Abstract
The non-enzymatic reaction between glucose and protein can be chemically reversed by transglycation. Here we report the transglycation activity of hydralazine using a newly developed MALDI-TOF-MS based assay. Hydralazine mediated transglycation of HbA1c, plasma proteins and kidney proteins was demonstrated in streptozotocin (STZ) induced diabetic mice, as evidenced by decrease in protein glycation, as well as presence of hydralazine-glucose conjugate in urine of diabetic mice treated with hydralazine. Hydralazine down regulated the expression of Receptor for Advanced Glycation End products (RAGE), NADPH oxidase (NOX) and super oxide dismutase (SOD). These findings will provide a new dimension for developing intervention strategies for the treatment of glycation associated diseases such as diabetes complications, atherosclerosis and aging.
Similar content being viewed by others
Introduction
Glycation is a proteome wide phenomenon resulting from a series of chemical reactions between proteins and reducing sugars leading to formation of heterogeneous Advanced Glycation End products (AGEs). The level of AGEs increases profoundly in diabetes due to chronic hyperglycemic condition. AGEs interact with Receptor for AGEs (RAGE) leading to oxidative stress and activation of pro-inflammatory pathways, which is believed to be the major cause of glycation associated diseases such as diabetic complications, aging, obesity, inflammation, polycystic ovarian syndrome, ischemic cardiovascular disease, neurodegenerative disorders and cancer1,2. Reducing AGE levels has been considered as an intervention strategy for the treatment of glycation associated diseases3,4. Some of the molecules that reduce AGE levels include aminoguanidine5, OPB-91956, ALT-9467, however, these molecules have not been approved by FDA due to toxic side effects. On the other hand several FDA approved drugs like metformin8, aspirin9, diclofenac10 show antiglycation activity. All these drugs mainly inhibit the AGE formation; however efforts towards reversing AGE formation are minimal. Interestingly cells have evolved an enzymatic reaction known as deglycation mediated by fructosamine-3-kinase (FN3K)11,12 through which AGE formation can be reversed. Deglycation can be achieved chemically by transglycation, where in sugar moiety of Schiff's base/Amadori product is transferred to nucleophiles like free amino acids, polyamines12. Glutathione mediated transglycation has been demonstrated in-vivo12. Therefore, deglycation and transglycation are important protective mechanisms against glycation. Development of transglycating agents for preventing or reversing glycation has been hindered due to lack of high throughput assays. Currently available assays for identification of transglycating compounds are based on NMR analysis, which limits a high throughput screening12. In this study we have developed mass spectrometry based transglycation assay, using this assay transglycation activity of hydralazine was discovered. Furthermore, hydralazine mediated transglycation was demonstrated in streptozotocin (STZ) induced diabetic mice as evidenced by decreased HbA1c, plasma protein glycation and formation of hydralazine glucose conjugates in urine. Consequently decreased expression of Receptor for Advanced Glycation End products (RAGE), NADPH oxidase (NOX) and Super oxide dismutase (SOD) was observed with hydralazine treatment. These findings suggested transglycation can be used as an intervention strategy for the treatment of glycation associated diseases such as diabetic complications, atherosclerosis and aging.
Results
In our previous study we have developed a MALDI-TOF-MS based insulin glycation inhibition assay13, where in insulin (m/z 5808) was glycated with glucose and the intensity of glycated insulin (m/z 5970) was monitored in presence or absence of drugs. This assay was modified to study transglycation by monitoring release of free insulin (m/z 5808) using glycated insulin (m/z 5970) and nucleophilic drugs as reactants. Using this assay, hydralazine, an anti-hypertensive and vasodilating drug, was identified as a transglycating agent (Fig. 1a). The transglycation of insulin was also evidenced by formation of hydralazine glucose conjugate (m/z 323. 13) in a MALDI-TOF-MS analysis (Fig. 1 b). Further, the effect of hydralazine on protein glycation was studied both in vitro, as well as in vivo using STZ induced diabetic mice model system.
In vitro transglycation activity of hydralazine (A) Glycated insulin (m/z 5970) was incubated with either 0 mM, 25 mM or 50 mM hydralazine for three hours at 37°C and formation of unglycated insulin (m/z 5808) was monitored by MALDI-TOF-MS. Hydralazine showed concentration dependent transglycation of glycated Insulin. (B) MALDI-TOF-MS analysis of hydralazine-glucose conjugate formed during transglycation assay where m/z 161.08 and m/z 323.13Da are hydralazine and hydralazine-glucose conjugate respectively.
Glycation leads to protein crosslinking4 and formation of fluorescent AGEs14. Hydralazine inhibited glycation induced in vitro HSA protein cross-linking as analyzed by SDS-PAGE analysis (Fig. 2a). In addition, the drug decreased AGE fluorescence emission at 440 nm suggesting that it inhibits AGE formation (Supplementary Fig. 1). Hydralazine inhibited the AGE formation in a concentration dependent manner and its inhibition was more pronounced compared to aminoguanidine at the same concentration (Fig. 2b). Hydralazine mediated inhibition of in vitro HSA glycation was also studied by LC-MSE analysis, a data independent acquisition wherein all the eluted peptides are fragmented15. This method allowed label free analysis and quantification of even the low intense AGE modified peptides. Previously LC-MSE has been used to characterize post translational modification namely for demiadation16, phosphorylation17 and glycation18,19. Glycated HSA showed more number of AGE modified peptides than unglycated HSA. The number of AGE modified peptides decreased in presence of hydralazine and aminoguanidine. Hydralazine was more potent than aminoguanidine in inhibition of AGEs as observed by decreased number of AGE modified peptides in LC- MSE analysis (Fig. 2c). The representative MS/MS annotated spectra have been shown in supplementary Fig. 2. Furthermore, the extent of decrease in AGE modification by hydralazine was studied. In a recent study, the extent of glycation of eight glucose sensitive peptides of human serum albumin was monitored for early diagnosis of Type 2 diabetes20 (supplementary Table 1). In this study, a similar approach was used albeit with a slight modification, which is described in Material and Methods. As expected the cumulative intensity ratio (CIR) of AGE modified peptides containing Glucose Sensitive Amino acid Residues (GSARs) was highest in glycated HSA than non-glycated HSA. In presence of hydralazine and aminoguanidine, the CIR of GSAR peptides decreased and this decrease was more in hydralazine treatment (Fig. 2d).
In vitro antiglycation activity of hydralazine.
HSA was glycated in vitro in presence or absence of 25 mM and 50 mM of hydralazine or aminoguanidine at 37°C for 7 or 30 days. (A)SDS-PAGE analysis depicting inhibition of glycation induced HSA crosslinking by hydralazine. (B)Hydralazine and aminoguanidine showed glycation inhibition in a concentration dependent manner as observed by decrease in AGE fluorescence emission at 440 nm. The per cent glycation inhibition was calculated by using the formula (C–T)/C × 100, where C and T are fluorescence emission of glycated HSA without or with inhibitor respectively. The bar graph represents the mean values with standard deviation (n = 3). (C) LC-MSE analysis depicting the number of AGE modified peptides in HSA, glycated HSA, glycated HSA in presence of hydralazine (50 mM) and aminoguanidine (50 mM). The values in the bar graph represent the number of AGE modified peptides in at least two replications. Glycated HSA had more number of AGE modified peptides than unglycated HSA. In presence of Hydralazine and aminoguanidine the number of AGE modified peptides were decreased. (D) Heatmap analysis of AGE modified GSAR containing peptides. The extent of AGE modification of GSAR containing peptides of glycated HSA was maximum. Hydralazine and aminoguanidine treatment decreased the AGE modification of GSAR containing peptides. The values in the Heatmap represent the average cumulative intensity ratio (CIR) of AGE modified peptides containing Glucose Sensitive Amino acid Residues (GSARs) to their unmodified form (n = 2). Heat map was generated using Matrix2png online software.
Furthermore, transglycation by hydralazine was demonstrated in vivo in STZ induced diabetic mice. Glycation associated parameters such as glycated hemoglobin (HbA1c), fructosamine, plasma AGEs were monitored. STZ induced diabetes led to increase in HbA1c (8.1%), which was decreased significantly in mice treated with hydralazine (Fig. 3a). The HbA1c decreased with time and was reversed to near normal levels (4.4%) within 15 days of hydralazine treatment (300 mg/L). However, treatment of aminoguanidine for 15 days, even at a higher concentration (2.4 g/L) failed to decrease HbA1c (8.4%) (Fig. 3a). A similar trend was also observed in plasma fructosamine levels (Fig. 3b). These results suggested that the immediate decrease in glycation can be achieved by transglycation rather than glycation inhibition. Hydralazine also decreased AGE modification of plasma proteins. Serum albumin and few abundant plasma proteins showed enhanced AGE modification in diabetic condition, which were transglycated by hydralazine treatment as reflected by decreased AGE modification in western blotting (Fig. 4a). The decrease in AGE modification was similar to a relatively higher concentration of aminoguanidine treatment (Fig. 4a). This trend was also evident in plasma AGE levels quantified by ELISA (Fig. 4b). Further, LC-MSE analysis of serum albumin and few abundant plasma proteins revealed relatively lesser number of AGE modified peptides in hydralazine treatment than aminoguanidine treated and diabetic mice (Fig. 4c and Supplementary Fig. 3).
In vivo transglycation activity of hydralazine.
Male BALB/c mice were injected with 50 mg/kg body weight of STZ for five consecutive days to induce diabetes. The induction of diabetes was confirmed after 30 days by measuring the blood glucose levels and HbA1c. Animals having blood glucose level of above 6.12 ± 1.7 mmol/L with ≥7.0 HbA1C were treated with either hydralazine (300 mg/L) or aminoguanidine (2.4 g/L). (A) Bar graph depicting the HbA1c of control mice, diabetic mice and diabetic mice treated with hydralazine or aminoguanidine at 30th, 45th, 60th and 90th day of experiment. Hydralazine decreased the HbA1c by 45th day (15 days of drug treatment) and was almost equal to that of control mice. The values represent mean ± SE, n = 6, P- value < 0.05. (B) Bar graph depicting the plasma fructosamine levels of control mice, diabetic mice and diabetic mice treated with hydralazine or aminoguanidine at 90th day of experiment. Fructosamine level was measured by using the NBT assay. The reduction of NBT to formazon was measured at 540 nm and levels were calculated using the standard fructosamine. Fructosamine levels were decreased with hydralazine treatment (The values represent mean ± SE, n = 6, P- value < 0.05).
Hydralazine mediated in vivo reduction of AGE modification of plasma proteins.
(A) 5 μg of plasma proteins were separated on 10% SDS-PAGE and transferred onto the PVDF membrane. Plasma proteins were probed for AGE modification by western blot analysis using antibodies against CML (top panel), AGE (middle panel) and pentosidine (bottom panel) antibodies. Hydralazine decreased the AGE modification as measured by densitometric analysis, which is shown in the bar graph. (B) Plasma AGE levels were measured by ELISA. Each well of a 96-well microtiter plate coated with 0.1 ml of 20 μg/ml of plasma was blocked with 0.5% gelatin. Subsequent reactions were performed with 0.1 ml of anti-AGE antibody (0.5 pg/ml), secondary antibody conjugated to alkaline phosphatase and PNPP (p-nitro phenyl phosphate) substrate respectively. The absorbance of each well was recorded at 415 nm with a microplate absorbance reader. Mean of A415 were used to calculate the relative AGE levels in the plasma. The bar graph depicts decrease in relative AGE levels upon treatment with hydralazine and aminoguanidine. (The values represent mean ± SE, n = 6, P- value < 0.05). (C) Bar graph depicts the decrease in number of AGE modified peptides of serum albumin by LC-MSE analysis in presence of hydralazine (HYD) and aminoguanidine (AMG) (n = 2) (D)) Heatmap analysis of extent of AGE modification of GSAR containing peptides of mouse serum albumin. The extent of AGE modification of GSAR containing peptides of glycated mouse serum albumin was maximum. Hydralazine and aminoguanidine treatment decreased the AGE modification of GSAR containing peptides. The values in the Heatmap represent the average cumulative intensity ratio (CIR) of AGE modified peptides containing Glucose Sensitive Amino acid Residues (GSARs) to their unmodified form (n = 2). Heat map was generated using Matrix2png online software.
The extent of in vivo AGE modification was studied as described above (Fig. 2d). However, in case of mouse, the GSARs were identified by homology based sequence alignment with human serum albumin (Supplementary Table 1c). Heatmap analysis of AGE modified GSAR containing peptides of serum albumin suggested that the extent of modification was highest in diabetes and was decreased with hydralazine treatment (Fig. 4d).
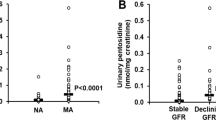
Accumulation of AGEs in the kidney is associated with development of nephropathic condition21. Hydralazine and aminoguanidine decreased AGE levels and AGE modification of kidney proteins in diabetic mice as measured by ELISA and western blot respectively (Fig. 5a and 5b). AGEs are also known to induce increased expression of RAGE, NADPH oxidase and SOD22. Hydralazine and aminoguanidine treated diabetic mice kidney showed decreased expression of these proteins (Fig. 5c).
Effect of hydralazine mediated transglycation on kidney proteins.
(A) Kidney AGE levels were measured by ELISA. Each well of a 96-well microtiter plate coated with 0.1 ml of 20 μg/ml of kidney proteins, was blocked, subsequent reactions were performed with 0.1 ml of anti-AGE antibody (0.5 pg/ml), secondary antibody conjugated to alkaline phosphatase and PNPP (p-nitro phenyl phosphate) substrate respectively. The absorbance of each well was recorded at 415 nm with a microplate absorbance reader. Mean of A415 were used to calculate the relative AGE levels in the kidney. The bar graph depicts decrease in relative AGE levels upon treatment with hydralazine and aminoguanidine. (The values represent mean ± SE, n = 6, P- value < 0.05). (B) 50 μg of kidney proteins were separated on 12% SDS-PAGE and transferred onto the PVDF membrane. AGE modification was probed using AGE antibodies by western blot analysis. Hydralazine decrease the AGE modification of kidney proteins (Lane DIAB-HYD) compared to STZ induced diabetic kidney proteins (Lane DIAB). (C) Western blot analysis of 20 μg of kidney proteins indicating the expression of RAGE, NOX and SOD. Hydralazine and aminoguanidine treatment decreased the expression of these proteins (Lanes DIAB-HYD and DIAB-AMG) as shown by densitometric analysis in the bar graph.
Hydralazine mediated transglycation was also evidenced by analysis of hydralazine glucose conjugate in urine using high resolution accurate mass spectrometer. To analyze the hydralazine glucose conjugate, retention time (RT 6.3 min) was determined by spiking its labeled form (hydralazine 13C-glucose conjugate) as an internal standard (Supplementary Fig. 4). The fragmentation pattern of unlabeled and labeled hydralazine glucose conjugate has been shown in Supplementary Fig. 5. The fragmentation was exactly identical except for few fragments that showed an increase in mass by 1Da e.g. m/z 306.1278 and m/z 198.0853 due to presence of 13C label in those fragments (supplementary Fig. 6, 7). A similar fragmentation pattern was observed in urine sample spiked with labeled conjugate (Fig. 6a). Extracted ion chromatogram (XIC) of selected fragment ion (m/z 305.1244) was used to develop standard curve (Supplementary Fig. 8). Hydralazine glucose conjugate was identified and quantified by monitoring the XIC of its selected fragment ion (m/z 305.1244). About 304.22 ± 20.35 pg of hydralazine glucose conjugate per milliliter of urine was detected in diabetic mice treated with hydralazine (Fig. 6b). This drug conjugate was not detected in control mice treated with hydralazine perhaps due to its lower concentration. Hydralazine treatment showed beneficial effects in terms of decreased levels of plasma cholesterol, triglycerides, blood urea nitrogen and creatinine levels, as compared to diabetic mice and aminoguanidine treated diabetic mice (Table 1).
Detection of hydralazine-glucose conjugate in urine of diabetic mice treated with hydralazine (A) MS/MS fragmentation of hydralazine glucose conjugate in the urine of hydralazine treated diabetic mice, which was spiked with its labeled form. (B) Extracted ion chromatogram (XIC) of selected fragment ion (m/z 305.1244) of hydralazine-glucose conjugate (m/z 323.1335, RT 6.3 min) of synthetic standard, as well as in urine of control and diabetic treated with hydralazine.
Discussion
In this study we have shown that hydralazine inhibits AGE formation by transglycation. The possible mechanism by which hydralazine causes transglycation is depicted in Fig. 7. The reaction between glucose and protein leading formation of Schiff's base and Amadori product is reversible in nature. It is possible that hydralazine interferes at the level of Schiff's base or Amadori product formation and removes the protein bound glucose by virtue of its nucleophillic nature. A similar mechanism was proposed in case of glutathione mediated transglycation12.
Previous studies have employed various strategies to inhibit AGE accumulation23. These approaches are broadly divided into chemical and cellular approaches. Chemical approaches involve inhibition of Amadori products24 and AGEs25, chemical quenching of reactive dicarbonyls26, cross-link breakers27. While, cellular approaches include enzymes such as, aldose reductase28, which converts reducing sugars to corresponding sugar alcohols; aldehyde dehydrogenases and glyoxalases29, which convert reactive dicarbonyls to their inactive forms; matrix metalloproteases that are involved in the release of soluble RAGE (sRAGE) from mRAGE, which prevents AGE interaction with mRAGE30. Another such enzyme, namely fructosamine-3-kinase is involved in deglycation11, which inspired the discovery of small molecule mediated chemical deglycation called transglycation12. Biomolecules such as glutathione, cysteine and polyamines have shown to have tranglycation activity12. Synthetic molecules such as isoniazid and aminoguanidine show poor transglycation activity31. Peptide derivative like N-acetyl carnosine with transglycation activity is being used in the eye drop formulation for the treatment of diabetes induced cataract32, although this is an encouraging indication for use of glycation inhibitors, yet there are no FDA approved drugs. In view of this, discovery of hydralazine as a transglycation agent has a great significance in controlling AGE levels and for the treatment of AGE induced diseases.
Previous studies have shown hydralazine inhibits glycation of low density lipoproteins and prevents foam cell formation in murine macrophages33. The drug was shown to inhibit in vivo AGE formation and improved renal damage in a type 2 diabetic nephropathy rat model34. These studies supported our finding of hydralazine as a tranglycating agent and AGE inhibitor. AGE accumulation is associated with up-regulation of RAGE expression and activation of AGE-RAGE axis leading to oxidative stress. In earlier studies hydralazine treatment resulted in decreased oxidative stress and lipid peroxidation35, perhaps this can be attributed to inhibition of AGE formation. Recent studies involving hydralazine as an acrolein scavenger36 support its ability of transglycation. Therefore, the drug has been suggested for the treatment of atherogenesis37, nervous system trauma38 and Alzheimers39. In this study for the first time we have unequivocally demonstrated the transglycating ability of hydralazine by in vitro and in vivo experiments including insulin transglycation by MALDI-TOF-MS, analysis of hydralazine-glucose conjugate, as well as proteome wide decrease in AGE modification of plasma proteins and AGE levels in plasma and kidney. The decrease in AGE modification and AGE levels was quite significant in comparison with a relatively higher dose of aminoguanidine treatment. Furthermore, hydralazine was able to reduce HbA1c and AGE levels quite faster when compared to aminoguanidine suggesting transglycation is a better intervention strategy. As hydralazine is already FDA approved drug for the treatment of hypertension, it has the potential to be repositioned for treatment of glycation induced diseases.
Methods
All chemicals were procured from Sigma-Aldrich unless otherwise mentioned. Hydralazine was generous gift from Dr. M. K. Gurjar, Director (R and D), Emcure, Pharmaceuticals and Pune. Antibodies for CML, RAGE, NOX and SOD were from Abcam (UK), pentosidine antibody from Cosmo Bio (Japan) and AGE antibody, secondary antibody-biotin conjugate, secondary antibody-HRP were purchased from Merck Millipore, (India), GOD-POD assay kit purchased from Beacon Diagnostics Pvt. Ltd, (India).
MALDI-TOF-MS based insulin transglycation assay
Insulin was glycated as described earlier13. The glycation of insulin was monitored for 7–10 days till the relative intensity showed 50% on MALDI-TOF-MS (Voyager, ABSCIEX). The excess glucose was removed by dialysis against MilliQ water, lyophilized and stored at −80°C until use. Removal of glucose was confirmed by GOD-POD assay (Beacon). The tranglycation assay was performed by incubating 50 μl of 1 mg/ml glycated insulin with 50 μl of 25 mM and 50 mM of hydralazine at 37°C for three hours and analyzed by MALDI-TOF-MS.
Glycation of human serum albumin (HSA)
In vitro glycation of pure HSA was done as described40 with slight modifications. Briefly, The reaction was carried out by incubationg 200 μl of 50 mg/ml HSA in 0.01 M phosphate buffer (pH 7.4) and 100 μl 0.5 M D-glucose containing 5 mM sodium azide as a bacteriostat with or without 100 μl of 25 mM and 50 mM (final concentration) of hydralazine at 37°C for 30 days. HSA glycation was monitored by fluorescence spectroscopy14 and LC-MSE 18,19.
Animal experiments and sample preparation
Ethics statement
The animal experiments were approved by Institutional Animal Ethics committee of National Centre for Cell Sciences, India. The experimental protocols were carried out in accordance with the guidelines of CPCSEA (Committee for the Purpose of Control and Supervision of Experiments on Animals), India.
Male BALB/c mice were injected with 50 mg/kg body weight of streptozotocin (STZ) in 50 mM citrate buffer pH 4.5 for five consecutive days to induce hyperglycemia, whereas control mice were injected with 50 mM citrate buffer41. The induction of diabetes was confirmed after 30 days by measuring the blood glucose levels with glucometer (Bayer, Germany) and HbA1C level by using HbA1C kit (Bayer Germany). Animals having blood glucose level above 6.12 ± 1.7 mmol/L with ≥7.0 HbA1C were selected for further studies. For each treatment eight animals were grouped into control, diabetic and diabetic treated with either hydralazine (300 mg/L)42 or aminoguanidine (2.4 g/L)43 for 60 days after induction of diabetes. Hydralazine and aminoguanidine was made available through drinking water as described43,44. Glucose and HbA1c levels were monitored on 30th, 45th, 60th and 90th day (0th, 15th, 30th and 60th day after initiation of drug treatment, respectively). Animals were euthanized at the end of study after 60 days of drug administration. Blood samples were collected and were immediately analyzed for blood glucose and HbA1c. Urine was collected in the last week of the experiment by maintaining them in Nalgene metabolomic cages after acclimatization for 24 h. Collected urine was stored at −80°C till analysis44. Plasma was obtained by EDTA treatment, which was then centrifuged at 1500 g for 5 min and the supernatant was stored at −80°C until further use. Total cholesterol, triglycerides, creatinine and blood urea nitrogen (BUN) concentrations were determined in plasma and protein and creatinine concentrations in urine with an automatic analyzer (Synchron CX7, Beckman Coulter Inc., Fullerton, CA). Kidney tissue was collected by snap freezing into liquid nitrogen. Later the tissue was perfused with cold phosphate buffer saline to remove blood stains prior to homogenization. The tissue was homogenized to fine powder in liquid nitrogen and the protein was extracted in buffer consisting of 7 M urea, 2 M thiourea, 2% CHAPS, 1% DTT, 40 mM Tris and centrifuged at 14,000 g for 30 min at 4°C. The supernatant was collected and stored in aliquots at −80°C. Protein concentration was determined by using Bio-Rad protein assay kit (Bio-Rad, Hercules, CA).
NBT Colorimetric fructosamine assay
Plasma fructosamine level was measured by using the NBT assay as described previously45. 200 μl of 0.75 mM NBT was added to a 96-well microplate containing 10 μl of the plasma. The reduction of NBT by fructosamine group was measured at 540 nm after incubation at 37°C for 30 min using an iMark microplate absorbance reader (Bio-Rad, Hercules, CA).
LC–MSE, protein identification, database search and PTM analysis
Prior to LC-MSE analysis plasma proteins and HSA were digested with trypsin after reduction and alkylation with 100 mM DTT and 200 mM iodoacetamide respectively. Two microliters (100 ng/μL) of digested peptides was spiked with 100 fm of enolase, was analyzed by using online nanoACQUITY UPLC coupled to a SYNAPT HDMS (Waters Corporation, Milford, MA) by MSE18. After MSE analysis, data were analyzed with Protein Lynx Global Server software (PLGS version 2.4 Waters Corporation, Milford, MA). A preliminary search of processed samples was performed for protein identification against the UniProt mice database containing 24382 protein entries. Glycation modification sites were identified by subjecting PLGS search against subset of protein databases that were identified in the preliminary search as described18,19. The false positive rate was set to 4% in the PLGS workflow. The PLGS identified glycation modifications were validated by following criteria. (a) accurate shift in precursor ion mass due to glycation (b) MS/MS spectra of glycated peptides should have at least seven fragments (c) the MS/MS spectra was analyzed for fragment mass error and fragment retention time error (d) glycated peptides should exist in at least two replications. An example of annotation of glycation modification has been shown in the supplementary data.
Extent of AGE modification of serum albumin
The extent of glycation modification was determined by analyzing the AGE modification of glucose sensitive peptides of serum albumin as described20 with a slight modification (supplementary Table 1). We have monitored the AGE modification of all the peptides containing the Glucose Sensitive Amino acid Residues (GSARs) (K44, R168, K210, K264, K438, R452) since trypsin digestion can generate different peptides containing these amino acid residues. The Cumulative Intensity Ratio (CIR) of AGE modified peptides containing GSAR to their unmodified form was monitored to quantify the extent of AGE modification. The CIR was used because the same GSAR can undergo various AGE modifications e.g. CEL, CML etc. and therefore it becomes important to consider the intensity of all the AGE modified peptides. The Cumulative Intensity Ratio (CIR) of AGE modified peptides containing GSAR to their unmodified form was monitored to quantify the extent of AGE modification.
Enzyme-linked immunosorbent assay
Each well of a 96-well microtiter plate was coated with 0.1 ml of 20 μg/ml of plasma/kidney protein sample in 50 mM carbonate buffer (pH 9.6) and incubated overnight at 4°C. The plate was washed three times with PBS containing 0.05% Tween 20 (Buffer A). Each well was blocked with 0.5% gelatin, washed with Buffer A and reacted with 0.1 ml of anti-AGE antibody (0.5 pg/ml). Then the wells were washed with buffer A, incubated with secondary antibody conjugated to alkaline phosphatase (Bangalore Genei, India) for 30 min. Thereafter the plate was washed and incubated in dark with PNPP (p-nitro phenyl phosphate) for 15 min and the reaction was stopped by addition of sulphuric acid (0.5 M, 10 ll per well). The absorbance of each well was recorded at 415 nm with an iMark microplate absorbance reader (Bio-Rad, Hercules, CA).
Western blotting
Plasma and kidney proteins were separated on 10% and 12% SDS-PAGE respectively and transferred onto the PVDF membrane. The membranes were blocked with 5% skimmed milk powder dissolved in TBS (20 mM Tris-HCl (pH 7.5), 0.15 M NaCl). Plasma proteins were probed for AGE modification by western blot analysis using antibodies against AGE, CML and pentosidine antibodies. While kidney proteins were probed for AGE modification, RAGE, NOX and SOD. Antibodies against actin served as loading control. Antibody dilution was adopted according to the manufacturer instructions. Corresponding biotinylated secondary antibody was used in 1:2000 dilution followed by incubation with streptavidin HRP conjugate Immunoreactive bands were visualized using DAB system (Sigma) and documented by Bio-Rad G-800 densitometer.
Synthesis of hydralazine glucose and hydralazine 13C-glucose conjugates
Hydralazine glucose conjugate (aldehydo-D-glucose phthalazin-1-ylhydrazone) was prepared by incubating 0.51 mmole of D-glucose and hydralazine hydrochloride with sodium acetate (1.02 mmole) in water: methanol (1:3)46. The reaction mixture was kept at boiling water bath for 10 min. Further the reaction was continued at room temperature for 16 hours. The product was filtered, washed with methanol and dried to obtain yellow, needle-like crystals of hydralazine glucose conjugate with quantitative yield. The product was characterized by FT-IR (Fourier Transform Infrared spectroscopy) Vmax 3306 (broad, NH and OH) 1647 (C = N) and 1563 cm-1(Ph) and HRMS (high resolution mass spectrometry) with accurate mass of 323.1384. (Supplementary Figure 9). The same reaction conditions were used to synthesize hydralazine-13C-glucose conjugate.
Urine analysis for the identification of Hydralazine glucose conjugates
To analyze hydralazine glucose conjugate in urine, urinary proteins were removed by ultrafiltration with 3 kD molecular weight cut-off filters. The filtrate was collected and kept in −80°C until use. The urinary metabolites were separated and analyzed as described earlier47. In brief 2 μl of sample was separated by Accela UPLC (Thermo Scientific) consisting of binary solvent system and a reverse phase Hypersil GOLD C18, 8 μm, 4.6 × 150 mm. The binary solvent system included 99.9% water and 0.1% formic acid (mobile phase A) and 99.9% acetonitrile and 0.1% formic acid (mobile phase B). Hydralazine glucose conjugate was eluted with a flow rate of 0.5 ml/min using sequential gradient of mobile phase B for 1–15% (0–3 min), 15–50% (3–6 min) and finally 50–95% (6–9 min). The UPLC was connected to online high resolution mass spectrometer Q- Exactive (Thermo Scientific), a hybrid quadrupole orbitrap mass analyzer. The mass spectra were acquired in high resolution (30000 FWHM) mode by using Xcalibur and data was processed by Quant software (Thermo Scientific). The method consisted of full scans and targeted MS/MS of selected precursor ion at a defined mass and retention time, with the following instrument parameters; microscans 1, AGC target 2e5 and Maximum injection time 120 ms. The retention time was determined by analyzing both labeled (13C) and unlabeled synthetic hydralazine glucose conjugate.
Hydralazine glucose conjugate was analyzed by constructing the XIC of selected fragment ions namely m/z 305.1244 and m/z 306.1278 of unlabeled and labeled (13C) synthetic hydralazine glucose conjugates (m/z 323.1350 and m/z 324.1384) respectively. The standard curve was developed by plotting the log10 value of area under curve (AUC) of the selected fragment (m/z 305.1244) XIC against log10 value of various concentrations of synthetic hydralazine glucose conjugate ranging from 40 fg to 4 ng. All the XIC were extracted with an accuracy of 3 ppm. An optimum concentration of 500 pg/ml of labeled hydralazine conjugate was spiked as an internal standard into the urine samples. Hydralazine glucose conjugate from urine sample was identified and quantified by comparing the XIC of selected fragment ion (m/z 305.1244).
Statistical analysis
All experiments were performed in triplicates. Statistical analysis was performed by Student's t-test. Data are expressed as means ± SD. A p-value < 0.05 was considered as statistically significant.
References
Brownlee, M. Biochemistry and molecular cell biology of diabetic complications. Nature 414, 813–820 (2001).
Piperi, C., Adamopoulos, C., Dalagiorgou, G., Diamanti-Kandarakis, E. & Papavassiliou, A. G. Crosstalk between Advanced Glycation and Endoplasmic Reticulum Stress: Emerging Therapeutic Targeting for Metabolic Diseases. J Clin Endocrinol Metab. 97, 2231–2242.
Brownlee, M. D. M. Advaced protein glycosylation in diabetes and aging. Annu Rev Med. 46, 223–234 (1995).
Kulkarni, M. J., Korwar, A. M., Mary, S., Bhonsle, H. S. & Giri, A. P. Glycated proteome: From reaction to intervention. Proteomics Clin Appl. 7, 155–170 (2013).
Brownlee, M., Vlassara, H., Kooney, A., Ulrich, P. & Cerami, A. Aminoguanidine prevents diabetes-induced arterial wall protein cross-linking. Science 232, 1629–1632 (1986).
Miyata, T. et al. 2-Isopropylidenehydrazono-4-oxo-thiazolidin-5-ylacetanilide (OPB-9195) treatment inhibits the development of intimal thickening after balloon injury of rat carotid artery: role of glycoxidation and lipoxidation reactions in vascular tissue damage. FEBS Lett. 445, 202–206 (1999).
Forbes, J. M. et al. Renoprotective effects of a novel inhibitor of advanced glycation. Diabetologia 44, 108–114 (2001).
Beisswenger, P. & Ruggiero-Lopez, D. Metformin inhibition of glycation processes. Diabetes Metab. 29, 6S95–6S103 (2003).
Huby, R. & Harding, J. J. Non-enzymic glycosylation (glycation) of lens proteins by galactose and protection by aspirin and reduced glutathione. Exp Eye Res. 47, 53–59 (1988).
van Boekel, M. A. M., van den Bergh, P. J. P. C. & Hoenders, H. J. Glycation of human serum albumin: inhibition by Diclofenac. Biochim Biophys Acta 1120, 201–204 (1992).
Szwergold, B. S., Howell, S. & Beisswenger, P. J. Human Fructosamine-3-Kinase. Diabetes 50, 2139–2147 (2001).
Szwergold, B. S., Howell, S. K. & Beisswenger, P. J. Transglycation–A Potential New Mechanism for Deglycation of Schiff's Bases. Ann N Y Acad Sci. 1043, 845–864 (2005).
Golegaonkar, S. B., Bhonsle, H. S., Boppana, R. & Kulkarni, M. J. Discovery of rifampicin as a new anti-glycating compound by matrix-assisted laser desorption/ionization mass spectrometry-based insulin glycation assay. Eur J Mass Spectrom (Chichester, Eng). 16, 221–6 (2010).
Yanagisawa, K. et al. Specific fluorescence assay for advanced glycation end products in blood and urine of diabetic patients. Metabolism 47, 1348–53 (1998).
Silva, J. C., Gorenstein, M. V., Li, G.-Z., Vissers, J. P. C. & Geromanos, S. J. Absolute Quantification of Proteins by LCMSE: A Virtue of Parallel ms Acquisition. Mol Cell Proteomics 5, 144–156 (2006).
Xie, H., Gilar, M. & Gebler, J. C. Characterization of Protein Impurities and Site-Specific Modifications Using Peptide Mapping with Liquid Chromatography and Data Independent Acquisition Mass Spectrometry. Anal Chem. 81, 5699–5708 (2009).
Blackburn, K. & Goshe, M. B. Challenges and strategies for targeted phosphorylation site identification and quantification using mass spectrometry analysis. Brief Funct Genomic Proteomic. 8, 90–103 (2009).
Bhonsle, H. S. et al. Low Plasma Albumin Levels Are Associated with Increased Plasma Protein Glycation and HbA1c in Diabetes. J Proteome Res. 11, 1391–1396 (2012).
Bansode, S. B. et al. Proteomic Analysis of Protease Resistant Proteins in the Diabetic Rat Kidney. Mol Cell Proteomics 12, 228–236 (2013).
Zhang, M. X. W. & Deng, Y. A New Strategy for Early Diagnosis of Type 2 Diabetes Mellitus by Standard-Free, Label-Free LC-MS/MS Quantification of Glycated Peptides. Diabetes E-pub (2013).
Makita, Z. et al. Advanced Glycosylation End Products in Patients with Diabetic Nephropathy. N Engl J Med. 325, 836–842 (1991).
Yan, S. F., Ramasamy, R., Naka, Y. & Schmidt, A. M. Glycation, Inflammation and RAGE: A Scaffold for the Macrovascular Complications of Diabetes and Beyond. Circ Res. 93, 1159–1169 (2003).
Peyroux, J. & Sternberg, M. Advanced glycation endproducts (AGEs): pharmacological inhibition in diabetes. Pathol Biol (Paris). 54, 405–419 (2006).
Khalifah, R. G., Chen, Y. & Wassenberg, J. J. Post-Amadori AGE Inhibition as a Therapeutic Target for Diabetic Complications: A Rational Approach to Second-Generation Amadorin Design. Ann N Y Acad Sci. 1043, 793–806 (2005).
Khalifah, R. G., Baynes, J. W. & Hudson, B. G. Amadorins: Novel Post-Amadori Inhibitors of Advanced Glycation Reactions. Biochem Biophys Res Commun. 257, 251–258 (1999).
Ruggiero-Lopez, D. et al. Reaction of metformin with dicarbonyl compounds. possible implication in the inhibition of advanced glycation end product formation. Biochem Pharmacol. 58, 1765–1773 (1999).
Asif, M. et al. An advanced glycation endproduct cross-link breaker can reverse age-related increases in myocardial stiffness. Proceed Natl Acad Sci. 97, 2809–2813 (2000).
Costantino, L., Rastelli, G., Vianello, P., Cignarella, G. & Barlocco, D. Diabetes complications and their potential prevention: Aldose reductase inhibition and other approaches. Med Res Rev. 19, 3–23 (1999).
Shinohara, M. et al. Overexpression of glyoxalase-I in bovine endothelial cells inhibits intracellular advanced glycation endproduct formation and prevents hyperglycemia-induced increases in macromolecular endocytosis. J Clin Invest. 101, 1142–1147 (1998).
Goova, M. T. et al. Blockade of Receptor for Advanced Glycation End-Products Restores Effective Wound Healing in Diabetic Mice. Am J Pathol. 159, 513–525 (2001).
Shakkottai, V. G., Sudha, R. & Balaram, P. Gramicidin S: a peptide model for protein glycation and reversal of glycation using nucleophilic amines. J Pept Res. 60, 112–120 (2002).
Babizhayev, M. A., Micans, P., Guiotto, A. & Kasus-Jacobi, A. N-Acetylcarnosine Lubricant Eyedrops Possess All-In-One Universal Antioxidant Protective Effects of L-Carnosine in Aqueous and Lipid Membrane Environments, Aldehyde Scavenging and Transglycation Activities Inherent to Cataracts: A Clinical Study of the New Vision-Saving Drug N-Acetylcarnosine Eyedrop Therapy in a Database Population of Over 50,500 Patients. Am J Ther. 16, 517–533, 10.1097/MJT.0b013e318195e327 (2009).
Brown, B. E., Mahroof, F. M., Cook, N. L., Reyk, D. M. & Davies, M. J. Hydrazine compounds inhibit glycation of low-density lipoproteins and prevent the in vitro formation of model foam cells from glycolaldehyde-modified low-density lipoproteins. Diabetologia 49, 775–783 (2006).
Rodrigues, B., Goyal, R. K. & McNeill, J. H. Effects of hydralazine on streptozotocin-induced diabetic rats: prevention of hyperlipidemia and improvement in cardiac function. J Pharmacol Exp Ther. 237, 292–299 (1986).
Burcham, P. C., Kaminskas, L. M., Fontaine, F. R., Petersen, D. R. & Pyke, S. M. Aldehyde-sequestering drugs: tools for studying protein damage by lipid peroxidation products. Toxicology 181–182, 229–236 (2002).
Kaminskas, L. M., Pyke, S. M. & Burcham, P. C. Strong Protein Adduct Trapping Accompanies Abolition of Acrolein-Mediated Hepatotoxicity by Hydralazine in Mice. J Pharmacol Exp Ther. 310, 1003–1010 (2004).
Galvani, S. et al. Carbonyl scavenger and antiatherogenic effects of hydrazine derivatives. Free Radic Biol Med. 45, 1457–67 (2008).
Nickerson, M. & Carter, S. A. Protection against acute trauma and traumatic shock by vasodilators. Can J Biochem Physiol. 37, 1161–1171 (1959).
Wang, J. et al. Valsartan lowers brain beta-amyloid protein levels and improves spatial learning in a mouse model of Alzheimer disease. J Clin Invest. 117, 3393–3402 (2007).
Lapolla, A. et al. Advanced glycation end products: a highly complex set of biologically relevant compounds detected by mass spectrometry. J Mass Spectrom. 36, 370–378 (2001).
Batirel, S., Yarat, A. & Emekli, N. Effects of short-term streptozotocin-induced diabetes and vitamin C on platelet non-enzymatic glycation. Pathophysiol Haemost Thromb. 37, 72–6.
Chen, J., Kuhlencordt, P. J., Astern, J., Gyurko, R. & Huang, P. L. Hypertension Does Not Account for the Accelerated Atherosclerosis and Development of Aneurysms in Male Apolipoprotein E/Endothelial Nitric Oxide Synthase Double Knockout Mice. Circulation 104, 2391–2394 (2001).
Youssef, S. et al. Effect of diabetes and aminoguanidine therapy on renal advanced glycation end-product binding. Kidney Int. 55, 907–916 (1999).
Salek, R. M. et al. A metabolomic comparison of urinary changes in type 2 diabetes in mouse, rat and human. Physiol Genomics 29, 99–108 (2007).
Chen, L., Wei, Y., Wang, X. & He, R. Ribosylation Rapidly Induces alpha-Synuclein to Form Highly Cytotoxic Molten Globules of Advanced Glycation End Products. PLoS ONE 5, e9052 (2010).
Shaban, M. A. E., Ali, R. S. & El-Badry, S. M. The synthesis of 3-(alditol-1-yl)-1,2,4-triazolo[3,4-a]phthalazines. Carbohydr Res. 95, 51–60 (1981).
Want, E. J. et al. Global metabolic profiling procedures for urine using UPLC-MS. Nat. Protocols 5, 1005–1018 (2010).
Acknowledgements
Authors thank Dr. Sourav Pal, Director, CSIR-NCL and Dr. Vidya Gupta, Chair, Division of Biochemical Sciences for their support and encouragement. This work is supported by CSIR Empower project OLP002926 and Network project CSC0111. We are thankful to Dr. Mukund Gurjar, Director (R & D), Emcure Pharmaceuticals, Pune for providing hydralazine and Dr. Jomon Joseph for providing antibody against actin. S.K.K., S.B., A.B.D., S.B.G. thank CSIR and UGC India for the Senior Research fellowship.
Author information
Authors and Affiliations
Contributions
M.J.K. conceived the idea, designed, supervised the study and written the manuscript. S.K.K. developed MALDI based assay for transglycation and carried out the animal experiments. S.B., S.B.G. and S.D.B. have carried out western blotting and proteomic analysis including protein extraction, digestions and mass spectrometric acquisitions. M.G.J. and A.B.D. were involved in mass spectrometric data analysis, M.L.S. helped in animal experiments and carried out biochemical analysis, H.V.T. and H.S.P. synthesized labeled hydralazine glucose conjugate and designing metabolite analysis. S.K.K., S.B.G. and M.G.J. carried out metabolite analysis. R.B. designed the animal experiment and reviewed the manuscript. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Combined supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Kesavan, S., Bhat, S., Golegaonkar, S. et al. Proteome wide reduction in AGE modification in streptozotocin induced diabetic mice by hydralazine mediated transglycation. Sci Rep 3, 2941 (2013). https://doi.org/10.1038/srep02941
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep02941
This article is cited by
-
Hydralazine targets cAMP-dependent protein kinase leading to sirtuin1/5 activation and lifespan extension in C. elegans
Nature Communications (2019)
-
Proteomics in India: the clinical aspect
Clinical Proteomics (2016)
-
Potential Dual Role of Eugenol in Inhibiting Advanced Glycation End Products in Diabetes: Proteomic and Mechanistic Insights
Scientific Reports (2016)
-
Effect of diabetic duration on hemorheological properties and platelet aggregation in streptozotocin-induced diabetic rats
Scientific Reports (2016)
-
Strategy to enhance efficacy of doxorubicin in solid tumor cells by methyl-β-cyclodextrin: Involvement of p53 and Fas receptor ligand complex
Scientific Reports (2015)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.