Abstract
This retrospective cohort study investigated the progression risk of sequential complication in Asian type 2 diabetes (T2D) patients using the Taiwan Pay-for-Performance Diabetes Registry and claim data from November 2003 to February 2009. 226,310 adult T2D patients without complication were followed from diagnosis to complications, including myocardial infarction (MI), other ischemic heart disease (IHD), congestive heart failure (CHF), stroke, chronic kidney disease (CKD), retinopathy, amputation, death or to the end of study. Cumulative incidences (CIs) of first and second complications were analyzed in 30 and 4 years using the cumulative incidence competing risk method. IHD (29.8%), CKD (24.5%) and stroke (16.0%) are the most common first complications. The further development of T2D complications depends on a patient’s existing complication profiles. Patients who initially developed cardiovascular complications had a higher risk (9.2% to 24.4%) of developing IHD or CKD, respectively. All-cause mortality was the most likely consequence for patients with a prior MI (12.0%), so as stroke in patients with a prior MI (10.8%) or IHD (8.9%). Patients with CKD had higher risk of developing IHD (16.3%), stroke (8.9%) and all-cause mortality (8.7%) than end-stage renal disease (4.0%). Following an amputation, patients had a considerable risk of all-cause mortality (42.1%).
Similar content being viewed by others
Introduction
Type 2 diabetes (T2D) is a common chronic disease characterised by progressive, interdependent but partially preventable complications, including cardiovascular diseases (CVDs), stroke, chronic kidney disease (CKD) and retinopathy1,2,3. Poorly-controlled diabetes is associated with a significantly increased morbidity and mortality resulting in an enormous healthcare burden4.
A rapid escalation of diabetes prevalence has been noted in Asian populations and this has become a global public health concern. The International Diabetes Federation predicts the number of people with diabetes worldwide will rise from 366 million in 2011 to 552 million by 2030, with half of this increase arising from Asia. Of the anticipated 186 million new diabetic cases, 39 million are expected from China and India, the two countries with the largest diabetic populations5. Consequently, provision of diabetic care presents particular challenges for this region6.
A range of evidence-based clinical guidelines7,8 have been developed to recommend optimal diabetes management strategies based on large randomised controlled trials, such as the Diabetes Control and Complications Trial9 and United Kingdom Prospective Diabetes Study1 and several epidemiological studies also inform risks of long-term complication in diabetes1,2. However, epidemiological data studying the development of complications in Asian patients with diabetes are limited.
Sub-group analysis in several Western studies suggested that key diabetes complications in Asian ethnicity differ from their Western counterparts10, for example, Asian diabetic patients have lower risks of CVDs and amputation11,12,13,14, but are more likely to develop nephropathy15,16,17 and retinopathy18. An improved understanding of these differences in susceptibility to develop complications may contribute to the development of effective screening and treatment strategies and lead to improvements in quality of care Asian diabetic patients19.
In addition, previous epidemiological research in quantifying the risk of diabetes-associated complications mostly reported the risk of first complication and assessed individual complications in isolation without considering patients’ complications profiles11,12,13,14,20 However, patients who have developed a complication, may consequently be more likely to develop another specific complication7.
A competing risk is an event that may hinder the observation of a clinical event or that may modify the chance for the occurrence of event. Therefore, a competing risk analysis incorporating sequential complications may be a better alternative to mostly used standard survival analysis methods, i.e. the Kaplan-Meier (KM) estimates and Cox regression. Indeed, Abbasi et al. (2013) who developed a risk prediction model of diabetes complications from literature also suggested that current analysis of diabetic progression of complications (without considering competing risk) greatly obscures the estimate on risk of complications across patients with various disease profiles20.
This study aimed to investigate the development of complications in T2D patients who have no complication at the diagnosis of diabetes using a longitudinal population-based database. The long-term cumulative incidence (CIs) of first and second major complications after the diagnosis of diabetes was analysed considering each complication as a competing risk to another within a single analytic framework rather than treating each clinical event separately, which encompasses the interactions between complications in estimating the risk of diabetes progression21,22,23.
Results
Characteristics of patients
Of all, 226,310 T2D patients (1,882,341 patient-years, median: 6.7 years) were included, 51.0% were female. The mean age of diagnosis was 53.0 ± 11.9 (range: 18.5, 98.1) and the mean duration of diabetes was 5.6 ± 6.3 (range: 0, 61.5) years. At baseline, the cohort’s mean haemoglobin A1c (HbA1c) level was 8.5 ± 2.10% (69.4 ± 23.1 mmol/mol); mean body mass index (25.8 ± 4.0 kg/m2), fasting triglycerides (176.6 ± 175.5 mg/dl) and low-density-lipoprotein cholesterol (119.1 ± 35.3 mg/dl) were slightly higher than normal; while mean systolic (133.65 ± 18.16 mmHg) and diastolic (79.9 ± 10.8 mmHg) blood pressures were within normal range (Appendix 1).
Diabetic complications
Overall, 69,440 (30.7%) patients had developed at least one incidence of complication identified during the study period (Fig. 1). The total number of first and second complications identified including 2,702 myocardial infarction (MI), 33,319 other ischemic heart disease (IHD), 5,197 congestive heart failure (CHF), 17,176 stroke, 24,410 CKD, 38 amputation, 2,877 laser photocoagulation, 663 treatments for detached retina or vitreous haemorrhage and 4,264 (1,122 first and 3,142 second complications) all-cause mortality. In addition, recurrent events including 21 MI, 2,924 IHD, 297 CHF, 186 strokes and 617 end-stage renal diseases (ESRD) were identified at the second stage (Table 1).
Cumulative incidence of the first complication
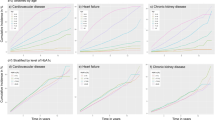
The 30-year cumulative incidences of first IHD, CKD and stroke (at the first stage) were found to be higher than other complications in all possible transitions after the diagnosis of diabetes (Fig. 2). The annual incidence of IHD, CKD and stroke ranged between 0.3% and 1.4%, resulting in a cumulative incidence of 6.8%; 4.5% and 2.9% after 5 years; 12.8%, 8.9% and 5.9% after 10 years; 23.1%; 18.0% and 11.8% after 20 years; and 29.8%, 24.5% and 16.0% respectively after 30 years. In contrast, the 30-year cumulative incidence of CHF, MI, retinopathy, amputation and all-cause mortality were lower than 4.0%.
Overall, 45,311 of the 69,440 (65.3%) patients only developed one complication during the study period. The proportions of patients developed a further complication varied and ranged from 25.1% (570/2272) in patients who developed retinopathy as the first complication and received laser photocoagulation, to 57.4% (1677/2923) in patients who developed CHF as their first complication (Table 2).
Cumulative incidence of the second complication
Of the 24,129 patients who experienced more than one complication, patients with a prior CVD (MI, IHD, CHF and stroke) as the first complication, the 4-year cumulative incidence of progression was higher to IHD and CKD but lower to MI, retinopathy and amputation (Table 2). For instance, for patients with a prior CHF, the 4-year cumulative incidence of progression was higher to IHD (24.4%) and CKD (14.7%) but lower to MI (1.6%) and retinopathy (0.4% and 0.1%). In particular, the 4-year cumulative incidences of progressing to IHD were markedly high in patients with CHF (24.4%) and stroke (18.8%) and the incidences of progressing to stroke were also noticeably high in patients with MI (10.8%) and IHD (8.9%).
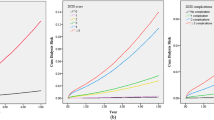
The 4-year incidence of recurrent CVDs (Fig. 3) was higher in patients with a prior IHD (12.8%) and CHF (12.7%) than patients with a prior MI (1.6%) and stroke (1.9%). All-cause mortality was the most likely consequence for patients with a prior MI (4-year incidence 12.0%) and it was also one of the largest threats for patients with a prior CHF (9.5%) and stroke (8.0%). It is also noteworthy that patients with a prior CHF had the lowest likelihood for staying without progression (4-year incidence 27.6%) comparing to patients with other cardiovascular complications.
For diabetic patients with a prior CKD, the 4-year cumulative incidences of progression to IHD (16.3%), stroke (8.9%) and all-cause death (8.7%) were higher than other complications (Fig. 4). Although ESRD is regarded as the renal complication that is likely to develop in patients with a prior CKD, the risk of progression to ESRD (3.98%) in patients with a prior CKD was lower than the risk of progression to other CVDs.
For diabetic retinopathy patients who either received laser photocoagulation or treatments for detached retina or vitreous haemorrhage, the 4-year cumulative incidence of progression was high to CKD (12.0%; 15.8%) and IHD (12.3%; 9.1%); moreover, the 4-year cumulative incidence of receiving laser photocoagulation for a new lesion was appreciable (9.3%). Finally, diabetic patients who received amputation had a considerable 4-year cumulative all-cause mortality of 42.1%.
Discussion
This study investigated the progressive development of diabetes complications in a large cohort of Asian Chinese T2D patients by modelling the first and second major complications in a single analytical framework. Adult patients enrolled in the Taiwan Diabetes Pay-for-Performance (PFP) Registry were more likely to develop IHD, CKD and stroke than to develop MI, CHF, retinopathy and amputation as the first complication that need emergency or inpatient care. In addition, we found the risk of developing a second complication varies by patients’ existing complication profiles prior to the occurrence of further complications.
For patients with a prior CVD (MI, IHD, CHF and stroke), the risk of developing a further IHD and CKD was markedly higher than other complications and stroke was one of the major complications for diabetic patients with a previous MI. Diabetic patients with CKD faced a higher risk of progressing to CVDs and all-cause mortality than progressing to ESRD within 4 years posterior to the diagnosis of CKD. The presence of retinopathy also contributed to an increased risk of impairing renal function. These results are expected based on previous epidemiological studies24,25,26.
Previous studies that have examined the risks of multiple diabetic complications mostly only reported the first occurrence of MI, CHF, stroke, ESRD and lower-extremity amputation (LEA) after diagnosis of diabetes as age- and sex-adjusted number of events per 1,000 patient-years. These studies also compared complication risks among different ethnic subgroups (Chinese and Asian patients) with whites in Canada13,14 and the United States11,12. In general, these studies showed the incidence of developing CVDs was significantly higher than the incidence of developing ESRD and LEA in Chinese diabetic patients.
For example, studies using the Kaiser Permanente Northern California Diabetes Registry11,12 and Canadian government-funded insurance programme in Ontario14 found that the risk of stroke (3.0–7.2/1000 person-year) was lower than MI (3.6–9.3/1000 person-year) during a 8-year study period (median follow up was 4.7 years) but slightly larger than CHF (2.5–5.9 /1000 person-year) for Chinese diabetes patients resident in Western countries and this is different from the risk of the first complication estimated in our study.
However, another Canadian study using the administrative data from British Columbia and Alberta found that the risk of stroke (4.1–4.2/1000 person-year) is higher than MI (1.5–2.8/1000 person-year) and CHF (2.3–2.0/1000 person-year)13 for Chinese patients, which is similar to our findings. The discrepancies in complication risks reported for Chinese diabetic patients residing in different areas may be due to the variations in research settings, sample sizes, criteria used to identify complications and follow-up time and hence warrants further exploration.
The previous studies11,12,13,14 also reported that white diabetes patients had a significantly higher risk of developing CVDs as the first complication than ESRD and LEA; of the CVDs, the highest risk was MI and the risks of stroke and CHF were approximately equivalent. Comparing with these findings, our study also demonstrated the risk of amputation was the lowest among diabetic complications. However, our patients were at relatively lower risk to develop CHF and MI, instead more likely to develop the non-fatal coronary heart disease (i.e. IHD) as the first complication.
It has been widely reported in the literature that for the first complication occurring in Asian diabetes patients, the prevalence of diabetic nephropathy was higher15,17 and there was a lower prevalence of ESRD than CVDs. However, there is a paucity of data on comparing the risk of CKD with other diabetic complications in both Asians and whites. In our analysis, the risk of CKD as the first complication was higher than stroke, CHF, MI and retinopathy; and diabetic patients with CKD were at a lower risk of developing further ESRD than CVDs, except for MI.
This study also identified a high risk of CKD in patients with existing CVDs. Although the effect of prevalent CVD on developing a further kidney disease has been poorly investigated in prior reports, our findings are comparable to the results of a large community-based cohort study, which examined the association between CVD and subsequent kidney function decline and development of kidney disease27. Several CKD prediction models have also shown that CVD, stroke and CHF were the risk factors for the occurrence of CKD28,29,30.
The observations listed above, together with the noticeable risk of CKD after retinopathy, suggests that diabetic patients with either micro- or macro-vascular complication in this study were inclined to develop CKD, thereby threatening to cause fatal or disabling events, with a significant potential for progressing to ESRD or another cardiovascular complication. Early identification of CKD allows the best opportunity to initiate therapy to reduce renal risk factors and decelerate the loss of kidney function31, therefore, routinely monitoring kidney function should be recommended for diabetic patients in these high-risk groups. At present, routine kidney function monitoring (serum creatinine and urine albumin-to-creatinine ratio every 3 to 6 months) is recommended by the Taiwan Society of Nephrology and diabetologists are also encouraged to refer diabetic patients to the Taiwan National Health Insurance (NHI) early-CKD and pre-ESRD PFP Programmes.
The risk of all-cause mortality for patients who received amputation as the first complication after diabetes was as high as 42.14%. A number of studies have shown a high mortality (about 50% at 3 years) following amputation of a limb in patients with various diabetes complications32,33. However, it is surprised to observe this in patients who had no other complication except for diabetic foots. We hypothesise this result could be associated with patients’ socioeconomic background or inhabitant in remote area, as patients did not access any healthcare before diabetes progressed. Further studies should be carried out to test this hypothesis when relevant information is available.
To our knowledge, this study is one of the largest study populations with the longest follow-up published to date on disease progression of Asian diabetic patients. The large number of study cohort and the comprehensive PFP medical records increase the validity of identifying relevant clinical outcomes in diabetes progression. This study is also the first to investigate changes in the type and number of major diabetic complications within a single analytic framework. It also comprehensively captured different pathways in which diabetic complications or composite complications occurred and thereby enabled identifying the most likely events among all possible increased risks after diabetes.
However, this study has several limitations. First, the baseline clinical indicators in the PFP Diabetes Registry were collected after November 2003, which varied for individuals at different stages of disease progression and therefore clinical indicators (e.g. laboratory data) were not appropriate for adjustment. In addition, this study aimed to quantify the long-term cumulative incidence of first and second major complications after diabetes rather than compare results across different subgroups. Moreover, the results are consistent after adjusting for age and gender in a single-cause competing risk model; hence the unadjusted results were reported.
Second, the selection bias is acknowledged as contracted physicians have the discretion to enrol patients in an incentivised payment scheme. Previous studies also have indicated diabetic patients enrolled in the PFP scheme were healthier than those who were not recruited34,35. This study also found the cumulative incidences of complications were relatively low. Therefore, it should be cautious in applying the observed relation between sequential complications to diabetic patients with poor health.
Third, for patients who were diagnosed as diabetic before enrolment or November 2003, the self-reported diagnosed year cannot be confirmed and this may have caused recall bias and obscured some observed disease progression. Finally, there was no information on the medication and treatment of patients before November 2003 and hence it is unclear whether some patients received amputation or any treatment for retinopathy during this period.
The progression of diabetes in Asian patients is different from that reported in western countries. IHD, CKD and stroke are more likely the first complication than CHF, MI, retinopathy and amputation for Asian patients. Risk for developing a further complication varies according to patients’ existing complication profiles and patients with an existing cardiovascular complication or retinopathy have a higher risk of developing IHD and CKD. These results inform the clinical decisions on prioritising monitoring and interventions for Asian diabetic patients who are at high risk of developing severe complications in this region.
Methods
Study design and data source
This retrospective cohort study was conducted using the Taiwan PFP Diabetes Registry from November 2003 to February 2009 after being granted approval from the Department of Health (DOH97-NH-1017) in Taiwan. The study protocol was also approved by the Institutional Review Board of Kaohsiung Medical University Hospital (KMUH-IRB-EXEMPT-20130038). All research procedures followed the directives of the Declaration of Helsinki.
The PFP Programme for Diabetes in Taiwan is one of the nationwide PFP programmes implemented since 200136. It incentivises healthcare providers to deliver comprehensive monitoring and follow-up care by additional bonus payment. Contracted physicians and hospitals participate in the programme on a voluntary basis and have the discretion to recruit patients into the programme35.
The PFP Diabetes Registry contains detail information of registered diabetes patients, such as demography (age, gender), past medical history, diabetes-specific physical examinations and laboratory data recorded at each follow-up visit. In addition, the PFP Diabetes Registry also links to the full NHI claim database of registered diabetes patients, such as outpatient and inpatient medical claims and dispensing claims from community pharmacies, thus allows a valid estimate of treatment outcomes measures in this longitudinal follow-up study.
All the NHI claim data and PFP Diabetes Registry data are anonymous and detailed description of the regular NHI claim database has been reported elsewhere37. The PFP database together with NHI claim database provides rich data to investigate patients’ diabetic progression.
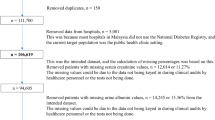
Study cohort
Adults (aged 18 and above) with either incident or prevalent T2D who met the inclusion criteria: (1) were enrolled in the PFP programme before February 2009, (2) diabetes diagnosed date (disease index date) was identifiable and (3) had no recorded diabetic complication before diagnosed date were included in this study. Patients’ medical claim data between November 2003 and February 2009 were extracted from the NHI claim database. To ensure the included patients had no diabetic compilation, those who had any diabetic complications recorded before 30 April 2004 (i.e. 6 months after beginning of follow-up) were excluded from this study.
Patients’ diabetes index dates were identified based on records in the PFP Registry. For patients whose diabetes was diagnosed before their enrolment into the programme or before November 2003, only ‘diagnosed year’ is available in the Registry and hence June 30th of the year was used as the index date for those patients. The identified cohort was followed from individual diabetes index date to complications, death or the end of study, whichever occurred first.
Outcome measure
The primary outcomes of this study were incidences of eight diabetes-related complications during the follow-up period, including MI, IHD (excluding MI), CHF, stroke, CKD and ESRD, retinopathy (defined as receiving laser and vitreoretinal surgery), amputation and all-cause mortality, that required inpatient or emergency care.
The outcome events and event dates were identified by screening the corresponding International Classification of Diseases, Ninth Revision (ICD-9) diagnosis or procedure codes38 and therapeutic medicines recorded in the NHI claim database for emergency or inpatient care (Appendix 2) and several exclusion criteria were applied to ensure the occurrence of incidences (Table 3). For a mortality event, the mortality date was retrieved from the Registry, otherwise it was defined as three months after the patient’s last record in the NHI claim database as it is unusual that a diabetic patient will not access NHI healthcare in Taiwan39.
Data analysis
All outcome events for individual patient were chronologically sequenced according to the event dates. The analysis focused on two disease progression stages, including: (1) the first stage—patients progressed from no complication to the first outcome incident occurring and (2) the second stage—patients progressed after the first event to when the second outcome event occurred. The observation end point in the first stage was any incidence of MI, IHD, CHF, stroke, CKD, amputation, receiving laser and vitreoretinal surgery and all-cause mortality. In the second stage, ESRD and recurrence (i.e. any repeat episode need inpatient or emergency care) of MI, IHD, CHF and stroke were recorded as the progression of cardiovascular and renal complications, instead of incident events (Fig. 5).
Conceptual framework for the pathway of first two events of diabetic complications.
(Note) DM: diabetes mellitus; MI: myocardial infarction; IHD: ischemic heart disease; CHF: congestive heart failure; CKD: chronic kidney disease; ESRD: End Stage Renal Disease; Laser: patients received laser photocoagulation; Detached retina: patients received treatments for detached retina or vitreous haemorrhage.
Event and time-to-event were calculated for each stage and patients who remained in a same event stage were followed to the end of study. Descriptive statistics were used to report enrolled patients’ demographic and clinical characteristics. Cumulative incidences of the first events over 30 years and the second events over 4 years were calculated using the Kaplan-Meier cumulative incidence competing risk method. All data were processed using SAS software, version 9.2 (SAS Institute Inc.). The competing risk analysis was conducted by using R statistical programme, version 3.0.2, with the cmprsk package.
Additional Information
How to cite this article: Cheng, L.-J. et al. A competing risk analysis of sequential complication development in Asian type 2 diabetes mellitus patients. Sci. Rep. 5, 15687; doi: 10.1038/srep15687 (2015).
References
Clarke, P. M. et al. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia 47, 1747–1759 (2004).
Fox, C. S. et al. Trends in cardiovascular complications of diabetes. JAMA 292, 2495–2499 (2004).
Morrish, N. J., Wang, S. L., Stevens, L. K., Fuller, J. H. & Keen, H. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia 44 Suppl 2, S14–21 (2001).
American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care 36, 1033–1046 (2013).
Chan, J. C. et al. Diabetes in Asia: epidemiology, risk factors and pathophysiology. JAMA 301, 2129–2140 (2009).
Vinicor, F. The public health burden of diabetes and the reality of limits. Diabetes Care 21 Suppl 3, C15–18 (1998).
American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care 36 Suppl 1, S11–66 (2013).
National Collaborating Centre for Chronic Conditions. Type 2 diabetes: national clinical guideline for management in primary and secondary care (update). (Royal College of Physicians, 2008).
The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med 329, 977–986 (1993).
Woodward, M. et al. The effects of diabetes on the risks of major cardiovascular diseases and death in the Asia-Pacific region. Diabetes Care 26, 360–366 (2003).
Kanaya, A. M. et al. Heterogeneity of diabetes outcomes among asians and pacific islanders in the US: the diabetes study of northern california (DISTANCE). Diabetes Care 34, 930–937 (2011).
Karter, A. J. et al. Ethnic disparities in diabetic complications in an insured population. JAMA 287, 2519–2527 (2002).
Khan, N. A. et al. Ethnicity and sex affect diabetes incidence and outcomes. Diabetes Care 34, 96–101 (2011).
Shah, B. R. et al. Cardiovascular complications and mortality after diabetes diagnosis for South Asian and Chinese patients: a population-based cohort study. Diabetes Care 36, 2670–2676 (2013).
Bhalla, V. et al. Racial/ethnic differences in the prevalence of proteinuric and nonproteinuric diabetic kidney disease. Diabetes Care 36, 1215–1221 (2013).
Hall, Y. N. et al. The conundrum of increased burden of end-stage renal disease in Asians. Kidney Int 68, 2310–2316 (2005).
Wu, A. Y. et al. An alarmingly high prevalence of diabetic nephropathy in Asian type 2 diabetic patients: the MicroAlbuminuria Prevalence (MAP) Study. Diabetologia 48, 17–26 (2005).
Li, Y., Liao, Y., Fan, A., Zhang, X. & Balluz, L. Asian American/Pacific Islander paradox in diabetic retinopathy: findings from the Behavioral Risk Factor Surveillance System, 2006-2008. Ethn Dis 20, 111–117 (2010).
Lanting, L. C., Joung, I. M., Mackenbach, J. P., Lamberts, S. W. & Bootsma, A. H. Ethnic differences in mortality, end-stage complications and quality of care among diabetic patients: a review. Diabetes Care 28, 2280–2288 (2005).
Abbasi, A. et al. Prediction models for risk of developing type 2 diabetes: systematic literature search and independent external validation study. BMJ (Clinical research ed.) 345, doi: http://dx.doi.org/10.1136/bmj.e5900 (2012).
Putter, H., Fiocco, M. & Geskus, R. B. Tutorial in biostatistics: competing risks and multi-state models. Stat Med 26, 2389–2430 (2007).
Tappenden, P. et al. Using whole disease modeling to inform resource allocation decisions: economic evaluation of a clinical guideline for colorectal cancer using a single model. Value Health 16, 542–553 (2013).
Wolbers, M., Koller, M. T., Witteman, J. C. & Steyerberg, E. W. Prognostic models with competing risks: methods and application to coronary risk prediction. Epidemiology (Cambridge, Mass.) 20, 555–561 (2009).
Vanholder, R. et al. Chronic kidney disease as cause of cardiovascular morbidity and mortality. Nephrol Dial Transplant 20, 1048–1056 (2005).
Kissela, B. M. et al. Epidemiology of ischemic stroke in patients with diabetes: the greater Cincinnati/Northern Kentucky Stroke Study. Diabetes Care 28, 355–359 (2005).
Witt, B. J. et al. A community-based study of stroke incidence after myocardial infarction. Ann Intern Med 143, 785–792 (2005).
Elsayed, E. F. et al. Cardiovascular disease and subsequent kidney disease. Arch Intern Med 167, 1130–1136 (2007).
Bang, H. et al. Validation and comparison of a novel screening guideline for kidney disease: KEEPing SCORED. Arch Intern Med 168, 432–435 (2008).
Bang, H. et al. SCreening for Occult REnal Disease (SCORED): a simple prediction model for chronic kidney disease. Arch Intern Med 167, 374–381 (2007).
Kshirsagar, A. V. et al. A simple algorithm to predict incident kidney disease. Arch Intern Med 168, 2466–2473 (2008).
National Collaborating Centre for Chronic Conditions. Chronic kidney disease: national clinical guideline for early identification and management in adults in primary and secondary care. National Institute for Health and Clinical Excellence Clinical Guidance CG 73. (London, 2008).
Hambleton, I. R. et al. All-cause mortality after diabetes-related amputation in Barbados: a prospective case-control study. Diabetes Care 32, 306–307 (2009).
Resnick, H. E. et al. Relation of lower-extremity amputation to all-cause and cardiovascular disease mortality in American Indians: the Strong Heart Study. Diabetes Care 27, 1286–1293 (2004).
Chang, R. E., Lin, S. P. & Aron, D. C. A pay-for-performance program in Taiwan improved care for some diabetes patients, but doctors may have excluded sicker ones. Health Aff (Millwood) 31, 93–102 (2012).
Chen, T. T., Chung, K. P., Lin, I. C. & Lai, M. S. The unintended consequence of diabetes mellitus pay-for-performance (P4P) program in Taiwan: are patients with more comorbidities or more severe conditions likely to be excluded from the P4P program? Health Serv Res 46, 47–60 (2011).
Tan, E. C., Pwu, R. F., Chen, D. R. & Yang, M. C. Is a diabetes pay-for-performance program cost-effective under the National Health Insurance in Taiwan? Qual Life Res 23, 687–696 (2014).
Chang, T.-J. et al. Accountability, utilization and providers for diabetes management in Taiwan, 2000–2009: An analysis of the National Health Insurance database. Taiwan Yi Xue Hui Za Zhi 111, 605–616 (2012).
Cheng, C. L., Kao, Y. H., Lin, S. J., Lee, C. H. & Lai, M. L. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf 20, 236–242 (2011).
Chang, Y. T., Wu, J. L., Hsu, C. C., Wang, J. D. & Sung, J. M. Diabetes and end-stage renal disease synergistically contribute to increased incidence of cardiovascular events: a nationwide follow-up study during 1998-2009. Diabetes Care 37, 277–285 (2014).
Acknowledgements
We would like to thank Ms Shuang Zhu and Mr Wei-Che Chen for their technical supports in assisting data management and analysis and Dr Simon Page, Diabetic and Endocrinology Consultant at Nottingham University for reviewing and commenting on this manuscript.
Author information
Authors and Affiliations
Contributions
L.-C.C. and L.-J.C. involved in the study design, had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. The research progress was managed by L.-J.C., C.H.L., J.H.C. and they also involved in the data cleaning, management and analysis that overseen by H.L., M.Y.L. and S.J.H. involved in defining outcome measures and interpreting study results.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Cheng, LJ., Chen, JH., Lin, MY. et al. A competing risk analysis of sequential complication development in Asian type 2 diabetes mellitus patients. Sci Rep 5, 15687 (2015). https://doi.org/10.1038/srep15687
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep15687
This article is cited by
-
Nomogram for prediction of severe community-acquired pneumonia development in diabetic patients: a multicenter study
BMC Pulmonary Medicine (2022)
-
Factors associated with influenza vaccine coverage among patients with diabetes: Korea National Health and Nutrition Examination Survey 2016–2018
International Journal of Diabetes in Developing Countries (2022)
-
Temporal trajectories of accompanying comorbidities in patients with type 2 diabetes: a Korean nationwide observational study
Scientific Reports (2020)
-
Predictors of vascular complications among type 2 diabetes mellitus patients at University of Gondar Referral Hospital: a retrospective follow-up study
BMC Endocrine Disorders (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.