Abstract
Study Design:
Case control study.
Objective:
To determine the main risk factors for pressure ulcer (PU) in ambulatory spinal cord injury (SCI) patients.
Setting:
Hospital del Trabajador, Santiago, (ACHS (Chilean Security Association), Chile.
Methods:
We studied 41 patients for traumatic SCI, from Santiago, Chile, cared for in our hospital. The clinical histories were reviewed from first discharge to 1996. The patients were categorized into two groups: 18 cases with a previous history of PU, and 23 patients with no history of PU were considered as controls. Univariate analysis was performed, 18 variables per case, 10 of which were psychosocial factors.
Results:
There were 37 men and four women. Average age was 41.7 years. Duration of SCI on average was 6.7 years. The distribution was complete paraplegia (CPP) 22 patients (54%), complete tetraplegia three patients (7%), incomplete paraplegia 11 patients (27%) and incomplete tetraplegia, five patients (12%). Four variables of the univariate analysis were significant: duration of cord injury (SCI time) >5 years, completeness of cord injury, paraplegia and not able to practice regular standing. There was a significant association in body morphology (endo or ectomorphic), being able to practice regular standing and personality disorder in CPP.
Conclusions:
The risk for developing PU was 4.3 times greater in CPP patients than is any other type of SCI. CPP patients who do not practice standing periodically, who have a personality disorder and have an ecto/endomorphic corporal morphology have a greater risk of suffering PU.
Similar content being viewed by others
Introduction
A pressure ulcer (PU) is a localized area of cellular necrosis and vascular destruction owing to a prolonged exposure to pressure, shearing or friction.1, 2, 3, 4, 5 The lack of sensibility and movement owing to the SCI favor the development of these lesions.5
PUs are frequent in SCI patients, with a prevalence of 25 to 30% a year.2, 6, 7, 8 Most PUs in ambulatory SCI patients occur in the ischiatic region,6, 9, 10 and can sometimes lead to additional complications such as amputation of extremities and urinary or bowel diversions.6, 11 PUs have a significant negative effect on the general health and quality of life of these patients.
None of the traditional risk assessment scoring systems have been useful in predicting the occurrence of PU in SCI patients. 4 Major risk factors are decreased activity,12 immobility,13, 14 how complete the cord injury is,1, 3, 4, 7, 9, 15, 16, 17, 18 urinary incontinence/being wet, altered autonomic reflexes and severe spasticity. PUs occur most frequently in complete SCI. The literature does not show agreement on the importance of the level of injury as a risk indicator.6, 8, 16 Pre-existing conditions such as being elderly,1, 2, 3, 9, 16 smoking,1, 4, 18 cardiopulmonary and renal diseases,4, 19 diabetes mellitus,4 reduced cognitive function, living in retirement/nursing homes, malnutrition and anemia, hypoalbuminemia (<3.4 g/dl) and hemoglobin <12 g/dl are also major risk factors.2, 3, 4, 7, 20
Potential risk factors for the development of PU are noncompliance with prevention measures, being in a noncollaborating environment, emotional stress, being single, poor responsibility for skin hygiene, low satisfaction with the activities of daily living (ADL), poor self esteem3, 4, 6, 7, 21 and personality disorders.22, 23, 24 Lack of education, of a job, no group activities, no sexual activity and others are also associated to PU occurrence in SCI patients.6, 7, 25
Heilporn24 described a mental disorder in these patients, which he called Ectodermic Syndrome, characterized by repeated PUs, inability to understand the importance of skin care, rejection of the condition of being disabled and being refractory to mental treatment.
The purpose of this study was to determine the main risk factors for PU and to construct a predictive model of PU in SCI patients in their ambulatory stage.
Methods
All patients had traumatic SCI. They were residents of the Metropolitan Region and were cared for at the Hospital del Trabajador in Santiago, Chile. The patients were affiliated to the Asociación Chilena de Seguridad (Chilean Safety Association); a private, nonprofit Insurance Company that administers the law that governs work-related injuries and occupational diseases.
Patient selection was sequential, and included all patients who lived in the Metropolitan Region during the study period and were affiliated to the Chilean Security Association. The clinical history of each patient was analyzed, from after first hospitalization to 1996 (about 7 years follow-up). History taking, physical examination, psychological and social studies were carried out. Laboratory work-up included blood hemoglobin, WBC count and differential, albuminemia, blood sugar and serum Transferrin. Two groups of patients were considered; 18 patients with a history of previous ambulatory PU (cases) and 23 patients without a history of ambulatory PU (controls).
Eighteen variables were analyzed for each case: age, completeness of SCI, SCI time, body type (ecto or endomorphic), fecal and/or urinary incontinence, smoking, spasticity, able or not able to practice regular standing, having a life partner, having a job, social interaction problems, sexuality, anxiety, depression, personality disorders, poor family relationship, alcoholism and moderate or severe psycho-organic deterioration associated to a concurrent traumatic brain injury.
Definition of variables
Age, age at the time of the study.
Completeness of SCI, according to the ASIA/ISCoS scales of international standards.
SCI time, time in years from the accident to the moment of the study.
Body type (ecto or endomorphic), ectodermic were thin patients, with easily palpable bony prominence and body mass index <20 kg/cm2. Endomorphic were obese patients with abundant subcutaneous tissues, especially in the abdominal and pelvic areas and a body mass index >30 kg/cm2.
Fecal and/or urinary incontinence, impossibility of controlling defecation or micturition, requiring permanent use of diapers.
Smoking, habit of periodically smoking five or more cigarettes per day for 1 year or more (this dose of nicotine is enough to produce cutaneous ischemia).
Spasticity, motor disorder characterized by velocity-dependent increased muscle tonus and increased tendinous reflexes.26
Able or not able to practice regular standing, or bipedestation, to be able to stand with or without orthosis for one hour or more, two or more times a week.
Having a life partner, the patient having a person (same or different sex) with whom he/she has positive affection manifestations, care and love, and this is emotionally significant
Having a job, having work, socially recognized as such, whether it is paid or not.
Social interaction problems, having significant problems in participating in formal or informal social groups such as clubs, church, friends or extended family.
Sexuality, having satisfactory sexual and intimacy relationships in quality and frequency.
Anxiety, a tension reaction of constant worry, with no apparent cause, diffuse, that appears when is danger or threat (that may even be subjective) and is manifested by a series of physiological, cognitive and behavioral responses. It can be acute (crisis) or chronic (generalized anxiety disorder).
Depression, generalized mood disorder characterized by sadness and the loss of the ability to experience pleasure (anhedonia). There may also be thought distortion, suicidal ideas, somatic and vital rhythm disturbances.
Personality disorder, an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual's culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time and leads to distress or impairment (DSM IV).
Poor family relationship, poor family relationship with presence of physical and or psychological intrafamilial violence.
Alcoholism, physical and psychological abuse and dependence on alcohol.
Moderate or severe psycho-organic deterioration associated to a concurrent traumatic brain injury, signs of organic brain damage related to brain concussion/trauma evidenced psychometric assessment as moderate or severe and that significantly interferes with the patient activities of daily living (ADL).
The National Pressure Ulcer Advisory Panel (NPUAP) classification system27 was used: types I and II were considered superficial ulcers and types III and IV were considered deep ulcers.
All applicable institutional and governmental regulations concerning ethics in the study of human volunteers were followed during the course of this research.
Results
In total, 37 men and four women were studied. Age at the time of assessment was 41.7±12.0 years (19.5–71.4 years), SCI time 6.7±4.4 years (0.1–20.7 years). Types of SCI are Complete paraplegia 22 patients (54%), complete tetraplegia three patients (7%), incomplete paraplegia 11 patients (27%), and incomplete tetraplegia five patients (12%).
From 1990 to 1995, 43.9% of this population suffered PU. There was a total of 146 ulcers during the ambulatory stage distributed as follows: 112 pelvic (53 ischiatic, 30 sacral and 29 trocantereal) and 34 in the lower extremities (25 ankle, nine foot). Depth of PU is superficial 54/146 (37%), deep 92/146 (63%). These lesions occur in the ambulatory stage (77%). Of the patients, 18/41 (43.9%) had one or more PU, on average: 3.3 lesions per patient (0–37).
Univariate analysis
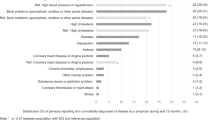
The results of the correlation of each variable with the response are shown in Table 1.
As shown in Table 1, there are five variables with P-values lower than 0.20: SCI time >5 years, complete SCI, paraplegia, able or not able to practice regular standing, social interaction problems and personality disorders.
Complete paraplegia
According to the univariate outcomes and the logistic regression model, the most frequent variable associated with the occurrence of PU is the type of SCI (complete paraplegics and other SCI). Out of 22, 14 (63.6%) patients with CPP had PUs. In patients with other types of SCI (incomplete paraplegics and complete or incomplete tetraplegics), only four out of 19 (21.1%) had PUs (odds ratio (OR)=6.56, IC 95% 1.7–25.6).
SCI time is also associated with PU, so this parameter was also assessed. Median injury time for CPP is 7.3 years, whereas, for other SCI it is 5.5 years (Table 2). The difference is not statistically significant (P=0.43). This shows that the greater percentage of complete paraplegic patients with PUs is not caused by SCI time, and this is confirmed by evaluating the association between presence of PU and complete paraplegia adjusted for SCI time (adjusted OR=9.14, IC 95% 1.8–45.7).
Analysis of the occurrence of the first PU
A regression analysis for survival studies (Cox's regression model), in this case, occurrence of first PU, for CPP and the other SCIs was carried out. By adjusting the model with the variable ‘months’ (difference between date of SCI and date of first PU) we obtain an OR for risk=4.3 (CI 95%: 1.4–13.1 for risk of PU). This indicates a greater risk for CPPs to suffer PU than other SCIs. Figure 1 shows the incomplete tetraplegics and paraplegics. It indicates that there are fewer patients with PU in this group and these PUs occur later in the course of the illness. So, for example, after 2 years of having the cord injury, 18% of patients will have their first PU. Figure 2 shows that in complete paraplegics, the number of Pus is quite high and the majority occur early. After 1 year of suffering from cord injury, approximately 38% of the patients will have their first PU, after 2 years 48% of the patients will have their first PU and after 3 years, 58% of the patients will have their first PU.
Recurrence (occurrence of second PU)
Of 14 CPP, 13 (92.9%) had at least 1 s episode of PU, nine out of 13 (69%) CPP had a second episode of PU before 1 year after the first PU. The average time between first and second PU was 10 months, standard deviation 10 months. Minimum time was 1 month and maximal time 30 months.
A comparison of the physical and psychosocial variables between CPP and other SCI patients is seen in Table 3.
Table 4 assesses the relationship between physical and psychosocial variables with the presence of PU in the complete paraplegic group.
In the CPP group, there is a significant association between the presence of PU and the following: body morphology (endo/ectomorphic), able to practice regular standing or not and personality disorder.
In laboratory results, no differences were detected between both types of patients.
Conclusions
The educational level of the studied Chilean population was low, 6 years of schooling on average. The majority of the patients were nonqualified hand laborers in mining, forestry or construction. The socio-economical level was low ranging in poverty or extreme poverty levels. Currently 20% of the Chilean population is poor, about 6% are in extreme poverty. The average level of disability pensions produced by SCI is US$ 150 monthly. The average family group is made up of four persons (two adults and two children) and frequently this group lives from the patient's pension. Approximately, 50% of the patients work independently gaining additional US$ 100 a month, on average. Given this economic situation, it is frequent to see patients living with kind families that take them in or sometimes take in other families that help with the expenses. Overcrowding in the homes is frequent. Access to health is limited for this population; most are beneficiaries of the Public Health System that has limited resolution power and poor basic health control.
Regarding diseases directly related to SCI such as PU, UTI, these can be cared for with the insurance payed for by their employers at the Asociación Chilena de Seguridad. It is possible to develop prevention programs for this population, thanks to this payment by the employers. Before carrying out this study, the magnitude of the PU problem in SCI patients was not known.
The variables that predict occurrence of PU in our SCI patients in the ambulatory phase are complete paraplegia (CPP) and SCI time >5 years (SCIT5). Having CPP is associated to a greater risk of suffering PU. These data are an advance regarding contradictory reports in the literature.4, 6, 8, 16
The risk for CPP to have PU is 4.3 times greater than other types of SCI. CPPs also have their first PU earlier than patients with other types of SCI. The probability of having a second PU is 92.9% for complete paraplegics.
Some CPP patients have a greater risk of suffering PU than others. They can be grouped into three risk groups: CPPs with personality disorder, those who do not practice standing periodically and those having an ecto/endomorphic corporal type. The most important of these for treatment is the personality disorder as it can condition the other two factors, lack of practicing regular standing and feeding disorders, which lead to body-type disorders. We recommend patients to be subgrouped accordingly; complete paraplegic patients with personality disorder, complete paraplegic patients without personality disorder and patients with other types of SCI.
The importance of the results of this study is that SCI patients with a high risk of developing PU can be identified and preventive interventions can be implemented to avoid this complication, as periodical home control by a registered nurse thereby stimulating PU prevention at home as well as allowing early detection and treatment of the PU, improving the quality of life for the patient and reducing the costs of care.11
References
Yarkony GM . Pressure ulcers: a review. Arch. Phys Med Rehabil 1994; 75: 908–917.
Kosiak M, Kottke FJ . Prevention and rehabilitation of ischemic ulcers. In: Kottke FJ, Lehmann JF (eds). Krusen's Handbook of Physical Medicine and Rehabilitation 4th edn. WB Saunders: Philadelphia 1990, pp 976–987.
Donovan WH et al. Pressure ulcers. In: DeLisa JA, Gans BM (eds). Rehabilitation Medicine 2nd edn. Principles and Practice. Lippincott JB: Philadelphia 1993, pp 716–732.
Byrme DW, Salzberg CA . Major risk factors for pressure ulcers in the spinal cord disabled:a literature review. Spinal Cord 1996; 34: 255–263.
Rochon PA et al. Risk assessment for pressure ulcers: an adaptation of the National Pressure Ulcer Advisory Panel risk factors to spinal cord injured patients. J Am Paraplegia Soc 1993; 16: 169–177.
Krause JS . Skin sores after spinal cord injury: relationship to life adjustment. Spinal Cord 1998; 36: 51–56.
Fuhrer MJ et al. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil 1993; 74: 1172–1177.
Rodriguez GP, Garber SL . Prospective study of pressure ulcer risk in spinal cord injury patients. Paraplegia 1994; 32: 150–158.
Vidal J, Sarrias M . An Analysis of the diverse factors concerned with the development of pressure sores in spinal cord injured patients. Paraplegia 1991; 29: 261–267.
Lehman CA . Risk factors for pressure ulcers in the spinal cord injured in the community. SCI Nurs 1995; 12: 110–114.
Garber SL, Rintala DH, Hart KA, Fuhrer MJ . Pressure ulcer risk in spinal cord injury: predictors of ulcers status over 3 years. Arch Phys Med Rehabil 2000; 81: 465–471.
Krause JS, Broderick L . Patterns of recurrent pressure ulcers after spinal cord injury: identification of risk and protective factors 5 or more years after onset. Arch Phys Med Rehabil 2004; 85: 1257–1264.
Salzberg CA et al. A new pressure ulcer risk assessment scale for individuals with spinal cord injury. Am J Phys Med Rehabil 1996; 75: 96–104.
Niazi ZB, Salzberg CA, Byrne DW, Viehbeck M . Recurrence of initial pressure ulcer in persons with spinal cord injuries. Adv Wound Care 1997; 10: 38–42.
Lee BY . Plastic surgery for pressure sores. In: Lee BY, Ostrander LE (eds). Comprehensive Management of the Spinal Cord Injured Patient. WB Saunders: San Diego 1991, pp 223–230.
Thiyaragajan C, Silver JR . Aetiology of pressure sores in patients with spinal cord injury. Brit Med J Clin Res 1984; 289: 1487–1490.
Abruzzese RS . Pressure sores: nursing aspects and prevention. In: Lee BY, Ostrander LE (eds). Comprehensive Management of the Spinal Cord Injured Patient. WB Saunders: San Diego 1991, pp 210–222.
Lamid S, El Ghatit AZ . Smoking, spasticity and pressure sores in spinal cord injured patients. Am J Phys Med Rehabil 1983; 62: 300–306.
Salzberg CA et al. Pg and preventing pressure ulcers in adults with paralisis. Adv Wound Care 1998; 11: 237–246.
Shea JD . Pressure sores, classification and management. Clin Orthop Rel Res 1975; 112: 89–100.
Anderson TP, Andberg MM . Psychosocial factors associated with pressure sores. Arch Phys Med Rehabil 1979; 60: 341–346.
Harding-Okimoto MB . Pressure ulcers, self-concept and body image in spinal cord injury patients. SCI Nurs 1997; 14: 111–117.
Richards JS, Meredith R, Fine PR, Nepomucino CS . Psycho-social predictors of decubitus ulcer in spinal cord injury. Arch Phys Med Rehabil 1981; 62: 532.
Heilporn A . Psychological factors in the Causation of pressure sores: case reports. Paraplegia 1991; 29: 137–139.
Krause JS et al. A exploratory study of pressure ulcers after spinal cord injury: relationship to protective behavioral and risk factors. Arch Phys Med Rehabil 2001; 82: 107–113.
Lance JW . Symposium synopsis. In: Feldman RG, Young RR, Koella WP (eds). Spasticity: Disordered Motor Control. Yearbook Medical: Chicago 1980, pp 485–494.
National Pressure Ulcer Advisory Panel:. Pressure ulcers: incidence, economics, risk assessment. Decubitus 1989; 2: 24–28.
Acknowledgements
We specially thank Mrs Valeria Rojas, our secretary, for her valuable help in this research. This research has been supported by the Fundación Científica y Tecnológica de la Asociación Chilena de Seguridad, NOPRO 02/97.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Correa, G., Fuentes, M., Gonzalez, X. et al. Predictive factors for pressure ulcers in the ambulatory stage of spinal cord injury patients. Spinal Cord 44, 734–739 (2006). https://doi.org/10.1038/sj.sc.3101914
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101914
Keywords
This article is cited by
-
The global burden of pressure ulcers among patients with spinal cord injury: a systematic review and meta-analysis
BMC Musculoskeletal Disorders (2020)
-
Predictors of pressure ulcer incidence following traumatic spinal cord injury: a secondary analysis of a prospective longitudinal study
Spinal Cord (2018)
-
Investigating the status of using lower extremity orthoses recommended to patients with spinal cord injury
Spinal Cord (2016)
-
The association between metabolic syndrome and pressure ulcers among individuals living with spinal cord injury
Spinal Cord (2016)
-
Engagement in occupational activities and pressure ulcer development in rehabilitated South Indian persons with spinal cord injury
Spinal Cord (2013)