Abstract
Study design: We evaluated the effects of serotonin (5-HT) agonists on in vitro models of spinal cord compressive injury. Evoked potentials in injured rat spinal cords (n=24) were recorded during perfusion with 5-HT agonists.
Objectives: To evaluate the therapeutic effects of 5-HT agonists on the recovery of compound action potentials in injured spinal cords.
Methods: Rat dorsal columns were isolated, placed in a chamber, and injured by extradural compression with a clip. Conducting action potentials were activated by supramaximal constant current electrical stimuli and recorded during perfusion with 5-HT agonists and antagonists.
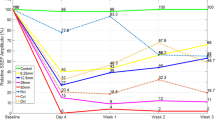
Results: After inducing compression injuries, mean action potential amplitudes were reduced to 33.9±5.4% of the pre-injury level. After 120 min of perfusion with Ringer's solution, the mean amplitudes recovered to 62.8±8.4% of the pre-injury level. At a concentration of 100 μM, perfusion with tandospirone (a 5-HT1A agonist) resulted in a significantly greater recovery of mean action potential amplitudes at 2 h after the injury (86.2±6.9% of pre-injury value) as compared with the control Ringer's solution (62.8±8.4% of pre-injury value, P<0.05). In contrast, quipazine (a 5-HT2A agonist) accelerated the decrease of amplitude (54.5±11.7% of pre-injury value). 5-HT1A and 5-HT2A agonist did not consistently alter latencies of the action potentials.
Conclusion: The 5-HT1A receptor agonist was effective for the recovery of spinal action potential amplitudes in a rat spinal cord injury model.
Similar content being viewed by others
Introduction
During the acute phase of a spinal cord injury, 5-HT may accelerate secondary damage, since it is known to be released at the injury site.1,2,3 We recently showed that both the 5-HT1A and 5-HT2A receptor subtypes are present on spinal dorsal column axons, and that they have opposing effects on axonal excitability. 5-HT2A agonists strongly excite action potentials, whereas 5-HT1A agonists depress them.4,5,6 Further, mianserin (5-HT2A antagonist) has been reported to be neuroprotective in acute spinal cord injuries.7,8 Thus, 5-HT receptors may play a role in the pathological responses of axons to injury. However, in the absence of any previous evidence for 5-HT receptors existing on axons, most hypotheses regarding 5-HT mediated secondary axonal injury have focused on indirect mechanisms, such as posttraumatic ischemia. Our previous results provided a theoretical basis for the direct action of 5-HT mediating excitotoxicity in axons, and suggested a new and interesting therapeutic approach to spinal cord injury. We postulated that 5-HT1A agonists depress axonal excitability and, as a consequence, they may also exert neuroprotective effects. To determine the role of 5-HT1A agonist in acute spinal cord injury, we evaluated methods of 5-HT agonists treatment with in vitro models of dorsal column axon compressive injury.
Materials and methods
A total of 24 male adult Wistar rats weighing 250–350 g were used, after being anesthetized with methoxyflurane and decapitated. Care of the animals was conducted in accordance with the Guide to the Care and Use of Experimental Animals (Shiga University of Medical Science). The dorsal columns were isolated,9,10 placed in a 3 ml recording chamber, and superfused at 120 ml/h with room-temperature (23–27°C) Ringer's solution for 2–3 h to wash out the methoxyflurane and stabilize the responses. The Ringer's solution contained NaCl (124 mM), KCl (3 mM), Na2HPO4 (1 mM), NaHCO3 (26 mM), MgSO4 (1.5 mM), CaCl2 (1.5 mM), and glucose (10 mM). The solution was saturated with O2 (95%) and CO2 (5%) at pH 7.4.
Many 5-HT receptor subtypes have been discovered in central nervous tissues and described.11 5-HT presumably activates all 5-HT receptors, whereas quipazine likely activates primarily 5-HT2A receptors, tandopirone should selectively activate 5-HT1A receptors, and mianserin should block 5-HT2A receptors. Table 1 summarizes the eight drug protocols tested (protocol ABCDEFGH listed in Table 1, n=49). The drugs were mixed into Ringer's solution and superfused at 120 ml/h for the 20 min incubation period. We tested the effects of 5-HT hydrochloride (5-HT HCl, SIGMA, St. Louis, MO, USA, protocol A listed in Table 1, n=8), quipazine dimaleate (quipazine, SIGMA, St. Louis, MO, USA, protocol BC listed in Table 1, n=10), and tandospirone (Sumitomo Pharm. Co. Ltd, Japan, protocol EF listed in Table 1, n=13). The protocols include two superfusate concentrations (10 μM and 100 μM) of quipazine and tandospirone. In the six experiments, we incubated the nerve preparations for 20 min in mianserin HCl (a 5-HT2A receptor antagonist, SIGMA, St. Louis, MO, USA, protocol D listed in Table 1, n=6) before applying the quipazine. In the six experiments, mianserin alone was superfused (protocol G listed in Table 1, n=6). In the six control experiments, Ringer's solution alone was superfused (protocol H listed in Table 1, n=6). Control pre-drug response amplitudes and latencies were 0.785±0.126 mV and 6.71±0.92 ms in experiments using maximal stimuli. The 5-HT agonist solutions included 0.01% ascorbic acid (Sigma, St. Louis, MO, USA) to inhibit oxidation, which had no effect on the action potentials in the preparations.
At superfusion rates of 120 ml/h, we predicted that drug concentrations in the chamber would approach 95% of the concentrations in the incoming fluid within 6 min, 99% within 10 min, and 99.9% by 30 min. We applied the agonists for 20 min. Further, the preparations were incubated for 10 min before and 10 min after injury.
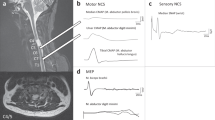
To activate the action potentials, we applied 0.2 Hz constant-current 200 μs duration pulses (Pulse Generator, MacLab Software, Australia) with a bipolar platinum electrode placed on the dorsal column (Stimulator, Nihon Kohden SEM4201, Japan). Maximal response by stimulation was determined by progressively elevating the current intensity until the response no longer showed a greater amplitude with additional current. The action potentials were recorded using glass micropipettes filled with 1 M NaCl that were inserted 50 μm deep into the dorsal column. The mean conduction distance between the stimulus and recording electrodes was 2.3±0.54 mm. The voltage signals were amplified (Amplifier (100×), Nihon Kohden AB601G, Japan), analyzed and displayed graphically on a computer (Data Acquisition, MacLab Software, Macintosh, PowerBook550c), as illustrated in Figure 1. Response amplitudes were measured from the initial positive peak (P1) to the first large negative peak (N1) of each compound action potential. Response latencies were measured from stimulus onset to N1.
The mean action potential amplitudes and latencies are expressed as percentages of the pre-injury control levels, which were obtained before spinal cord compression. All±values indicate standard deviations. To compare the treatment protocols, we applied statistical analysis. Significant differences between the control and treatment groups were determined by analysis of variance (ANOVA). Differences were deemed statistically significant at P<0.05.
Results
The isolated rat dorsal columns were typically 3.0 cm in length. Stimulation with constant-current pulses activated robust compound action potentials that were conducted along the length of the dorsal column preparations. Table 2 summarizes the mean control amplitudes and latencies found in individual groups. Since stimulus and recording positions differed from preparation to preparation, the control response amplitudes and latencies varied. However, the response characteristics remained stable within each experiment, seldom varying more than 5% over periods of 20–30 min.
After compression injury, the mean action potential amplitudes were reduced to 33.9±5.4%, and then recovered to 62.8±8.4% after 120 min of perfusion with Ringer's solution. At 10 μM and 100 μM concentrations, perfusion with tandospirone showed recovery values of 68.3±14.5% and 86.2±6.9% of the pre-injury values, respectively, and the 100 μM concentration of tandospirone resulted in a significantly greater recovery of mean action potential amplitudes as compared with the control Ringer's solution 2 h after injury (P<0.05). The latency shifts with 10 μM and 100 μM concentrations of tandospirone were respectively 2.3±4.8% and 2.2±2.0%. In contrast, 100 μM of quipazine (a 5-HT2A agonist) caused significantly less recovery as compared with the control Ringer's solution from 60 to 100 min after injury (P<0.05). Quipazine did not consistently affect response latencies. At a 50 μM concentration, mianserin (a 5-HT2A antagonist) eliminated the inhibitory effects of 100 μM quipazine, whereas 5-HT did not significantly affect the recovery of response amplitudes. Moreover, at 120 min after injury, neither the 10 μM nor 100 μM concentration of quipazine showed a significant reduction of amplitudes, while a 50 μM concentration of mianserin had no effect on the change of action potentials in the in vitro preparations.
Discussion
More than three decades ago, Osterholm, et al.12 suggested that the neurotransmitter 5-HT causes tissue damage in the brain. It has since been proposed that 5-HT contributes to the posttraumatic decline of blood flow and edema seen in injured spinal cords.13,14,15,16 Microdialysis studies have shown that a spinal cord injury releases large amounts of 5-HT into extracellular spaces,3,17,18 and we also reported that 5-HT is released from neural elements at the injury site and is transiently taken up by platelets.1,2 Mianserin, a 5-HT antagonist, has been reported to have beneficial effects towards the recovery of neurologic and neurophysiologic functions in acute spinal cord injury models.7,8 However, the mechanisms by which 5-HT causes secondary tissue damage, especially with axons, are not well understood. Most investigators have focused on the possible indirect effects of 5-HT, such as posttraumatic ischemia, and it has been demonstrated that some peripheral and central axon terminals have 5-HT autoreceptors.19,20 We recently found that spinal axons possess 5-HT receptors and suggested that 5-HT may have a direct excitotoxic effect on spinal axons.4,5,6
In previous experiments, 5-HT had robust effects on dorsal columns obtained from rats,4,5,6 and both 5-HT1A and 5-HT2A receptor subtypes were found on spinal dorsal column axons, however, they demonstrated opposing effects on axonal excitability. Further, we found that 5-HT2A agonists strongly excite action potentials, while 5-HT1A agonists depress them.4,5,6 It would be of interest to extend this area of study to investigate actual injured spinal cords, as the ratio of 5-HT2A/5-HT1A receptor expression at various stages after injury may well influence axonal responses to the extracellular neurotransmitter derangements that occur during those processes. In the previous study, it has been demonstrated that the neurotransmitters had the effects on dorsal columns obtained from neonatal rats.4 While the sensitivity diminished with maturation of dorsal column. We thought that the damage of the myelin sheath by spinal cord injury might cause the penetration of neurotransmitter. Our previous results also suggested an interesting and new therapeutic approach to spinal cord injury. Since 5-HT1A agonists probably depress axonal excitability more than the 5-HT2A antagonist, as a consequence, 5-HT1A agonists may also exert neuroprotective effects, perhaps more strongly than the 5-HT2A antagonist. Fortunately, many highly selective 5-HT1A receptor agonists are already available as drugs,11 while tandospirone is commonly used to treat anxiety disorders.21 It has been reported that the 5-HT-induced nociceptive response is mediated by 5-HT2A receptors in the periphery.22 Therefore, our study also suggests a therapeutic approach for the pain and numbness.
The data from this present study indicate that tandospirone and quipazine have opposing effects on an injured spinal cord, as the recovery of the compound action potential amplitude with 100 μM tandosporine significantly exceeded that seen in the control group, and quipazine (100 μM) accelerated the amplitude decrease at 60–100 min after injury. Moreover, mianserin (50 μM) blocked the quipazine induced amplitude change. The most conservative explanation of these results is that 5-HT2A receptors increase the excitotoxicity of dorsal column axons while 5-HT1A receptors decrease it following spinal cord injury. In conclusion, the 5-HT1A receptor agonist was effective for the recovery of spinal action potential amplitudes in a rat spinal cord injury model.
References
Saruhashi Y, Hukuda S, Maeda T . Acute aggregation of serotonin-immunoreactive platelets in the injured spinal cord of rat and change of serotonin content in the neural fibers J Neurotrauma 1990 7: 237–246
Saruhashi Y, Hukuda S, Maeda T . Evidence for a neural source of acute accumulation of serotonin in platelets in the injured spinal cord of rats. An experimental study using 5,6-dihydroxytryptamine treatment J Neurotrauma 1991 8: 121–128
Liu DX, Valadez V, Sorkin LS, McAdoo DJ . Norepinephrine and serotonin release upon impact injury to rat spinal cord J Neurotrauma 1990 7: 219–227
Saruhashi Y, Young W . Excitatory and inhibitory effects of serotonin on spinal axons Neurosci 1994 61: 645–653
Saruhashi Y et al. Evidence for serotonin sensitivity of adult rat spinal axons: Studies using randomized double pulse stimulation Neurosci 1997 80: 559–566
Saruhashi Y, Young W, Hassan AZ . Calcium-mediated intracellular messengers modulate the serotonergic effects on axonal excitability Neurosci 1997 81: 959–965
Puniak MA et al. Comparison of a serotonin antagonist, opioid antagonist, and TRH analog for the acute treatment of experimental spinal trauma J Neurotrauma 1991 8: 193–203
Salzman SK et al. The serotonin antagonist mianserin improves functional recovery following experimental spinal trauma Ann Neurol 1991 30: 533–541
Honmou O, Sakatani K, Young W . GABA and potassium effects on corticospinal and primary afferent tracts of neonatal rat spinal cord dorsal columns Neurosci 1993 54: 93–104
Saruhashi Y et al. GABA increases refractoriness of adult rat dorsal column axons Neurosci 1999 94: 1207–1212
Zifa E, Fillion G . 5-hydroxytryptamine receptors Pharm Rev 1992 44: 401–458
Osterholm JL, Bell J, Meyer R . Experimental effects of free serotonin on the brain and its relation to brain injury J Neurosurg 1996 31: 408–421
Abraham J et al. Spinal cord edema, 5-hydroxytryptamine, lipid peroxidation, and lysosomal enzyme release after acute contusion and compression injury in primates Cent Nerv Syst Trauma 1985 2: 45–60
Brodner RA, Dohrman GJ, Roth RH, Rubin RA . Correlation of cerebrospinal fluid serotonin and altered spinal cord blood flow in experimental trauma Surg Neurol 1980 13: 337–343
Cirino G et al. Human recombinant lipocortin 1 has acute local anti-inflammatory properties in the rat paw edema test Proc Natl Acad Sci USA 1989 86: 3428–3432
Sharma HS, Olsson Y, Dey PK . Early accumulation of serotonin in rat spinal cord subjected to traumatic injury. Relation to edema and blood flow changes Neurosci 1990 36: 725–730
Sorkin LS et al. Microdialysis recovery of serotonin released in spinal cord dorsal horn J Neurosci Meth 1988 23: 131–138
Sorkin LS et al. Release and metabolism of 5-hydroxytryptamine in the cat spinal cord examined with microdialysis J Pharmacol Exp Ther 1991 257: 192–199
Heidenreich BA, Rebec GV . Serotonergic dorsal raphe neurons: changes in spontaneous neuronal activity and responsiveness to 5-MeODMT following long-term amphetamine administration Neurosci Lett 1989 103: 81–86
Thor KB, Hisamitsu T, de Groat WC . Unmasking of a neonatal somatovesical reflex in adult cats by the serotonin autoreceptor agonist 5-methoxy-N,N-dimethyltryptamine Dev Brain Res 1990 54: 35–42
Hamik A, Oksenberg D, Fischette C, Peroutka SJ . Analysis of tandospirone (SM-3997) interactions with neurotransmitter receptor binding sites Biol Psychiatry 1990 28: 99–109
Doi-Saika M, Tokunaga A, Senba E . Intradermal 5-HT induces Fos expression in rat dorsal horn neurons not via 5-HT3 but via 5-HT2A receptors Neurosci Res 1997 29: 143–149
Acknowledgements
We thank Dr Wise Young, Dr Toru Imanaka, and Dr Naruhiro Tanaka for their kind help and helpful discussions. This study was supported by a grant from Japan Orthopaedics and Traumatology Foundation, Inc., No. 0095.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Saruhashi, Y., Matsusue, Y. & Hukuda, S. Effects of serotonin 1A agonist on acute spinal cord injury. Spinal Cord 40, 519–523 (2002). https://doi.org/10.1038/sj.sc.3101331
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101331
Keywords
This article is cited by
-
The recovery of 5-HT transporter and 5-HT immunoreactivity in injured rat spinal cord
Archives of Orthopaedic and Trauma Surgery (2009)
-
The antioxidant effect of β-Glucan on oxidative stress status in experimental spinal cord injury in rats
Neurosurgical Review (2005)