine derivate that binds with high affinity to SERTs and dopamine transporters (DATs) (Laruelle et al, 1993). The use of [123/125I]β-CIT in visualizing SERTs and DATs has been validated in vitro and ex vivo in rodents (Boja et al, 1992; Scheffel et al, 1992; Lew et al, 1996; Reneman et al, 2002) and in human brain slices (Staley et al, 1994). In addition, in vivo displacement studies in monkeys demonstrated that binding in the hypothalamus and midbrain was mainly associated with binding to SERTs, while binding in the striatum was mainly associated with binding to DATs (Laruelle et al, 1993). Therefore, it may be possible with [123I]β-CIT SPECT to study both SERT and DAT densities in anatomical separated areas.
In humans, in vivo [123I]β-CIT SPECT imaging of the SERT has been used, among others, to study SERT availability in depression and alcoholism and to study the neurotoxic effects of ecstasy (Malison et al, 1998; Heinz et al, 1998; Reneman et al, 2001a, 2001b). However, because [123I]β-CIT does not bind selectively to SERTs, but also to DATs and norepinephrine transporters, there are some difficulties in using [123I]β-CIT SPECT for studying SERT binding in vivo. Therefore, it is important to validate in which brain areas [123I]β-CIT can be accurately used to study SERTs. Although several studies used [123I]β-CIT SPECT to assess SERTs in vivo in humans, validation of this technique has been limited.
First, a limited number of studies have been performed to validate the use of [123I]β-CIT SPECT for studying SERTs in vivo in humans (Pirker et al, 1995, 2000) or to study the effects of [123I]β-CIT binding to SERTs and DATs in vivo in humans after blocking of SERTs with a SSRI (Pirker et al, 1995; Tauscher et al, 1999; Kugaya et al, 2003). One study validated the use of in vivo [123I]β-CIT SPECT in detecting MDMA-induced serotonergic neurotoxicity in SERT-rich brain areas in a monkey (Reneman et al, 2002).
Second, previous SSRI displacement studies did not validate the in vivo [123I]β-CIT binding to SERTs in cortical regions, probably because the interpretation in these areas is hampered by low SERT and DAT densities (Cortés et al, 1988; Bäckström et al, 1989; Heinz and Jones, 2000). Since studies in non-human primates showed long-term and possible irreversible damage of serotonergic axons in the cerebral cortex induced by MDMA (Hatzidimitriou et al, 1999), assessment of SERT density in the cerebral cortex is especially important for studying the neurotoxic effects of ecstasy. Reductions of SERT densities in cortical brain regions were reported in male (Semple et al, 1999) and female (Reneman et al, 2001b) ecstasy users. However, others discussed these results because of the presumed limited sensitivity of [123I]β-CIT SPECT imaging to measure SERT density in the cerebral cortex (Heinz and Jones, 2000; Ricaurte and McCann, 2001; Kish, 2002).
Third, previous validation studies have been limited by some methodological weaknesses. Some of these studies were performed in depressed patients, whereas depression may be an important confounder. For example, lower [123I]β-CIT binding ratios were reported in SERT-rich areas in depressed patients treated with SSRIs compared to healthy volunteers (Pirker et al, 1995; Tauscher et al, 1999), whereas also in untreated depressive patients decreased SERT binding has been described (Malison et al, 1998). Only Kugaya and co-workers (2003) studied the in vivo alterations of [123I]β-CIT binding during SSRI treatment in both depressive patients and in healthy volunteers. To our knowledge, no validation studies have been performed yet in the same healthy subjects before and after SSRI treatment.
The purpose of the present study was to further validate the technique of [123I]β-CIT SPECT to assess SERTs in vivo in humans in both SERT-rich and SERT-low brain areas using the most optimal study design. Therefore, a double-blind, placebo-controlled, crossover design with the most selective SSRI citalopram was used to study the binding of [123I]β-CIT to SERTs and DATs in SERT-rich, DAT-rich and in SERT-low cortical brain regions. As citalopram selectively blocks SERTs, we hypothesized that [123I]β-CIT binding ratios would decrease in both SERT-rich areas and in SERT-low cortical areas after pretreatment with citalopram.
MATERIALS AND METHODS
Subjects
Six healthy male volunteers were included in the present study between November 2002 and May 2003. They were recruited by means of posters at the Faculty of Medicine of the University of Amsterdam, The Netherlands. Exclusion criteria were age below 18 or above 35 years, major mental or physical problems, use of psychopharmaceuticals such as SSRIs, and use of hard drugs such as ecstasy, cocaine, amphetamine, or heroine in the past. All volunteers had to complete the Beck Depression Inventory (BDI; Beck et al, 1961), a validated depression questionnaire, before each imaging session to exclude depression. Participant with a BDI⩾10 were excluded. Written informed consent was obtained from all subjects and the study was approved by the local medical ethics committee.
Study Procedure
We used a double-blind, placebo-controlled, crossover design to study the effect of the SSRI citalopram on binding of [123I]β-CIT to SERTs and DATs. Therefore, all six subjects participated in two different sessions with an interval of 4–6 weeks between both sessions. At 3 h before injection with [123I]β-CIT, the subjects were given a capsule with either 20 mg of the most selective SSRI citalopram (Johnson, 1991) or a placebo that had to be taken orally under supervision of the examiner. Both volunteer and examiner were blinded for the content of the capsule. At 3 h after intake of the capsule, [123I]β-CIT was injected. Per session two SPECT scans were acquired, 4 h post-injection (p.i.) as well as 22–27 h p.i., when stable uptake to the SERTs and DATs is expected to be reached, respectively (Laruelle et al, 1994; Pirker et al, 2000). After 4–6 weeks, the procedure was repeated and subjects who were given citalopram in the first session got placebo in the second session, and vice versa.
[123I]β-CIT SPECT Imaging
Subjects were examined using SPECT with the radioligand [123I]β-CIT that binds to SERTs, DATs, and, in a lesser extent, also to norepinephrine transporters. Radiosynthesis of [123I]β-CIT was performed by electrophilic radioiododestannylation of the trimethyltin precursor (RadioNuclide Center, Vrije Universiteit Amsterdam, The Netherlands), with carrier-free [123I] as NaI (BV Cyclotron, Vrije Universiteit) in the presence of peracetic acid as oxidant. After labeling, the product was further purified with HPLC separation, diluted, and sterile filtrated to an injectable solution with a radioactive concentration of 55–60 MBq/ml. The radiochemical purity of the solution was higher than 99.5%. At both sessions, 112 MBq (3.02 mCi) [123I]β-CIT was injected intravenously as a bolus. Subjects received a potassium iodide solution to block thyroid uptake of free radioactive iodide.
SPECT studies were performed using a 12-detector single slice brain-dedicated scanner (Neurofocus 810, which is an upgrade of the Strichmann Medical Equipment) with a full-width at half-maximum resolution of approximately 6.5 mm, throughout the 20 cm field-of-view (http://www.neurophysics.com). After positioning of the subjects with the head parallel to the orbitomeatal line, axial slices parallel and upward from the orbitomeatal line to the vertex were acquired in 5 mm steps. Each acquisition consisted of approximately 15 slices with 3 min scanning time per slice, acquired in a 64 × 64 matrix. The energy window was set at 135–190 keV.
Image Reconstruction and Analysis
Attenuation correction of all images was performed as described earlier (Booij et al, 1997). Images were reconstructed in 3D mode (http://www.neurophysics.com). For quantification, both region-of-interest (ROI) and voxel-by-voxel analyses were performed.
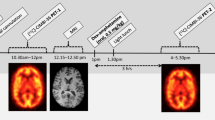
Standardized templates of 2D ROIs were drawn with the help of a high-resolution MRI and a brain atlas. For the SPECT scans 4 h p.i., ROIs for the midbrain, (hypo)thalamus, frontal cortex, temporal cortex, occipital cortex, and cerebellum were used. For the SPECT scan 22–27 h p.i., ROIs for the striatum and cerebellum were used. The ROIs were positioned on the SPECT slices by the same examiner who was blinded for the content of the pretreatment (Figure 1). For the right and left striatum, a template with irregular ROIs, according to the contour of the putamen and caudate nucleus, was positioned on four consecutive axial slices with highest striatal activity. Individual variation required movement of the fixed ROIs, without changing size and shape, within the template for optimal fitting. For the frontal, right occipital, and left occipital cortices, irregular ROIs were drawn in one template. The template was positioned on four consecutive slices: on the three superior slices where the striatal ROIs were positioned and on one slice above. We defined the inferior level of the (hypo)thalamus to correspond with the inferior level of the striatum. For the (hypo)thalamic area, a template with an oval-shaped ROI was placed on four SPECT slices with the highest (hypo)thalamic activity. The superior level of the midbrain was defined to coincide with the most superior slice without visible striatal activity. For this midbrain area, a template with a round-shaped ROI was placed on four SPECT slices with the highest activity of the midbrain. For the cerebellum, a template with an irregular-shaped ROI was positioned on three SPECT slices with highest cerebellar activity. A template with irregular ROIs for right and left temporal cortex was placed on the two most superior slices where the cerebellum template was positioned. Mean striatal, mean temporal, and mean occipital binding densities were averaged from right and left ROIs. Mean cortical binding was calculated as the mean counts per voxel from the frontal, temporal, and occipital cortex together. Absolute uptake in the cerebellum was defined as the mean activity within the ROI of the cerebellum divided by the injected dose (Bq/ml/MBq). Activity in the cerebellum was assumed to represent nondisplaceable activity (nonspecific binding and free radioactivity). Specific to nonspecific binding ratios were calculated as (activity in ROI−activity in cerebellum)/activity in cerebellum.
[123I]β-CIT SPECT images with ROI templates of cerebellum (1), right temporal cortex (2), left temporal cortex (3), midbrain (4), frontal cortex (5), right occipital cortex (6), left occipital cortex (7), right striatum (8), and left striatum (9). Images a and b are 4 h p.i. and image c is 24 h p.i. The level of radioactivity is color encoded from low (black) through medium (yellow) to high (white) and scaled to the maximum of the study. To visualize low specific binding to SERTs in images a and b, the upper threshold was set at approximately 25% of the maximum of the study.
For the voxel-by-voxel analysis, Statistical Parametric Mapping software (SPM 99, welcome of Cognitive Neurology, Institute of Neurology, London, UK; www.fil.ion.ucl.ac.uk/spm) implemented in matlab (Mathworks, Sherborn, MA, USA) was used (Friston et al, 1995). All SPECT images were spatially normalized by a linear coregistration to a standard stereotaxic space (Talairach and Tournoux, 1988). Subsequently, the images were intensity scaled to the corresponding mean cerebellar nonspecific counts per voxel. The mean cerebellar counts were obtained from the ROI analysis.
Statistical Analysis
Differences in binding densities in ROIs between citalopram and placebo pretreatment were analyzed using a two-sided Student's t-test for paired samples. The Kolmogorov–Smirnov test was used to analyze whether data were normally distributed. Statistical significance was defined as p<0.05. Statistical analyses were performed using SPSS 11.5.
Based on the coregistered images, statistical parametric maps of the paired t-statistics SPM{T} were calculated and transformed to the unit normal distribution SPM{Z}. Only clusters of connected voxels above an extent threshold of 20 voxels (voxel threshold was set at p<0.01, Z-score=2.33, uncorrected for multiple comparisons) were tested for significance by means of spatial extent statistical theory (Worsley et al, 1992; Friston et al, 1996). Clusters of voxels surviving the thresholds were color coded and superimposed on reference images.
RESULTS
Mean age of the subjects was 24.0±4.3 years (range 18.7–31.2 years). Mean BDI scores were 1.3±2.3 (range 0–6) at placebo session and 1.3±1.9 (range 0–5) at citalopram session. As BDI scores between 0 and 9 are regarded within the normal range, none of the subjects had clinical depression.
ROI Analysis
Data from the ROI analysis were normally distributed. The individual and mean absolute uptake in the cerebellum and the individual and mean uptake ratios within ROIs are described in Table 1. Figure 2 shows a representative sagittal slice of the activity uptake in the midline 4 h p.i. after placebo pretreatment (a) and after citalopram pretreatment (b). Absolute nonspecific cerebellar activity was significantly higher after citalopram pretreatment than after placebo intake 4 h, but not 24 h p.i. Binding ratios of [123I]β-CIT 4 h p.i. were significantly lower after citalopram intake than after placebo intake in the SERT-rich midbrain (p=0.009) and (hypo)thalamus (p=0.001). [123I]β-CIT binding ratios 4 h p.i. were also lower after citalopram intake than after placebo intake in the SERT-low temporal, frontal, and occipital cortical areas, although these findings did not reach statistical significance (p=0.055, 0.088, and 0.340, respectively). The calculated mean cortical binding ratio was also not significantly different between the two sessions (p=0.124). The binding ratio in the DAT-rich striatum 22–27 h p.i. was significantly higher (p=0.009) after citalopram intake than after placebo intake.
Voxel-by-Voxel Analysis
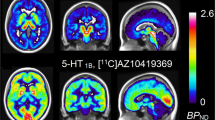
Voxel-by-voxel analysis of the scans made 4 h p.i. showed clusters of significantly lower [123I]β-CIT binding ratios in the SERT-rich midbrain and thalamus (Zmax=4.45, pcluster level=0.000) after pretreatment with citalopram. Clusters of significantly decreased binding ratios after citalopram pretreatment were also found in several SERT-low (mainly) cortical areas, for example, subcortical insula, left and right middle- and superior temporal gyrus, inferior frontal gyrus, and postcentral gyrus (Zmax=4.20, pcluster level=0.000), right middle- and superior frontal gyrus (Zmax=3.74, pcluster level=0.047) and anterior cingulate (Zmax=4.88, pcluster level=0.004) (Figure 3a). Analysis of the scans 22–27 h p.i. showed a cluster of significantly lower binding ratios in the midbrain/thalamus area (Zmax=3.53, pcluster level=0.000) after citalopram pretreatment (Figure 3b) and increased binding ratios in the DAT-rich left caudate nucleus (Zmax=3.32, pcluster level=0.000) (Figure 3c).
Clusters of significant different binding ratios after voxel-by-voxel analysis with citalopram pretreatment compared to placebo pretreatment, superimposed on reference images. Image a shows 4 h p.i lower binding ratios in subcortical (insula, midbrain, and thalamus) and in several cortical areas (eg middle- and superior temporal gyrus, inferior-, middle-, and superior frontal gyrus, anterior cingulate, and postcentral gyrus). The clusters high on the sagittal slice are related to the upper boundary of the field of view and are likely to represent artifacts rather than real significant differences in [123I]β-CIT binding ratios. Image b shows lower binding ratios in the midbrain/(hypo)thalamus area and image c shows increased binding ratio in the left caudate nucleus 22–27 h p.i.
DISCUSSION
To our knowledge, this is the first study that validated the use of [123I]β-CIT SPECT to assess SERTs in vivo in the human brain using a double-blind and placebo-controlled design in which the same healthy volunteers were examined with and without pretreatment with the most selective SSRI citalopram. The potential confounders age, gender, and depression were excluded because we only included men within a small age range without depression. Although [123I]β-CIT SPECT is currently not used as a diagnostic tool to assess SERT densities, validation of this technique is important because a valid technique would make it possible to study adequately the serotonergic system in vivo in several diseases such as mood disorders, Parkinson's disease, eating disorders, alcoholism, and MDMA neurotoxicity. Moreover, [123I]β-CIT SPECT could be used to evaluate the occupancy of SERTs by medication such as SSRIs.
In the present study, we measured (with ROI analyses) [123I]β-CIT uptake ratios for SERT binding 4 h p.i., although kinetic studies showed that in SERT-rich areas binding ratios were closer to a state of transient equilibrium between 20 and 24 h p.i. than 4 h p.i. (increase in binding ratios in the midbrain of 5.5±3.9%/h vs 2.5±5.3%/h at 4–10 h p.i. and 20–24 h p.i., respectively) (Pirker et al, 2000). As the differences were small and because several studies reported stable uptake in the (hypo)thalamus, midbrain, cerebral cortex, and cerebellum at 4 h p.i. (Brücke et al, 1993; Pirker et al, 1995), it was suggested that both time points are reliably for measurements of SERTs with [123I]β-CIT (Pirker et al, 2000). Moreover, as the count statistics are better 4 h than 24 h p.i., leading to better visibility especially of the SERT-low cortical areas, it would be likely that measurements of SERT binding 4 h p.i. have better test–retest reliability than measurements of SERT binding 24 h p.i., although we did not study this.
The most important results of our study are that [123I]β-CIT binding ratios were lower in SERT-rich as well as in SERT-low areas (although only statistically significant with voxel-by-voxel analysis and not with ROI analysis) and higher in the DAT-rich striatum after pretreatment with citalopram compared to placebo. Moreover, we found that citalopram increased the absolute [123I]β-CIT in the SERT- and DAT-low cerebellum. These results will be discussed in detail in the following paragraphs.
First, in the SERT-rich midbrain and (hypo)thalamus, [123I]β-CIT binding significantly decreased with 72 and 58%, respectively (ROI analysis), after pretreatment with citalopram. This corroborates previous findings of in vivo studies in humans, which showed that citalopram significantly inhibited [123I]β-CIT binding to SERTs in the brainstem and diencephalon (Pirker et al, 1995; Kugaya et al, 2003). Human PET studies using the SERT-selective radiotracer [11C]DASB also showed high occupancy of SERTs in the midbrain and thalamus after (sub)therapeutic doses of various SSRIs (Meyer et al, 2004). In addition, previous studies in animals showed that [123I]β-CIT binds to SERTs in these brain areas (Laruelle et al, 1993). Decreased binding of [123I]β-CIT to SERTs after pretreatment with citalopram could be caused by decreased availability of SERTs due to blockage of SERTs by citalopram, by downregulation of the SERT protein, by a change in affinity of [123I]β-CIT for the SERT, or by a combination of these factors. Benmansour et al (2002) showed that marked loss of SERT binding sites due to downregulation occurred in rats only after 10–15 days of SSRI treatment. Therefore, we think it is not likely that SERT downregulation in our subjects occurred within one day after only one dose of citalopram. However, downregulation of SERT proteins may play a role in subjects who have taken SSRI treatment for a longer period in other studies. Although we cannot exclude that SSRIs induce fast changes in the affinity of [123I]β-CIT for SERTs, the presently observed decreased binding of [123I]β-CIT in SERT-rich brain areas after citalopram pretreatment is most likely explained by acute blockage of SERT binding sites.
Second, besides a decrease in [123I]β-CIT binding in SERT-rich areas, we also found a decrease in [123I]β-CIT binding ratios in SERT-low cortical areas after pretreatment with citalopram. Voxel-by-voxel analysis showed clusters of significant decreases within several cortical areas. Using ROI analysis, the decreases in cortical binding did not reach the level of statistical significance, possibly because of low statistical power. Reduction of [123I]β-CIT binding after SSRI pretreatment has also been shown in the prefrontal cortex of rats (Scheffel et al, 1992). Moreover, autoradiographic studies of human brain sections showed that citalopram, but not the selective norepinephrine reuptake blocker desipramine or the selective DAT blocker GBR12909, was capable to displace cortical binding of the PET ligand [11C]β-CIT (Farde et al, 1994). In addition, significant reductions of [123I]β-CIT binding ratios were observed in various cortical areas of rats after pretreatment with MDMA, which is considered to be a selective neurotoxin for serotonergic neurons (Reneman et al, 2002). In line with this, [123I]β-CIT SPECT studies in human ecstasy users showed reductions of SERTs in cortical brain regions (Semple et al, 1999; Reneman et al, 2001a, 2001b). These findings suggest that [123I]β-CIT binding in the cerebral cortex is predominantly caused by binding to SERTs. However, other studies were not able to show that [123I]β-CIT binds to cortical SERTs (Laruelle et al, 1993) or did not study this issue (Pirker et al, 1995; Kugaya et al, 2003). In addition, a SSRI displacement study with the SERT-selective PET radioligand [11C]McN 5652 in non-human primates also failed to show specific binding in the cerebral cortex (Parsey et al, 2000). Finally, studies showed in rats (Scheffel et al, 1992) and in post-mortem human brains (Günther et al, 1997) that cortical [123I]β-CIT binding was mainly blocked by citalopram, and to a lesser extent also by selective DAT and norepinephrine reuptake inhibitors. Therefore, using the radiotracer [123I]β-CIT, it will be very difficult to distinguish between SERT and DAT binding in the cortical areas and this would only be possible when selective blockers for DAT and norepinephrine transporter are used simultaneously. As expected, we found much lower [123I]β-CIT binding ratios in the cortex than in the midbrain and (hypo)thalamus, because the SERT concentration is much lower in the cerebral cortex than in the midbrain or diencephalon (Cortés et al, 1988; Bäckström et al, 1989). These low binding densities and corresponding low signal-to-noise ratios cause poor visualization and delineation by which placement of ROI templates in the cerebral cortex is hampered. Owing to these arguments, we think that measurement of SERT in the cortical areas using [123I]β-CIT must be interpreted with caution, although SPM data provide evidence that [123I]β-CIT most likely binds to SERTs in specific SERT-low brain regions such as the temporal and frontal cortex. More selective SERT ligands for SPECT imaging, such as the recently developed [123I]ADAM with a 1000-fold greater selectivity to SERTs than to norepinephrine transporters or DATs (Oya et al, 2000), will probably be more sensitive to the detection of decreased SERT availability in the cortical areas.
Third, in contrast to a decreased binding to SERTs, we observed an increased binding of [123I]β-CIT in the DAT-rich striatum 22–27 h p.i. after pretreatment with citalopram compared to placebo. From other studies, it is known that SERTs are highly expressed in human lungs and that SSRIs accumulate in here (Suhara et al, 1998). Additionally, human biodistribution studies with [123I]β-CIT showed intense binding in the lungs, liver, and lower large intestine (Seibyl et al, 1994). It is therefore likely that peripheral blockage of SERTs by citalopram has resulted in increased tracer availability in the brain. However, kinetic studies showed that the specific binding of [123I]β-CIT to DATs in human brain is stable 20–30 h p.i. and the kinetic model predicts that both specific and nonspecific binding would increase in the same proportion (Laruelle et al, 1994). Therefore, it is not expected that a change in radiotracer availability would influence the striatal binding ratio. On the other hand, the finding of increased striatal activity after the administration of SSRIs was also observed in several other studies in animals (Scheffel et al, 1994; Szabo et al, 2002) and in humans (Tauscher et al, 1999; Kugaya et al, 2003). Kugaya et al (2003) suggested that the increase might be caused by interaction between 5-HT and dopamine systems. Scheffel et al (1994) suggested that pretreatment with SSRIs would cause displacement of the radiotracer from peripheral and central SERTs, and that this would lead to an increased availability of radiotracer for binding to DATs. In accordance with Scheffel et al (1994), we hypothesize that the combination of increased tracer availability (due to peripheral SERT blockage) and decreased SERT availability (due to central SERT blockage) in the brain might have led to increased availability of the tracer for binding to DATs, consequently leading to the observed increased uptake ratio in the DAT-rich striatum when compared to the DAT-devoid reference area of the cerebellum. Although the underlying mechanism is debatable, the finding deserves attention in future studies. This is, for example, of importance because [123I]β-CIT SPECT studies are performed frequently to measure striatal DATs in parkinsonian patients, and such patients quite often use SSRIs.
Fourth, we observed an increase of absolute cerebellar binding after pretreatment with citalopram, 4 h p.i. This increased binding was probably also caused by increased availability of radiotracer in the brain. Szabo et al (2002) reported a strong increase of brain uptake of the selective SERT tracers [11C]DASB and [11C]McN5652 in baboons treated with the SSRI paroxetine. The authors suggested that this finding was caused by a combination of a decreased peripheral binding to SERTs and a paroxetine-induced reduction of the metabolism of both radiotracers. In our study, we did not measure the influence of citalopram on the metabolism of [123I]β-CIT. Although in literature there are no indications that SSRIs influence the metabolism of [123I]β-CIT, we cannot exclude this as a cause of enhanced brain uptake. We believe it is more likely, however, that blockage of peripheral SERTs by citalopram has led to an increased absolute brain uptake (including increased nonspecific cerebellar uptake) of [123I]β-CIT, although Farde et al (1994) did not observe a change in cerebellar activity of the PET ligand [11C]β-CIT after the administration of citalopram. This discrepancy emphasizes the need for more studies on the influence of SSRIs on metabolism and on binding of SERT radiotracers to central as well as peripheral SERTs. It is not likely that binding ratios have been affected by the increased cerebellar uptake, because the binding ratios are considered to be stable 4 h p.i. (Brücke et al, 1993; Pirker et al, 1995, 2000). Therefore, increased tracer availability would increase both specific and nonspecific (cerebellar) binding in the same proportion. This means that the presently observed lower binding ratios in SERT-rich and cortical areas after citalopram presumably reflect blocking of specific binding to SERTs.
In contrast to the above-mentioned increased absolute cerebellar uptake of SERT radiotracers after pretreatment with SSRIs, pretreatment with the selective 5-HT neurotoxin MDMA significantly decreased cerebellar uptake of activity in the same study of Szabo et al (2002) and in a study with rats using the radioligand [123I]β-CIT (De Win et al, 2004). Since the cerebellum is not devoid of SERTs (Cortés et al, 1988; Bäckström et al, 1989), this might be explained by an MDMA-induced decreased availability of SERTs in the cerebellum. Both SSRI and MDMA pretreatment could be used to evaluate the specificity of radiotracer binding to SERTs. However, the contrasting findings on cerebellar (nonspecific) binding emphasize that results from different studies should be interpreted with caution, because differences in binding may not solely reflect blockage of binding from specific central binding sites. In case of measuring MDMA-induced neurotoxicity, it has been advocated to use specific to nonspecific ratios, with the cerebellar binding as an adequate estimate of nonspecific binding. As specific binding ratios are calculated by the formula ((activity in ROI−activity in cerebellum)/activity in cerebellum), MDMA-induced loss of cerebellar SERT binding might lead to an overestimation of SERT density and thus an underestimation of the presumably neurotoxic effects of MDMA. Therefore, it has been suggested that the specific to nonspecific SERT binding ratios may not be optimal (Szabo et al, 2002).
Finally, although the present study was performed using a crossover study design in which subjects were their own controls, the relatively small group of subjects may have resulted in a limited statistical power, especially with regard to the [123I]β-CIT binding in SERT-low cortical areas with its limited signal-to-noise ratios. Moreover, due to the low specific to nonspecific binding ratios in the cortical areas, one may expect that the test reliability is lower in these areas than in areas with high SERT densities. However, because of the radiation exposure, we could not perform test–retest measurements to determine test reliability. The accuracy of this study would probably have been improved by coregistration of the SPECT images with MRI. Also, we did not check levels of citalopram in blood samples, although we supervised the intake of the citalopram or placebo capsule.
In conclusion, our results provide evidence that [123I]β-CIT SPECT is a valid technique to study SERTs in vivo in humans in SERT-rich brain areas, as binding ratios significantly decreased by pretreatment with the selective SSRI citalopram. In addition, we show that [123I]β-CIT also seems to bind to SERTs in SERT-low brain regions, such as the temporal and frontal cortex. Owing to the very low specific binding in these areas, statistical significant changes in specific binding ratios due to citalopram were only detectable with a voxel-by-voxel analysis, and, therefore, in vivo measurements with [123I]β-CIT SPECT in cortical areas must be interpreted with caution. In addition, pretreatment with citalopram caused increased binding ratios in the DAT-rich striatum and increased absolute uptake in the cerebellum. More studies, especially in humans, are needed to evaluate the accuracy of the use of cerebellar binding to estimate nonspecific binding. Finally, in near future, this study needs to be repeated with SPECT radiotracers, which are more selective for SERTs than [123I]β-CIT, to investigate whether the selective radiotracers are more sensitive to assess SERTs in, especially, SERT-low brain areas.
References
Bäckström I, Bergström M, Marcusson J (1989). High affinity [3H]paroxetine binding to serotonin uptake sites in human brain tissue. Brain Res 486: 261–268.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961). An inventory for measuring depression. Arch Gen Psychiatry 4: 561–571.
Benmansour S, Owens WA, Cecchi M, Morilak DA, Frazer A (2002). Serotonin clearance in vivo is altered to a greater extent by antidepressant-induced downregulation of the serotonin transporter than by acute blockade of this transporter. J Neurosci 22: 6766–6772.
Boja JW, Mitchell WM, Patel A, Kopajtic TA, Carroll FI, Lewin AH et al (1992). High-affinity binding of [125I]RTI-55 to dopamine and serotonin transporters in rat brain. Synapse 12: 27–36.
Booij J, Tissingh G, Boer GJ, Speelman JD, Stoof JC, Janssen AG et al (1997). [123I]FP-[CIT SPECT shows a pronounced decline of striatal dopamine transporter labelling in early and advanced Parkinson's disease. J Neurol Neurosurg Psychiatry 62: 133–140.
Brücke T, Kornhuber J, Angelberger P, Asenbaum S, Frassine H, Podreka I (1993). SPECT imaging of dopamine and serotonin transporters with [123I]β-CIT. Binding kinetics in the human brain. J Neural Transm Gen Sect 94: 137–146.
Cortés R, Soriano E, Pazos A, Probst A, Palacios JM (1988). Autoradiography of antidepressant binding sites in the human brain: localization using [3H]imipramine and [3H]paroxetine. Neuroscience 27: 473–496.
De Win MML, de Jeu RAM, de Bruin K, Habraken JBA, Reneman L, Booij J et al (2004). Validity of in vivo [123I]β-CIT SPECT in detecting MDMA-induced neurotoxicity in rats. Eur Neuropsychopharmacol 14: 185–189.
Farde L, Halldin C, Müller L, Suhara T, Karlsson P, Hall H (1994). PET study of [11C]β-CIT binding to monoamine transporters in the monkey and human brain. Synapse 2: 93–103.
Friston KJ, Holmes AP, Poline JB, Price CJ, Frith CD (1996). Detecting activation in PET and fMRI: levels of inference and power. Neuroimage 4: 223–235.
Friston KJ, Holmes AP, Worsley KJ, Poline JB, Frith CD, Frakowiak RSJ (1995). Statistical parametric maps in functional imaging: general approach. Hum Brain Mapp 2: 189–210.
Gerra G, Zaimovic A, Giucastro G, Maestri D, Monica C, Sartori R et al (1998). Serotonergic function after (±)3,4-methylene-dioxymethamphetamine (‘ecstasy’) in humans. Int Clin Psychopharmacol 13: 1–9.
Günther I, Hall H, Halldin C, Swahn CG, Farde L, Sedvall G (1997). [125I]β-CIT-FE and [125I]β-CIT-FP are superior to [125I]β-CIT for dopamine transporter visualization: autoradiographic evaluation in the human brain. Nucl Med Biol 24: 629–634.
Hatzidimitriou G, McCann UD, Ricaurte GA (1999). Altered serotonin innervation patterns in the forebrain of monkeys treated with (±)3,4-methylenedioxymethamphetamine seven years previously: factors influencing abnormal recovery. J Neurosci 19: 5096–5107.
Heinz A, Jones DW (2000). Serotonin transporters in ecstasy users. Br J Psychiatry 176: 193–195.
Heinz A, Ragan P, Jones DW, Hommer D, Williams W, Knable MB et al (1998). Reduced central serotonin transporters in alcoholism. Am J Psychiatry 155: 1544–1549.
Johnson AM (1991). The comparative pharmacological properties of selective serotonin reuptake inhibitors in animals. In: Heighner JP, Boyer WF (eds). Perspectives in Psychiatry, Vol 1. Selective Serotonin Reuptake Inhibitors. Wilet: Chichester. pp 37–70.
Kish SJ (2002). Effects of MDMA (ecstasy) use and abstention on serotonin neurons. Lancet 359: 1616.
Kish SJ, Furukawa Y, Ang L, Vorce SP, Kalasinsky KS (2000). Striatal serotonin is depleted in brain of a human MDMA (Ecstasy) user. Neurology 55: 294–296.
Kugaya A, Seneca NM, Snyder PJ, Williams SA, Malison RT, Baldwin RM et al (2003). Changes in human in vivo serotonin and dopamine transporter availabilities during chronic antidepressant administration. Neuropsychopharmacology 28: 413–420.
Laruelle M, Baldwin RM, Malison RT, Zea-Ponce Y, Zoghbi SS, al Tikriti MS et al (1993). SPECT imaging of dopamine and serotonin transporters with [123I]β-CIT: pharmacological characterization of brain uptake in nonhuman primates. Synapse 13: 295–309.
Laruelle M, Wallace E, Seibyl JP, Baldwin RM, Zea-Ponce Y, Zoghbi SS et al (1994). Graphical, kinetic, and equilibrium analyses of in vivo [123I]β-CIT binding to dopamine transporters in healthy human subjects. J Cereb Blood Flow Metab 14: 982–994.
Lew R, Sabol KE, Chou C, Vosmer GL, Richards J, Seiden LS (1996). Methylenedioxymethamphetamine-induced serotonin deficits are followed by partial recovery over a 52-week period. Part II: radioligand binding and autoradiography studies. J Pharmacol Exp Ther 276: 855–865.
Lucki I (1998). The spectrum of behaviors influenced by serotonin. Biol Psychiatry 44: 151–162.
Malison RT, Price LH, Berman R, van Dyck CH, Pelton GH, Carpenter L et al (1998). Reduced brain serotonin transporter availability in major depression as measured by [123I]-2β-carbomethoxy-3β-(4-iodophenyl)tropane and single photon emission computed tomography. Biol Psychiatry 44: 1090–1098.
Meyer JH, Wilson AA, Sagrati S, Hussey D, Carella A, Potter WZ et al (2004). Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. Am J Psychiatry 161: 826–835.
Oya S, Choi SR, Hou C, Mu M, Kung MP, Acton PD et al (2000). 2-((2-((dimethylamino)methyl)phenyl)thio)-5-iodophenylamine (ADAM): an improved serotonin transporter ligand. Nucl Med Biol 3: 249–254.
Parrott AC (2000). Human research on MDMA (3,4-methylenedioxymethamphetamine) neurotoxicity: cognitive and behavioural indices of change. Neuropsychobiology 42: 17–24.
Parsey RV, Kegeles LS, Hwang DR, Simpson N, Abi-Dargham A, Mawlawi O et al (2000). In vivo quantification of brain serotonin transporters in humans using [11C]McN 5652. J Nucl Med 41: 1465–1477.
Pirker W, Asenbaum S, Hauk M, Kandlhofer S, Tauscher J, Willeit M et al (2000). Imaging serotonin and dopamine transporters with 123I-β-CIT SPECT: binding kinetics and effects of normal aging. J Nucl Med 41: 36–44.
Pirker W, Asenbaum S, Kasper S, Walter H, Angelberger P, Koch G et al (1995). CIT SPECT demonstrates blockade of 5HT-uptake sites by citalopram in the human brain in vivo. J Neural Transm Gen Sect 100: 247–256.
Reneman L, Booij J, de Bruin K, Reitsma JB, de Wolff FA, Gunning WB et al (2001b). Effects of dose, sex, and long-term abstention from use on toxic effects of MDMA (ecstasy) on brain serotonin neurons. Lancet 358: 1864–1869.
Reneman L, Booij J, Habraken JBA, de Bruin K, Hatzidimitiou G, den Heeten GJ et al (2002). Validity of [123I]β-CIT SPECT in detecting MDMA-induced serotonergic neurotoxicity. Synapse 46: 199–205.
Reneman L, Lavalaye J, Schmand B, de Wolff FA, van den Brink W, den Heeten GJ et al (2001a). Cortical serotonin transporter density and verbal memory in individuals who stopped using 3,4-methylenedioxymethamphetamine (MDMA or ‘ecstasy’): preliminary findings. Arch Gen Psychiatry 58: 901–906.
Ricaurte GA, McCann UD (2001). Assessing long-term effects of MDMA (Ecstasy). Lancet 358: 1831–1832.
Ricaurte GA, Yuan J, McCann UD (2000). 3,4-Methylenedioxymethamphetamine (‘Ecstasy’)-induced serotonin neurotoxicity: studies in animals. Neuropsychobiology 42: 5–10.
Scheffel U, Dannals RF, Cline EJ, Ricaurte GA, Carroll FI, Abraham P et al (1992). [123/125I]RTI-55, an in vivo label for the serotonin transporter. Synapse 11: 134–139.
Scheffel U, Kim S, Cline EJ, Kuhar MJ (1994). Occupancy of the serotonin transporter by fluoxetine, paroxetine, and sertraline: in vivo studies with [125I]RTI-55. Synapse 16: 263–268.
Seibyl JP, Wallace E, Smith EO, Stabin M, Baldwin RM, Zoghbi S et al (1994). Whole-body biodistribution, radiation absorbed dose and brain SPECT imaging with iodine-123-β-CIT in healthy human subjects. J Nucl Med 35: 764–770.
Semple DM, Ebmeier KP, Glabus MF, O'Carroll RE, Johnstone EC (1999). Reduced in vivo binding to the serotonin transporter in the cerebral cortex of MDMA (‘ecstasy’) users. Br J Psychiatry 175: 63–69.
Staley JK, Basile M, Flynn DD, Mash DC (1994). Visualizing dopamine and serotonin transporters in the human brain with the potent cocaine analogue [125I]RTI-55: in vitro binding and autoradiographic characterization. J Neurochem 62: 549–556.
Suhara T, Sudo Y, Yoshida K, Okubo Y, Fukuda H, Obata T et al (1998). Lung as reservoir for antidepressants in pharmacokinetic drug interactions. Lancet 351: 332–335.
Szabo Z, McCann UD, Wilson AA, Scheffel U, Owonikoko T, Mathews WB et al (2002). Comparison of (+)-11C-McN5652 and 11C-DASB as serotonin transporter radioligands under various experimental conditions. J Nucl Med 43: 678–692.
Talairach J, Tournoux P (1988). Co-Planar Stereotaxic Atlas of the Human Brain. Thieme: New York.
Tauscher J, Pirker W, de Zwaan M, Asenbaum S, Brücke T, Kasper S (1999). In vivo visualization of serotonin transporters in the human brain during fluoxetine treatment. Eur Neuropsychopharmacol 9: 177–179.
Thomasius R, Petersen K, Buchert R, Andresen B, Zapletalova P, Wartberg L et al (2003). Mood, cognition and serotonin transporter availability in current and former ecstasy (MDMA) users. Psychopharmacology 167: 85–96.
Verbaten MN (2003). Specific memory deficits in ecstasy users? The results of a meta-analysis. Hum Psychopharmacol 18: 281–290.
Wenk GL (2003). Neuropathologic changes in Alzheimer's disease. J Clin Psychiatry 64 (Suppl 9): 7–10.
Worsley KJ, Evans AC, Marrett S, Neelin P (1992). A three-dimensional statistical analysis for CBF activation studies in human brain. J Cereb Blood Flow Metab 12: 900–918.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Win, M., Habraken, J., Reneman, L. et al. Validation of [123I]β-CIT SPECT to Assess Serotonin Transporters In Vivo in Humans: a Double-Blind, Placebo-Controlled, Crossover Study with the Selective Serotonin Reuptake Inhibitor Citalopram. Neuropsychopharmacol 30, 996–1005 (2005). https://doi.org/10.1038/sj.npp.1300683
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300683
Keywords
This article is cited by
-
A review on pathology, mechanism, and therapy for cerebellum and tremor in Parkinson’s disease
npj Parkinson's Disease (2022)
-
Expectancy effects on serotonin and dopamine transporters during SSRI treatment of social anxiety disorder: a randomized clinical trial
Translational Psychiatry (2021)
-
Simultaneous serotonin and dopamine monitoring across timescales by rapid pulse voltammetry with partial least squares regression
Analytical and Bioanalytical Chemistry (2021)
-
Tobacco smoking and dopaminergic function in humans: a meta-analysis of molecular imaging studies
Psychopharmacology (2019)
-
Lower serotonin transporter binding in patients with cervical dystonia is associated with psychiatric symptoms
EJNMMI Research (2017)