Abstract
The prevalence and the distribution characteristics of corneal astigmatism (CA) and anterior segment biometry before surgery in Chinese congenital cataract (CC) patients are not completely understood. This study involved 400 CC patients from the Zhongshan Ophthalmic Center enrolled from February 2011 to August 2015. Data on CA, keratometry, central corneal thickness (CCT) and anterior chamber depth (ACD) were measured by the Pentacam Scheimpflug System. The mean age of patients was 54.27 months, and the ratio of boys to girls was 1.53:1. The mean CA was 2.03 diopters (D), and 39.25% of subjects had CA values ≥2 D. The most frequent (71.8%) diagnosis was with-the-rule astigmatism. Oblique astigmatism was present in 16.2% of cases, and 12% of cases had against-the-rule astigmatism. The mean keratometry measurement of cataractous eyes in bilateral patients was significantly larger than that in unilateral patients. Girls had a larger mean keratometry but a thinner CCT than did boys. The CA, CCT, and ACD of cataractous eyes were significantly larger than those of non-cataractous eyes in unilateral patients. The CA, mean keratometry, CCT, and ACD in CC patients varied with age, gender, and laterality. Fully understanding these characteristics may help inform guidelines and treatment decisions in CC patients.
Similar content being viewed by others
Introduction
Congenital cataract (CC) is a primary cause of childhood blindness, which has become treatable in the past decade1,2. It is also one of the primary diseases affecting eye development, with the underlying mechanism involving defocus3,4,5,6 and form deprivation7,8. Several publications, including our previous studies, have reported that the development of axial length in pediatric patients with cataractous eyes is significantly different from that in healthy children9. However, reports on the prevalence and distribution characteristics of corneal astigmatism (CA) and anterior segment biometry in CC patients remain rare. Research on the developmental status of anterior segment biometry will help us fully understand the effect of CC on eye development beyond axial length, which will greatly improve the guidelines for CC treatment. Furthermore, keratometry and anterior chamber depth (ACD) are the most important indices in the accurate calculation of the required intraocular lens (IOL) power before surgery, whereas the variability in central corneal thickness (CCT) may affect the intraocular pressure (IOP) measurement in CC patients during the management of pediatric glaucoma10. The present study was designed to explore the prevalence of CA and the distribution of keratometry, CCT and ACD before surgery in Chinese CC patients and to compare data from the unilateral cataractous eye with those from the corresponding non-cataractous eye. Data on the developmental status of CA and anterior segment biometry in CC patients are of clinical significance to the guidelines for CC treatment, IOL power calculation, and IOP measurement.
Results
Four hundred of the 476 (84.03%) CC patients with qualified measurements in both eyes were included. Of these eligible patients, 34% (136/400) presented with a unilateral cataract, and the remaining 66% (264/400) had bilateral involvements. The mean age was 54.27 ± 42.75 months, and the ratio of boys to girls was 1.53:1 (242:158).
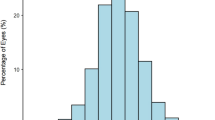
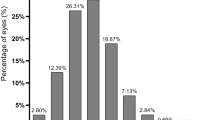
The CA values of CC patients largely (78.5%, 314/400) fell between 0.5 and 3 diopters (D), and the overall distribution of CA is shown in Fig. 1. The mean value of CA was 2.03 ± 1.46 D; 79% (316/400) of subjects had values of ≥1 D, and 39.25% (157/400) had values of ≥2 D. The most frequent (71.8%) diagnosis was with-the-rule astigmatism (WTR astigmatism) (steepest meridian at 180 ± 30 degrees). Oblique astigmatism (steepest meridian between 120 and 150 degrees or between 30 and 60 degrees) was present in 16.2% of cases, and 12% of cases had against-the-rule astigmatism (ATR astigmatism) (steepest meridian at 90 ± 30 degrees) (Fig. 2). Further description of the CA in patients by age group, gender and laterality is provided in Table 1.
Tables 2, 3, 4 show the distribution of mean keratometry, CCT, and ACD, respectively, by age group, gender and cataract laterality. The mean keratometry measurements of the cataractous eye in bilateral patients were significantly larger than those in unilateral involvements. Girls had a larger mean keratometry but a thinner CCT than did boys. No significant differences in ACD were found in CC patients by gender or laterality.
Figure 3 shows scatterplots of mean keratometry versus age. A linear decline in mean keratometry with age was revealed in patients less than 6 months old, but this tendency was absent in older patients. Scatterplots of mean keratometry, CA, CCT, and ACD in relation to age are shown in Fig. 4. Panels A (mean keratometry versus age), B (CA versus age) and C (CCT versus age) show little relationship between their respective variables and age. Panel D illustrates a logarithmic relationship between ACD and age.
Panel (A) (mean keratometry versus age), Panel (B) (CA versus age) and Panel (C) (CCT versus age) show little relationship between the respective variables and age. Panel (D) illustrates a logarithmic relationship between ACD and age. D: diopters; CA: anterior corneal astigmatism; CCT: central corneal thickness; ACD: anterior chamber depth.
Table 5 shows the differences in mean keratometry, CA, CCT, and ACD between the unilateral cataractous eye and the clear counterpart eye. Larger CA, CCT, and ACD values were found for the affected eye.
The multiple linear regression equation of CA and mean keratometry, CCT, and ACD was shown as follow:

Notes: R2(adjusted) = 0.036, F = 5.97, P = 0.001 (P(X1) = 0.75, P(X2) = 0.18, P(X3) = 0.00); Y: CA, X1: mean keratometry, X2: CCT, X3: ACD.
Discussion
Knowledge of the prevalence of preoperative CA and the associated characteristics of anterior segmental biometry can greatly enhance the guidelines for CC treatment and prognosis. However, few studies have used a large cohort of CC patients, perhaps due to the low incidence of CC, a lack of awareness of the importance of such data, the challenge of the necessary examination, and a lack of proper equipment. The Pentacam Scheimpflug System used in the present study can provide a 3-dimensional representation of the anterior segment of the eye, including comprehensive parameters, by rotating 180 degrees around the eye and capturing 25 single-slit images in less than 2 seconds11. Because of the merits of noncontact, rapid imaging and high quality, the success rate of examination in this study was relatively high (84.03%). In the present cohort, the mean CA in CC patients was larger than 2 D, and most patients had with-the-rule astigmatism. Girls had a larger mean keratometry but a thinner CCT than did boys, and a positive, linear relationship was found between ACD and age. Furthermore, the CA, CCT, and ACD values of the unilateral cataractous eye were significantly larger than those of the corresponding non-cataractous eye. This study is the first report on the prevalence of CA and the characteristics of the anterior segmental biometry in Chinese CC patients.
Previous studies have found a high rate of postoperative astigmatism in CC patients, although a number of cases reduced spontaneously over time12,13. Research on preoperative CA can be of great benefit in informing the guidelines for astigmatism treatment in CC patients. A previous study14 with a small sample size (62 patients) reported the distribution of CA in CC patients using an autorefract-keratometer. They found that the prevalence of CA ≥2 D in Japanese patients was 65.7%, and the most frequent diagnosis was WTR astigmatism. However, they did not describe the specific relationships between CA and patient demographics. In the present study using a large cohort of CC patients, similar findings regarding the prevalence and type of CA were revealed. Furthermore, we found that the prevalence of CA was unassociated with age, gender, and laterality. These findings demonstrate a markedly higher prevalence of CA (≥1.00 D, 79% in this study, and 89.9% in the study of Japanese patients mentioned above) in pediatric CC patients than in children without cataracts from Taiwan (13.3%)15, Northern Ireland (25–29%)16, and Australia (26.6%)17. Furthermore, the proportion of high astigmatism (≥2 D) in CC patients was higher than that reported for Tohono O’odham children, a native American tribe that has been documented with a high prevalence of astigmatism among preschool- and school-age members18. We also found that the affected eye of unilateral cataract patients had a higher CA than did the unaffected eye in 5 age groups. A higher CA in the eye with CC likely resulted from the abnormal development of the eyeball19. For those CC patients with high preoperative CA, the selection of an appropriate surgical procedure20, appropriate delay of the surgery12, the use of a small vitrectomy system21, and the adjustment of the type or location of the incision according to the CA reading13,20 may contribute to a decrease in the prevalence of postoperative astigmatism. In addition, a less favorable outcome with postoperative amblyopia treatment has also been reported in children with ATR astigmatism than those with WTR astigmatism;22 thus, a detailed explanation of the potential for poor postoperative visual function is needed.
In addition to information on astigmatism, knowledge of the distribution of other anterior segment variations, such as keratometry, CCT and ACD, can improve CC treatment and should be measured before surgery. Previous studies have described the distribution of keratometry in White and African American23, Nepalese24, Serbian25, and Italian children26. Trivedi and colleagues23 investigated keratometry in 299 pediatric eyes with cataracts in America and found that the average value was 45.39 D, with steeper keratometry in girls than in boys. They also found that the corneal curvature of the eye with the cataract was steeper in unilateral cases than in bilateral involvements and that the eye with the cataract had a significantly steeper cornea than did the corresponding eye in monocular cataract patients. However, until now, keratometry in Chinese children with cataracts has been unclear because keratometry varies with ethnicity27. In this study with a large Chinese cohort, we similarly found steeper keratometry in girls than in boys. However, the mean keratometry reading (43.37 D) was smaller than that found in other studies. This result may reflect the specific study population involved and the low proportion of younger children (only 11.5% of children were ≤6 months) in the present study, as infants were found to have a steeper corneal curvature. Similar to a previous finding, we found that newborns have a steeper corneal curvature than do older children; this curvature decreased with age and stabilized after 6 months of age28. This growth pattern of keratometry with age may reflect the compensatory changes in axial length that are required to maintain a constant state of refractive power23. Unfortunately, the anterior segment imaging and analysis system (the Pentacam in this study) does not provide the measurement of axial length. In addition, we found that the mean keratometry measurements of eyes in bilateral CC patients (6–18 years old) were significantly larger than those of the cataractous eye in unilateral involvements and that the keratometry value of the cataractous eye was the same as that of the healthy eye in unilateral patients, the latter of which contradicts previous findings23. In addition to age composition, different ethnicities and measurement techniques (keratometer vs. Pentacam) could account for these discrepancies among studies.
It is necessary to consider the CCT distribution in the management of pediatric glaucoma due to the effect of CCT on IOP measurement10. A small sample size of cataract patients (n = 30) and the multi-racial (≥5 races) composition of a previous study29 limited the scope of investigation of the relationships between CCT and the demographics of CC patients. The results of the present study of a large cohort of CC patients (n = 400) within a single racial group (Chinese) provide an overview of the distribution of CCT in Chinese pediatric CC patients. We found that the CCT of boys was thicker than that of girls, and a thicker CCT was revealed in the cataractous eye of 135 unilateral CC patients when compared with the contralateral healthy eye. Muir et al.29 found a trend of a thicker mean CCT in the cataractous eye than in the eye without a cataract (564 ± 34 μm vs. 552 ± 38 μm), although the difference became smaller after excluding eyes with an abnormal cornea from the cataract group. The CCT is usually thickest immediately after birth and then thins until approximately 3 years old10. Thus, we hypothesize that the thicker CCT in the eyes with a cataract may have resulted from the delayed development and maturation of the cornea.
ACD is a component of the axial length and is an indicator of the development of the anterior segment of the eyeball. In this study, the ACD of the cataractous eye showed a logarithmic relationship with age. This finding confirms that the increase in ACD with age may be a result of the increase in axial length due to the close relationship between ACD and axial length30. We also found that the ACD of the affected eye in unilateral cataract patients was larger than that of the fellow eye. However, this difference was limited to patients aged 2–6 years. Furthermore, both Twelker et al.27 and Trivedi et al.30 noted that girls had a shallower anterior chamber than did boys in both the healthy eye and the cataractous eye. Interestingly, in Chinese CC patients, we also found a smaller ACD in girls than in boys aged 7 months to 2 years, but no differences were observed in the other age groups. It is known that ACD varies with ethnicity27, but the relationship between ACD and gender in different races and whether boys have a deeper anterior chamber at all ages remain unknown. In addition, results of the multiple linear regression (eq. 1) showed that patients with short ACD were more likely to suffer larger CA than those with deeper anterior chamber. Therefore, more attention about the CA should be paid to those patients with shallow anterior chamber relatively easily found by a slit lamp examination.
The results of our study should be interpreted with caution. First, we only focused on the development of the anterior segmental biometry in eyes of Chinese CC patients and did not include measurement of axial length, which is another important indicator of eye development. Axial length will be included in our next study to provide a more comprehensive assessment of eye development. Second, a lack of fixation while measuring the anterior segmental parameters under chloral hydrate sedation in some patients may have introduced some error in our biometry readings31. However, massaging the eyeball to the primary position and referring to the quality index of the Pentacam image helped us to obtain reliable measurements in the absence of fixation. Despite these limitations, the results of this study describe the prevalence of CA and the overall distribution of anterior segmental biometry before surgery in a large cohort of Chinese CC patients. In conclusion, the CA of cataractous eyes in CC patients was significantly larger than that of eyes with a clear lens, and the most frequent type of astigmatism was WTR astigmatism. The mean keratometry, CA, CCT, and ACD in CC patients varied with age, gender, and laterality. The anterior segment biometry data of Chinese pediatric patients provided in the present study are of clinical significance to the guidelines for CC treatment, IOL power calculation, and IOP measurement.
Patients and Methods
Subjects
From February 2011 to August 2015, patients ≤18 years old with CC were recruited and enrolled in this study from the Zhongshan Ophthalmic Center (ZOC), one of the largest eye facilities in China and located in Guangzhou city in Southern China. Participants were eligible if the child was diagnosed with CC before surgery and lacked other ocular abnormalities, such as corneal diseases, lens luxation, glaucoma, retinal diseases, nystagmus, and nanophthalmos. The analyzed cataractous eyes were composed of the affected eye of unilateral patients and a randomly selected eye of bilateral patients. This study was approved by the Human Research Ethics Committee of the ZOC, Sun Yat-sen University. All procedures adhered to the tenets of the Declaration of Helsinki, and written informed consent was obtained from at least one parent of each patient.
Anterior segment examination and parameters
Anterior segment parameters, including CA, mean keratometry, CCT and ACD, of CC patients were measured under an undilated pupil before surgery. These measurements were obtained using a 3-dimensional anterior segment imaging and analysis system (Pentacam HR, Oculus Inc., Wetzlar, Germany), which is a commercially available camera based on the Scheimpflug principle11. It provides a 3-dimensional representation of the anterior segment of the eye after rotating around the eye from 0 to 180 degrees and capturing 25 single-slit images in less than 2 seconds. All patients were tested by one experienced examiner (ZLL), and those patients who were unable to actively cooperate were sedated with 10% chloral hydrate (0.8 ml/kg, oral or rectal administration)32. The mean of 3 measurements that met the quality standards was calculated for each parameter.
CA, mean keratometry, CCT and ACD were the main parameters measured from the anterior segment of the eye and were defined in this study as follows. The difference between the steep keratometry and flap keratometry of the front surface of the cornea was defined as the CA, and the mean value of the steep keratometry and flap keratometry was defined as the mean keratometry. Furthermore, CCT was measured from the central anterior corneal epithelium to the central posterior corneal endothelium. The ACD, which is equivalent to the “ACD-lens” described in our previous publication33, was defined as the distance from the corneal endothelium to the lens epithelium.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS ver. 19.0, Chicago, IL, USA). Absolute frequency (n) and relative frequency (%) were used for the analysis of qualitative variables, and mean and standard deviation (mean ± SD) were used for the analysis of quantitative variables. The Kolmogorov-Smirnov test was used to evaluate the normality of the distribution for all variables. The t-test for independent samples was used to analyze the variables of cataract eyes, and the paired t-test was used to evaluate the differences between the affected eye and the fellow eye in unilateral patients. The relationships between the biometry data and age were analyzed based on Pearson correlation coefficients and regression analysis. The multiple linear regression was used to analyze the relationships between CA and mean keratometry, CCT, and ACD. A P-value < 0.05 was considered statistically significant.
Additional Information
How to cite this article: Lin, D. et al. Prevalence of Corneal Astigmatism and Anterior Segmental Biometry Characteristics Before Surgery in Chinese Congenital Cataract Patients. Sci. Rep. 6, 22092; doi: 10.1038/srep22092 (2016).
References
Pi, L. H. et al. Prevalence of eye diseases and causes of visual impairment in school-aged children in Western China. J. Epidemiol. 22, 37–44 (2012).
Lim, Z., Rubab, S., Chan, Y. H. & Levin, A. V. Pediatric cataract: the Toronto experience-etiology. Am. J. Ophthalmol. 149, 887–892 (2010).
Zhu, X., Park, T. W., Winawer, J. & Wallman, J. In a matter of minutes, the eye can know which way to grow. Invest. Ophthalmol. Vis. Sci. 46, 2238–2241 (2005).
Graham, B. & Judge, S. J. The effects of spectacle wear in infancy on eye growth and refractive error in the marmoset (Callithrix jacchus). Vision Res. 39, 189–206 (1999).
Wallman, J. et al. Moving the retina: choroidal modulation of refractive state. Vision Res. 35, 37–50 (1995).
Read, S. A., Collins, M. J. & Sander, B. P. Human optical axial length and defocus. Invest. Ophthalmol. Vis. Sci. 51, 6262–6269 (2010).
Bremond-Gignac, D., Copin, H., Lapillonne, A. & Milazzo, S. Visual development in infants: physiological and pathological mechanisms. Curr. Opin. Ophthalmol. 22 Suppl, S1–8 (2011).
Lambert, S. R. et al. The infant aphakia treatment study: design and clinical measures at enrollment. Arch. Ophthalmol. 128, 21–27 (2010).
Zhan, J., Lin, H., Zhang, X., Chen, W. & Liu, Y. Significance of axial length monitoring in children with congenital cataract and update of measurement methods. Eye Sci. 28, 95–102 (2013).
Xiao, W., Liang, X. F. & Sun, J. J. Changes of corneal central thickness of aphakia following congenital cataract surgery under the first six months of life. Int. J. Ophthalmol. 4, 78–80 (2011).
Kim, J. S., Chung, S. H. & Joo, C. K. Clinical application of a Scheimpflug system for lens density measurements in phacoemulsification. J. Cataract Refract. Surg. 35, 1204–1209 (2009).
Bar-Sela, S., Glovinsky, Y., Wygnanski-Jaffe, T. & Spierer, A. The relationship between patient age and astigmatism magnitude after congenital cataract surgery. Eur. J. Ophthalmol. 19, 376–379 (2009).
Bar-Sela, S. M. & Spierer, A. Astigmatism outcomes of scleral tunnel and clear corneal incisions for congenital cataract surgery. Eye (Lond.) 20, 1044–1048 (2006).
Watanabe, T., Matsuki, N., Yaginuma, S. & Nagamoto, T. [Corneal astigmatism in children with congenital cataract]. Nippon Ganka Gakkai Zasshi 118, 98–103 (2014).
Lai, Y. H., Hsu, H. T., Wang, H. Z., Chang, C. H. & Chang, S. J. Astigmatism in preschool children in Taiwan. J. AAPOS 14, 150–154 (2010).
O’Donoghue, L. et al. Refractive and corneal astigmatism in white school children in northern ireland. Invest. Ophthalmol. Vis. Sci. 52, 4048–4053 (2011).
Huynh, S. C., Kifley, A., Rose, K. A., Morgan, I. G. & Mitchell, P. Astigmatism in 12-year-old Australian children: comparisons with a 6-year-old population. Invest. Ophthalmol. Vis. Sci. 48, 73–82 (2007).
Harvey, E. M. et al. Prevalence of corneal astigmatism in Tohono O’odham Native American children 6 months to 8 years of age. Invest. Ophthalmol. Vis. Sci. 52, 4350–4355 (2011).
Bouzas, A. G. Anterior polar congenital cataract and corneal astigmatism. J. Pediatr. Ophthalmol. Strabismus 29, 210–212 (1992).
Ma, L. W., Xuan, D., Li, X. Y. & Zhang, J. S. Corneal astigmatism correction with scleral flaps in trans-scleral suture-fixed posterior chamber lens implantation: a preliminary clinical observation. Int. J. Ophthalmol. 4, 502–507 (2011).
Chee, K. Y. & Lam, G. C. Management of congenital cataract in children younger than 1 year using a 25-gauge vitrectomy system. J. Cataract Refract. Surg. 35, 720–724 (2009).
Somer, D., Budak, K., Demirci, S. & Duman, S. Against-the-rule (ATR) astigmatism as a predicting factor for the outcome of amblyopia treatment. Am. J. Ophthalmol. 133, 741–745 (2002).
Trivedi, R. H. & Wilson, M. E. Keratometry in pediatric eyes with cataract. Arch. Ophthalmol. 126, 38–42 (2008).
Shrestha, U. D. & Shrestha, M. K. Keratometry in eyes with bilateral pediatric cataract at tertiary eye care center in Nepal: a preliminary report. Nepal Med. Coll. J. 11, 203–204 (2009).
Marjanovic, I., Stefanovic, I. & Vlajkovic, G. [Keratometric measurements of cornea in first three years of life in children with congenital cataract]. Srp. Arh. Celok. Lek. 136, 471–475 (2008).
Capozzi, P., Morini, C., Piga, S., Cuttini, M. & Vadala, P. Corneal curvature and axial length values in children with congenital/infantile cataract in the first 42 months of life. Invest. Ophthalmol. Vis. Sci. 49, 4774–4778 (2008).
Twelker, J. D. et al. Children’s ocular components and age, gender, and ethnicity. Optom. Vis. Sci. 86, 918–935 (2009).
Gordon, R. A. & Donzis, P. B. Refractive development of the human eye. Arch. Ophthalmol. 103, 785–789 (1985).
Muir, K. W., Duncan, L., Enyedi, L. B., Wallace, D. K. & Freedman, S. F. Central corneal thickness: congenital cataracts and aphakia. Am. J. Ophthalmol. 144, 502–506 (2007).
Trivedi, R. H. & Wilson, M. E. Biometry data from caucasian and african-american cataractous pediatric eyes. Invest. Ophthalmol. Vis. Sci. 48, 4671–4678 (2007).
Mittelviefhaus, H. & Gentner, C. [Errors in keratometry for intraocular lens implantation in infants]. Ophthalmologe 97, 186–188 (2000).
Chen, J., Lin, Z. & Lin, H. Progress of application of sedation technique in pediatric ocular examination. Eye Sci. 29, 186–192 (2014).
Lin, H. et al. Anterior segment variations after posterior chamber phakic intraocular lens implantation in myopic eyes. J. Cataract Refract. Surg. 39, 730–738 (2013).
Acknowledgements
This clinical study was supported by the Ministry of Science and Technology of China Grants (973 program, 2015CB964600), the Key Projects for Hospital Clinical Disciplines of the Ministry of Health of China in 2010–2012 (Project No. 175 in Document 439 of the Planning and Finance Secretary of the Ministry of Health), the Pearl River Science and Technology New Star (Grant No. 2014J2200060) Project of Guangzhou City, the Guangdong Provincial Natural Science Foundation for Distinguished Young Scholars of China (Grant No. 2014A030306030), Youth Science and Technology Innovation Talents Funds in the Special Support Plan for High Level Talents in Guangdong Province (Grant No. 2014TQ01R573), the Intensive Cultivation Projects (2015ykzd11) for Young Teaching Staff of Sun Yat-sen University from the Fundamental Research Funds for the Central Universities, the National Natural Science Foundation of China (81300750), the Fundamental Research Funds of State Key Laboratory of Ophthalmology (Grant No. 2015QN01) and Key Research Plan for National Natural Science Foundation for Cultivation Project of China (No. 91546101). The sponsors of the study played no role in the study protocol design, data collection, data analysis, data interpretation, manuscript preparation, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
H.T.L., D.R.L., J.J.C., Z.Z.L. and W.R.C. were involved in the study’s conception, design, and funding; H.T.L., D.R.L., J.J.C., Z.Z.L., W.R.C. and Y.Z.L. conducted the study; H.T.L., D.R.L., J.J.C., Z.Z.L., Z.L.L., X.Y.L., X.H.W., E.P.L., H.C. and L.Z. collected the data; H.T.L., D.R.L., J.J.C., J.C.L. and W.R.C. analyzed the data; H.T.L., D.R.L., J.J.C. and Z.Z.L. wrote the manuscript; H.T.L., D.R.L., J.J.C., L.X.L., Z.L.L., X.H.W., E.P.L., H.C., W.R.C. and Y.Z.L. reviewed the manuscript; and all authors gave final approval of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Lin, D., Chen, J., Liu, Z. et al. Prevalence of Corneal Astigmatism and Anterior Segmental Biometry Characteristics Before Surgery in Chinese Congenital Cataract Patients. Sci Rep 6, 22092 (2016). https://doi.org/10.1038/srep22092
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep22092
This article is cited by
-
Preoperative Characteristics of Ocular Biometry in Children with Unilateral Congenital Cataracts
Phenomics (2022)
-
Analysis of corneal astigmatism and aberration in chinese congenital cataract and developmental cataract patients before cataract surgery
BMC Ophthalmology (2021)
-
Clinical outcomes of Transepithelial photorefractive keratectomy to treat low to moderate myopic astigmatism
BMC Ophthalmology (2018)
-
Height, weight and body mass index of children with congenital cataracts before surgical treatment
BMC Ophthalmology (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.