Abstract
Previously, we demonstrated that renal hemodynamic responses to nitric oxide (NO) inhibition were attenuated in aged, hypertensive sheep born with a solitary functioning kidney (SFK). NO is an important regulator of renal function, particularly, in the postnatal period. We hypothesized that the onset of renal dysfunction and hypertension in individuals with a SFK is associated with NO deficiency early in life. In this study, renal and cardiovascular responses to L-NAME infusion (Nw-nitro-L-arginine methyl ester) were examined in 6-month old lambs born with a SFK, induced by fetal unilateral nephrectomy (uni-x). Renal responses to L-NAME were attenuated in uni-x sheep with the fall in glomerular filtration rate (GFR) and urinary sodium excretion (UNaV) being less in the uni-x compared to sham lambs (%ΔGFR; −41 ± 3 vs −54 ± 4: P = 0.03, %ΔUNaV; −48 ± 5 vs −76 ± 3, P = 0.0008). 24 hour-basal urinary nitrate and nitrite (NOx) excretion was less in the uni-x animals compared to the sham (NOx excretion μM/min/kg; sham: 57 ± 7; uni-x: 38 ± 4, P = 0.02). L-NAME treatment reduced urinary NOx to undetectable levels in both groups. A reduction in NO bioavailability in early life may contribute to the initiation of glomerular and tubular dysfunction that promotes development and progression of hypertension in offspring with a congenital nephron deficit, including those with a SFK.
Similar content being viewed by others
Introduction
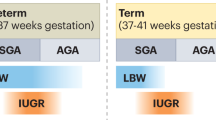
In children born with only one kidney (congenital solitary functioning kidney; SFK) or those who lose a kidney early in life (acquired SFK), the onset of hypertension and renal disease occur early in life1,2 and ~20–40% of these children develop end-stage renal disease (ESRD) by the age of 303. In contrast, in adults who donate a kidney, the risk of developing chronic kidney disease (CKD) and hypertension are relatively low4 indicating that the loss of renal mass early in life may carry a greater risk for future onset of diseases but the mechanisms remain unclear. A relationship between small kidney length, renal dysfunction and arterial pressure in children with a SFK has been identified1. Additionally, infants born of low birth weight and those born premature, have smaller kidneys and in these children a higher prevalence of cardiovascular and CKD has also been reported5. Since a small kidney size correlates with low nephron number6 and given the importance of kidney function in regulation of arterial pressure, it is likely that alterations in factors regulating renal physiology early in life when the kidneys are undergoing functional maturation, underpin the development of hypertension in these children.
Nitric oxide is an important regulator of renal hemodynamics and tubular function7 and NO produced within the kidney contributes to the regulation of sodium excretion and thus, maintenance of vascular volume and arterial pressure in the adult8. NO also plays a significant role in the normal maturation of renal function early in the postnatal period. Renal blood flow (RBF) and GFR are low in the fetus but increase rapidly after birth4. In newborn lambs, the rise in RBF during the postnatal period occurs with a concomitant increase in nitric oxide (NO) production9. Moreover expression of endothelial NO synthase (eNOS) increases progressively in the pre-glomerular resistance vasculature of the newborn compared to the adult suggesting a critical role for NO in modulating renal hemodynamics in the postnatal period10. A reduction in bioavailability/production of NO has been observed in experimental models of nephron deficiency11,12 and in patients with ESRD and hypertension13. Additionally it has been demonstrated that increasing NO bioavailability by L-Arginine or Citrulline supplementation normalizes blood pressure, improves renal function and prevents proteinuria in developmental programming14 and genetic models15 of hypertension. This suggests that a deficiency of NO is present in both genetic and acquired forms of hypertension. Therefore, a strong case can be made for NO deficiency in the early life as a primary stimulus for the development and/or progression of hypertension and renal disease in adulthood16,4,17.
Since majority (~90%) of children with SFK do not have extra-renal abnormalities18, we established an ovine model of congenital SFK to better understand the effects of a reduction of renal mass on regulation of renal and cardiovascular function. In our model, a congenital SFK is induced by performing unilateral nephrectomy in the sheep fetus (uni-x) at 100 days of gestation (term = 150 days) and this results in ~30% reduction in total nephron number as a result of some compensatory nephrogenesis in the remaining kidney of the sheep fetus19. The sheep begins formation of the permanent kidney at day 27 of gestation and completes nephrogenesis at day 130 of gestation, 3 weeks prior to birth20, making it almost identical to the human which also completes nephrogenesis 3 weeks prior to birth20. Similar to our observations in sheep, compensatory nephrogenesis has also been reported in children with SFK21. We have demonstrated that both male and female uni-x sheep have early onset of disease with increases in arterial pressure and reductions in glomerular filtration rate (GFR) occurring by 6 months of age22,23. Additionally, the normal age-related decline in renal function and elevation in blood pressure is exacerbated by 4–5 years of age24,25. Our detailed characterization of renal function in aged sheep with SFK demonstrated that renal hemodynamic responses to inhibition of nitric oxide synthase (NOS) were attenuated26 indicating a nitric oxide (NO) deficiency. However, a limitation of the study in aged sheep was that the hypertension was longstanding (~4 years) and therefore it was not possible to determine if the NO deficiency was a cause or a consequence of the hypertension. Studies in rodents have also implicated reduced NO bioavailability in the developmental origins of hypertension, though again these studies were conducted once hypertension was well established27.
In the present study we examined if a deficiency of NO was present in young sheep with a congenital SFK (induced by fetal uni-x). Our studies in the young sheep are important because very little is known about the mechanisms driving the early onset of disease in children with SFK. We hypothesized that a renal NO deficiency is present early in life in lambs with a congenital SFK (uni-x) such that the contribution of NO to basal renal hemodynamics and function would be reduced. Specifically in the present study cardiovascular and renal responses to in vivo NOS inhibition via the administration Nw-nitro-L-arginine methyl ester (L-NAME) in conscious female lambs with a SFK or with intact kidneys was examined at 6 months of age. Additionally we examined levels of urinary nitrate as a marker of NO deficiency22.
The findings of the current study are novel because for the first time, we have identified a change in a factor regulating renal hemodynamic very early in life that provides an early biomarker of disease. The finding that our sheep with a congenital SFK have deficiencies in NO from as early as 6 months of age, a time when they are only very mildly hypertensive suggests this mechanism contributes to the overt and progressive elevations in blood pressure that occur with aging25. Having identified a deficiency of NO early in the disease phase, future studies can examine whether increasing NO bioavailability from this stage can be a viable treatment option for slowing the progression of disease in those with congenital SFK.
Results
Body weights
All lambs were born at 150 ± 1 days of gestation. Body weight at birth and at 6 months of age, was not different between the sham and uni-x groups (birth weight (kg): sham: 3.5 ± 0.3, uni-x: 4.2 ± 0.2; 6 months (kg): sham: 24.5 ± 1.7, uni-x: 25.5 ± 0.8).
Metabolic cage-balance studies
Food intake, water intake, urine output and urinary sodium excretion (UNaV) during the 5 days the animals were housed in metabolic cages are shown in Fig. 1. All variables were corrected for body weight. Food intake increased in both groups to a similar extent across time (Ptime = 0.002; Pgroup x time = 0.4, Fig. 1a). Both groups had similar 24-h water intake (Fig. 1b) and urine output (Fig. 1c) over the 5-day period. In the sham lambs UNaV was similar across each day of the measurement period. However, in the uni-x lambs UNaV oscillated, increasing and decreasing across the 5-day period and this was significantly different to the response in the sham group (Pgroup x time = 0.04, Fig. 1d). However, average UNaV across the 5-day period was not significantly different (average UNaV, mmol/min/bw; sham: 7.6 ± 0.1, uni-x: 7.0 ± 0.5, P = 0.2).
Twenty-four hour (a) food intake, (b) water intake and (c) urine output and urinary sodium excretion (UNaV) measured over a period of 5 days at 6 months of age in sheep that underwent either uninephrectomy (uni-x; n = 9; solid circles) or sham (n = 7; open circles) surgery on 100 days of gestation. P-values are from a repeated measures ANOVA with factors group (sham, uni-x), time and their interaction. *P < 0.05 Bonferroni post- hoc as compared to the sham group. Variables are expressed per bodyweight (bw). Values are presented as mean ± sem.
Basal 72-h arterial pressure and heart rate
Mean arterial pressure (MAP) and heart rate (HR), continuously recorded in un-anesthetized animals over 72 hours, are reported as averages of the day (5 am–5 pm) and night period (5 pm–5 am) (Fig. 2). The diurnal rhythm was similar in both groups for MAP (Ptime < 0.0001, Pgroup x time = 0.1, Fig. 2a) and HR (Ptime < 0.0001, Pgroup x time = 0.1, Fig. 2b). Uni-x animals had a significantly higher MAP compared to the sham group (average 72-h: MAP (mmHg); sham: 80 ± 2, uni-x: 86 ± 1, P = 0.009, Fig. 2a). but HR was similar between the groups (average 72-h: Heart rate (beats/min); sham: 91.7 ± 2.2, uni-x: 91.1 ± 1.8, Fig. 2b).
Continuous three day measurement of (a) mean arterial pressure (MAP) and (b) heart rate (HR) presented as day and night averages at 6 months of age in un-anesthetised sheep that underwent either uninephrectomy (uni-x; n = 9; black bars) or sham (n = 7; open bars) surgery at 100 days of gestation. P-values are from a repeated measures ANOVA with factors group (sham, uni-x), time and their interaction. Values are presented as mean ± sem.
Basal cardiovascular and renal response to vehicle infusion
Cardiovascular and renal function were also assessed in response to a 3 hour period of vehicle infusion as a time control (Fig. 3). MAP was significantly higher in uni-x animals compared to sham animals (Pgroup = 0.0008, Fig. 3a) and heart rate was not different between the groups (Fig. 3b). No effect of time was observed on either of these variables.
Cardiovascular and renal responses to vehicle infusion.
(a) Mean arterial pressure (MAP), (b) heart rate (HR), (c) renal blood flow (RBF), (d) renal vascular resistance (RVR), (e) glomerular filtration rate (GFR), (f) filtration fraction, (g) urine flow rate (UFR), (h) urinary sodium excretion (UNaV) measured over 3 hours of vehicle infusion in sheep aged 6 months that underwent fetal uninephrectomy (uni-x; n = 9; closed symbols-broken lines) or sham surgery (n = 7; open symbols-solid lines). P-values are from a repeated measures ANOVA with factors group (sham, uni-x) and time (period of vehicle infusion) and their interaction (group x time). Renal variables are expressed per bodyweight (bw). All values are presented as mean ± sem.
RBF, renal vascular resistance (RVR), GFR and filtration fraction did not vary with time in either treatment group (Fig. 3c–f). Uni-x animals had a significantly lower RBF (Pgroup < 0.0001, Fig. 3c) and GFR (Pgroup < 0.0001, Fig. 3e) compared to the sham group across the entire 3 hour period. RVR was greater in uni-x animals compared to the sham group across the entire 3 hour period (Pgroup < 0.0001, Fig. 3d) but filtration fraction was similar between the groups (Fig. 3f). Urine flow rate (UFR) was similar between the groups across the 3 hour period of measurement and was not affected by time (Fig. 3g). Uni-x animals had a lower urinary excretion of sodium (UNaV) compared to the sham (Pgroup = 0.02, Fig. 3h) but time had no effect on UNaV in either treatment group.
Cardiovascular and function in response to L-NAME infusion
Prior to administration of L-NAME cardiovascular and renal function was assessed over a period of 1 hour to establish a baseline on that day (Fig. 4). During the hour baseline period the variables measured were similar to those obtained during the assessment of renal function during vehicle infusion (Fig. 3).
Cardiovascular and renal responses to L-NAME infusion.
(a) Mean arterial pressure (MAP), (b) heart rate (HR), (c) renal blood flow (RBF), (d) renal vascular resistance (RVR), (e) glomerular filtration rate (GFR), (f) filtration fraction, (g) urine flow rate (UFR), (h) urinary sodium excretion (UNaV) measured over 1 hour (basal) and in response to 120 minutes of infusion of L-NAME in sheep aged 6 months that underwent fetal uninephrectomy (uni-x; n = 9; closed symbols-broken lines) or sham surgery (n = 7; open symbols-solid lines). P-values are from a repeated measures ANOVA with factors group (sham, uni-x) and treatment (before and during L-NAME) and their interaction (group x treat). Renal variables are expressed per bodyweight (bw). All values are presented as mean ± sem.
The responses to L-NAME infusion were similar over the 2 hours of administration (Fig. 4), therefore this data was averaged to allow determination of the average response to L-NAME across the infusion period to compare the percent response in each group. In response to L-NAME, MAP increased compared to baseline in both groups (both P < 0.0001, Fig. 4a). The percentage change in MAP in response to L-NAME from baseline was similar between the groups (%Δ MAP; sham: 17 ± 1, uni-x: 16 ± 2). HR decreased in response to L-NAME in both groups compared to baseline (both P < 0.0001, Fig. 4b). The percentage change in HR from baseline in response to L-NAME was not different between the groups (%Δ HR; sham: −23 ± 3, uni-x: −18 ± 1).
In response to L-NAME, GFR and RBF decreased compared to baseline in both sham and uni-x groups (both P < 0.0001, Fig. 4c,e). However, the fall in GFR (%Δ GFR; sham: −54 ± 4, uni-x: −41 ± 3, P = 0.03) and RBF (%Δ RBF; sham: −73 ± 3, uni-x: −47 ± 3, P < 0.0001) were less in the uni-x compared to sham lambs. In response to L-NAME, RVR increased in both groups compared to baseline (both P < 0.001, Fig. 4c). However, the percent change in RVR from baseline in response to L-NAME was significantly less in the uni-x group relative to the sham (%Δ RVR; sham: 349 ± 44, uni-x: 125 ± 12, P < 0.0001). As a result of the proportionally larger fall in RBF as compared to GFR in the sham group, filtration fraction was observed to increase in response to L-NAME (P < 0.0001, Fig. 4f). However, as GFR and RBF fell by a similar extent in response to L-NAME in the uni-x lambs, filtration fraction was not different to baseline (Fig. 4f).
UFR decreased in response to L-NAME compared to baseline in both groups (both P < 0.001) but the percentage change was not different between the groups (%Δ UFR; sham: −50 ± 7, uni-x: −42 ± 5, Fig. 4g). UNaV declined in response to L-NAME compared to baseline in both groups (sham, P < 0.0001, uni-x, P < 0.01, Fig. 4h). Moreover, the percent change in UNaV in response to L-NAME from baseline was less in the uni-x compared to sham lambs (%ΔUNaV; sham: −76 ± 3, uni-x: −48 ± 5, P = 0.0008).
Urinary NOx
Basal 24-h urinary nitrate and nitrite (total NOx) excretion was significantly less in the uni-x compared to the sham animals (total NOx excretion; μM/min/bw; sham: 57 ± 7; uni-x: 38 ± 4, P = 0.02). Similarly during the hour baseline period on the day of the L-NAME infusion NOx excretion was lower in the uni-x as compared to the sham lambs (NOx excretion; μM/min/bw; sham: 72 ± 8; uni-x: 54 ± 3, P = 0.04). NOx levels could not be detected in urine at 120 mins of L-NAME administration (below the detection limit of the assay kit).
Discussion
The major finding of this study was that NO made a reduced contribution to the modulation of renal hemodynamics and tubular function in young sheep born with a single kidney. This is the first study to demonstrate this in a large animal model of congenital solitary functioning kidney. Inhibition of NO synthases caused RBF and GFR to decrease in both the uni-x and sham lambs at 6 months of age, but the reduction was markedly less in the uni-x sheep. Furthermore, whilst filtration fraction almost doubled in the normotensive sham group, filtration fraction was unaltered in the uni-x animals. Additionally, total urinary NOx (nitrate and nitrite) excretion was significantly less in uni-x lambs indicative of reduced renal NO production. This data demonstrates NO deficiency is present in juvenile sheep subject to the removal of a kidney as a fetus and that the NO deficit has impacted control of net glomerular filtration pressure as evidenced by the lack of modulation of filtration fraction by L-NAME in the uni-x lambs. Thus, a reduction in NO bioavailability early in life may contribute to the chronic kidney disease and hypertension observed in children with a SFK.
Previously, in aged sheep (5 years old) we identified a NO deficit in the kidney of uni-x sheep26. A major limitation of that study was that the sheep had been hypertensive for 4 years at the time of study at 5 years of age. Thus, we could not determine if the NO deficiency was a cause or an effect of the hypertension. In the current study we demonstrated a diminished role for NO in the modulation of renal function in juvenile uni-x sheep (50% of their adult body weight at this age). In our study in aged animals, notably there was an aged related decline in the contribution of NO to the control of renal function, which was exacerbated in the uni-x sheep26. However, this renal NO deficit is still very much evident in the 6-month old uni-x lambs. In terms of basal renal function, we have shown that renal blood flow declined in the uni-x sheep significantly between the age of 1 year to 5 years.25 Given the important role of NO in maintaining renal hemodynamics, such a decrease in renal function is consistent with a decline in NO levels with ageing. However, renal NO has been shown to be a key modulator of increases in renal function which occur in the postnatal period28. Therefore, if a reduction in NO is present from a young age, this may limit the appropriate increases in renal function in the postnatal period and hasten the “normal” age-related decline in renal function. Our findings show that a reduction in NO production/bioavailabilty is present from early in life in the presence of a nephron deficit and this may be responsible for the greater decline in renal function and exacerbation of hypertension with age observed in sheep with a congenital SFK.
NO is a potent vasodilator and an important regulator of both glomerular and tubular function7. In response to systemic administration of L-NAME, in the normotensive sham lambs we observed an increase in MAP that was associated with an increase in RVR and falls in RBF, GFR, urine flow and sodium excretion similar to previous reports in sheep29 and other species30,31. MAP increased similarly in both the sham and the uni-x animals (~13 mmHg). This finding is comparable to our observations in aged female sheep in which a similar elevation in MAP (~17 mmHg) was observed in response to L-NAME in both sham and uni-x groups26. Alterations in systemic arterial pressure can, via autoregulation influence renal hemodynamics but given that the increase in arterial pressure was of a similar degree, it likely equally affected renal function in both groups. RVR comprises resistance in the pre- and post-glomerular segments of the renal vasculature. In young sham sheep, the increase in RVR in response to L-NAME was large (~300%) and was accompanied by unequal falls in GFR (54%) and RBF (72%) resulting in an increase in filtration fraction. Previous studies have also reported a lesser reduction in GFR than RBF following NOS inhibition, leading to an increase in filtration fraction32,16. This suggests that nitric oxide is acting predominantly at the efferent arterioles33. Collectively, these findings highlight the importance of endogenous NO within the kidney in the regulation of renal hemodynamics.
In marked contrast to the normotensive sham group, in the uni-x lambs the increase in RVR (~120%) and the decreases in GFR (41%) and RBF (47%) to NOS inhibition were attenuated. Since the decrease in GFR and RBF were of the same order, filtration fraction did not significantly change in uni-x animals in response to L-NAME, suggesting a similar degree of vasoconstriction at the afferent and efferent arterioles. NO has also be shown to raise GFR by increasing the glomerular ultrafiltration coefficient33 and NO deficiency might influence GFR by this mechanism but this was not addressed in the current study. Thus the kidney of uni-x sheep, due to the inability to recruit NO, may have an impaired ability to regulate net glomerular filtration pressure and thus GFR, in response to changes in perfusion pressure. In the kidney, NO is produced by endothelial NOS (eNOS) in the vasculature and neuronal NOS (nNOS) in the macula densa cells, which acts to modulate segmental renal vascular resistance and glomerular dynamics34,10. Additionally, whilst urine flow decreased by a similar extent in both groups, the reduction in sodium excretion was attenuated in the uni-x (48%) as compared to the sham lambs (76%) in response to L-NAME. This observation is similar to our observations in aged sheep26. Under normal homeostatic conditions, NO has been shown to block sodium transporters and decrease sodium and fluid reabsorption35,36,37. Thus, our findings suggest that uni-x lambs likely have a NO deficiency in both the vascular and tubular components of the nephron.
NO deficiency associated with a reduction in renal mass and/or nephron number in early life may have far reaching effects. NO is involved in the maturation of renal function in the postnatal period17,10,4. RBF and GFR are low in the fetus but increase rapidly in the postnatal period38. In newborn lambs, the rise in RBF during the postnatal period39 occurs with a concomitant increase in NO production9. Moreover the ontogeny of expression of NOS in the glomerular resistance vasculature of the newborn compared to the adult suggests a critical role for NO in modulating renal hemodynamics in the postnatal period. In the renal resistance vasculature of the newborn pig, the expression of the neuronal isoform of NOS (nNOS) is greatest, but in the adult, eNOS has the greatest expression10. In support of this, nNOS makes a greater contribution to the control of RBF in the postnatal period but in the adult pig, eNOS contributes predominantly10. In the sheep kidney, all three isoforms of NOS have the greatest expression at birth, particularly in the renal cortex and the levels start to decline from 12 weeks of age34, providing strong evidence that NO plays an important role in the regulation of renal function in the early postnatal period17. Thus, NO deficiency may drive the development of hypertension and renal dysfunction when renal mass is reduced early in life, as a result of being born with a SFK or low nephron number.
Total urinary NOx excretion was significantly lower in the uni-x lambs, indicative of a reduction in endogenous NO synthesis. Previously, in a pediatric population lower urinary NOx has been associated with acute kidney injury40. Thus, urinary nitrate may be a predictive marker of future cardiovascular and renal risk in children with a SFK. The lambs in the present study are part of a larger on-going project and as such tissues were not collected and therefore it was not possible to further directly examine the mechanistic pathways causing NO deficiency in the uni-x lambs. However, experimental and clinical studies have demonstrated that renal dysfunction is associated with a state of low NO production12,41,13 and can be a result of increased levels of assymetric dimethylarginine (ADMA)42,43, a potent competitive inhibitor of all three isoforms of NOS or a reduction in NOS activity and/or NOS expression12,44. A reduction in NO bioavailability can also be brought about in the presence of increased NOS expression. It has been shown that under pathological conditions such as hypertension, an increase in eNOS expression is observed but there is also a reduction in eNOS dimer formation and eNOS uncoupling45,46. eNOS uncoupling is the enzymatic reduction of molecular oxygen coupled to L-arginine, resulting in the generation of the superoxide, rather than NO47 and eNOS dimerization is a mechanism for preventing eNOS uncoupling48. The increased generation of reactive oxygen species (ROS) can also in turn inactivate NO, for example the nitrosylation of NO7. In developmental programming models of hypertension, oxidative stress has been implicated in reducing NO bioavailability where nitric oxide is nitrosylated to generate peroxynitrites, which mediate oxidative injury49. Indeed in our aged uni-x sheep, in addition to attenuated renal responses to systemic administration of L-NAME, we showed that inhibition of eNOS in isolated renal lobar arteries resulted in significantly lower basal tone generation26. This suggests that NO generation is impaired under basal conditions. However, this response was observed in the presence of increased renal eNOS gene and protein expression in the aged uni-x animals26. Further investigation revealed that renal arteries from aged uni-x sheep had greater levels of 3-nitrotyrosine26 suggestive of increased ROS generation and oxidative stress. Oxidative stress has been suggested to be both a cause and consequence of renal injury and hypertension50. Whether, the mechanisms of reduction in production/bioavailability of NO in younger uni-x sheep is similar to that of the aged sheep warrants further investigation. Finally, recent studies have suggested that dietary nitrate has blood pressure lowering effects and that the renal vasculature is particularly sensitive to dietary nitrate, at levels at which other beds are unresponsive51. Thus, dietary nitrate supplementation may be a viable novel therapy for children with a SFK to limit the progression of renal injury and hypertension.
Finally, at 6 months of age female uni-x lambs had a higher MAP (~6–7 mmHg) and a lower GFR (~30%) compared to the sham lambs at 6 months of age in agreement with previous studies in this model22. These findings of hypertension and renal insufficiency are also consistent with reports in other models of nephron deficiency52,53. In addition, whilst sodium excretion varied less than 5% each day in the sham group, in the uni-x lambs it varied much more widely. In the female uni-x lambs daily UNaV fluctuated by as much as 25% each day despite food intake being similar to the control group. However, over the 5 day period the total sodium excretion was not different between the groups, rather the excretion level oscillated around the mean more widely in the uni-x group. This pattern of greater variation in daily sodium excretion has also been observed in male uni-x lambs aged 6 months54. Furthermore, it has been demonstrated previously that following a saline load uni-x sheep excrete a greater amount of sodium but at a slower rate than sham animals54,55. In similar studies in rats that underwent uninephrectomy early in life, a reduced ability to excrete a sodium load has also been observed56. This situation is in marked contrast to the events that occur following uninephrectomy in adults, which in a healthy adult has little impact on renal function or blood pressure57. This study provides convincing evidence. Together this data suggests that the impairment of sodium handling in young sheep following fetal uni-x is associated with a diminished role for NO in the modulation of renal function and this may underpin the development of hypertension following loss of a kidney in early life4,58.
Conclusion
In conclusion, lambs born with a SFK have a renal NO deficit as demonstrated by an attenuated renal response to NOS inhibition and a lower total urinary NOx excretion. Therefore, alterations in the NO system could be an important prognostic marker for disease in the setting of a congenital nephron deficit. In addition, identification of the causes of the reduction in NO bioavailability warrants further investigation in this model. This could provide the groundwork for the NO system to be targeted early in life for individuals born with a SFK and individuals born with a suspected nephron deficit such as premature infants59 and infants that experience poor conditions in-utero53.
Materials and Methods
All experiments were approved by an Animal Ethics Committee of Monash University and were performed in accordance with the guidelines of the National Health and Medical Research Council of Australia. Pure-bred merino ewes were time-mated and on gestational day 90, the pregnant ewes were transported to Monash University Large Animal Facility where they were housed in lambing pens and allowed at least 10 days to acclimatize prior to undergoing surgery, as previously described60. In brief, in the ewes, on gestation day 100, anesthesia was induced with intravenous administration of thiopentone sodium (20 mg/kg, Thiobarb, Lyppard Ltd, Australia) and maintained with isoflurane (1.5–2% in oxygen, Troy Laboratories Pty Ltd, Australia) for the duration of the surgery. After preparing the ewes for surgery, a midline incision was made, the uterus was manipulated and an incision was made to pull the hind-quarters of the fetal lamb out of the uterus. An incision was made over the left flank of the fetus and the left kidney was exposed and cleared of surrounding fat. Then, unilateral nephrectomy was performed by ligating the left renal artery, vein and ureter and excising the kidney (uni-x; n = 9). In 7 fetuses, the left kidney was exposed and gently manipulated but not excised (sham; n = 7). After recovery from surgery the ewes were returned to the farm and allowed to lamb naturally. Birth weight was recorded for all lambs. Lambs remained with their mothers on pasture until 18 weeks of age when they were weaned. At 4 months of age animals underwent surgery to construct carotid arterial loops. Anesthesia was induced as described above and the right and left carotid arteries were exteriorized into skin folds to enable direct access to the carotid artery for cannulations22. At the same time, the ewes underwent bilateral ovariectomy to minimize the effect of the oestrus cycle on blood pressure and renal function22. Each of the following four experiments, on separate days, were performed in un-anesthetized lambs.
Metabolic cage-balance studies
At 6 months of age, lambs were brought into the animal housing facility and housed in pens for a week. Following this period of acclimation animals were weighed and housed individually in metabolic cages. These cages allow for the separation of feces from urine. Then, for a period of 5-days animals were meal-fed 800 g of lucerne hay and chaff and offered 5000 ml of water at 0900 h daily. Food intake, water intake and urine output over 24 hours were measured daily. A urine sample was collected each day to measure urinary sodium excretion. Additionally on the final day (day 5), urine was also collected to determine urinary nitrate concentration.
24-hour arterial pressure and heart rate
At 6 months of age 24-hour arterial pressure (mean, systolic and diastolic) and heart rate, over 3 days, were measured via a catheter (PVC tubing, 1.5 × 1.0 mm, Microtube Extrusions, NSW, Australia) inserted into the carotid artery. Following cannulation, the carotid arterial catheter was connected to a pressure transducer (pvb DPT-6000, Cellplex Pty Ltd, Australia) and a blood pressure acquisition unit. Measurements of blood pressure and heart rate were acquired in un-anesthetized lambs using the HEM Cardiovascular Monitoring system (Notochord Systems, Notochord, Japan) in real-time and averaged over 10 seconds.
Cardiovascular and renal response to vehicle infusion
Basal renal function (time control experiment) was determined over a period of 3 hours during vehicle infusion (12 ml/h 0.9% isotonic saline, Baxter Healthcare, USA). A day prior to this, all animals had a catheter inserted into their right and left jugular vein (PE tubing, 1.2 × 1.0, Microtube Extrusions, Australia) for infusion purposes. On the morning of the experiment, a Foley catheter (Size 8 or 10, Uromedical, Australia) was inserted into the bladder for continuous urine collection. 51Chromium ethylenediaminetetraacetic acid (51Cr EDTA) and para-aminohippuric acid (PAH), was administered (i.v.) for the determination of glomerular filtration rate (GFR) and renal blood flow (RBF), respectively, via clearance methods as previously described55. An equilibration period of one hour was allowed for the 51Cr EDTA and PAH to reach steady-state within the plasma. Following the equilibration period, urine samples were collected at 20 minute intervals, with an arterial blood sample (5 ml) collected mid-point, for a period of 3 hours. Blood pressure and heart rate were monitored continuously during this period.
Cardiovascular and function in response to L-NAME infusion
The renal function protocol above was repeated 2 days later to examine the effect of L-NAME administration. Cardiovascular and renal function were measured for a period of 1 hour to establish a baseline following which animals received L-NAME (40 mg/kg bolus + 20 mg/kg/h infusion, i.v., L-NAME hydrochloride, Cayman Chemical, Australia) for 2 hours. This dose of L-NAME has previously been shown to completely abolish responses to NO stimulation in conscious lambs29. Urine samples were collected every 20 minutes with a 5 ml arterial blood sample collected at each mid-point for the duration of the experiment. Urinary nitrate levels were determined before and at the end of L-NAME infusion (see below).
Sample analysis
Urine and plasma samples were frozen and stored at −20 °C. 51Cr EDTA levels were measured using a gamma counter (PerkinElmer Wizard 1470). PAH concentration was determined using a using a previously described rapid microplate assay method61 and urinary sodium concentration was measured using an electrolyte analyser (RapidChem 744, EBOS). All renal variables were corrected for body weight.
Total urinary nitrate and nitrite concentration (NOx) was measured using a colorimetric assay (Cayman Chemical Company). NOx levels were determined in urine collected during the last day of the metabolic-cage study and before and after 120 mins of L-NAME infusion. Samples were diluted in assay buffer (1:20) and assayed in duplicates as per the manufacturer’s instructions. Detection limit of the assay for NOx was 2.5 μM. The intra-assay coefficient of variation was 2.2%.
Statistical analysis
Values are presented as mean ± sem. Statistical analysis was performed using Graphpad software (Graphpad Prism 6 for Windows, Graphpad Software Inc, USA), with the level of significance set at P≤0.05. The Kolmogorov-Smirnov test was used to determine if data fitted a Gaussian distribution before further statistical analysis. An unpaired, two-tailed student’s t-test was used to compare body weight and urinary NOx levels between the sham and uni-x groups. For the 5-day metabolic-cage balance and 24-h arterial pressure and heart rate data a repeated measures analysis of variance (ANOVA) was performed with factors group (Pgroup; sham or uni-x), time (Ptime) and their interaction (Pgroup x time). For the cardiovascular and renal variables during vehicle or L-NAME infusion, a repeated measures ANOVA was performed with factors group (Pgroup; sham or uni-x), treat (Ptreat; before and during treatment) and their interaction (Pgroup x treat). A Bonferroni post-hoc test was performed to compare the responses to baseline or between groups as appropriate.
Additional Information
How to cite this article: Singh, R. R. et al. Renal Nitric Oxide Deficiency and Chronic Kidney Disease in Young Sheep Born with a Solitary Functioning Kidney. Sci. Rep. 6, 26777; doi: 10.1038/srep26777 (2016).
References
Westland, R., Kurvers, R. A., Van Wijk, J. A. & Schreuder, M. F. Risk factors for renal injury in children with a solitary functioning kidney. Pediatrics 131(2), e478 (2013).
Schreuder, M. et al. Hypertension and microalbuminuria in children with congenital solitary kidneys. J Paediatr Child Health 44(6), 363 (2008).
Sanna-Cherchi, S. et al. Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int 76(5), 528 (2009).
Fong, D. et al. Compensatory responses to nephron deficiency: Adaptive or maladaptive? Nephrology 19(3), 119 (2014).
Luyckx, V. & Brenner, B., Birth weight, malnutrition and kidney-associated outcomes—a global concern. Nat Rev Nephrol 11, 135 (2014).
Hughson, M. D. et al. Associations of glomerular number and birth weight with clinicopathological features of African Americans and whites. Am J Kidney Dis 52(1), 18 (2008).
Baylis, C. Arginine, arginine analogs and nitric oxide production in chronic kidney disease. Nat Clin Pract Nephrol 2(4), 209 (2006).
L., R. & C., B. Glomerular actions of nitric oxide. Kidney Int 48(1), 20 (1995).
Tolins, J. P., Palmer, R. M., Moncada, S. & Raij, L. Role of endothelium-derived relaxing factor in regulation of renal hemodynamic responses. Am J Physiol 258(3 Pt 2), H655 (1990).
Rodebaugh, J. et al. Neuronal nitric oxide synthase, nNOS, regulates renal hemodynamics in the postnatal developing piglet. Pediatr Res 71, 144 (2012).
Aiello, S., Remuzzi, G. & Noris, M. Nitric oxide/endothelin balance after nephron reduction. Kidney Int Suppl 65, S63 (1998).
Aiello, S. et al. Renal and systemic nitric oxide synthesis in rats with renal mass reduction. Kidney Int 52(1), 171 (1997).
Schmidt, R. J. & Baylis, C. Total nitric oxide production is low in patients with chronic renal disease. Kidney Int 58(3), 1261 (2000).
Tain, Y. L. et al. Effects of maternal L-citrulline supplementation on renal function and blood pressure in offspring exposed to maternal caloric restriction: the impact of nitric oxide pathway. Nitric Oxide 23(1), 34 (2010).
Racasan, S. et al. Perinatal L-arginine and antioxidant supplements reduce adult blood pressure in spontaneously hypertensive rats. Hypertension 44, 83 (2004).
Ballevre, L., Thonney, M. & Guignard, J. P., Nitric oxide modulates glomerular filtration and renal blood flow of the newborn rabbit. Biol Neonate 69(6), 389 (1996).
Sener, A. & Smith, F., Renal hemodynamic effects of L-NAME during postnatal maturation in conscious lambs. Pediatr Nephrol 16, 868 (2001).
Westland, R. et al. Clinical implications of the solitary functioning kidney. Clin J Am Soc Nephrol 9(5), 978 (2013).
Douglas-Denton, R., Moritz, K. M., Bertram, J. F. & Wintour, E. M. Compensatory renal growth after unilateral nephrectomy in the ovine fetus. J Am Soc Nephrol 13(2), 406 (2002).
Moritz, K. et al. Factors influencing mammalian kidney development: implications for health in adult life. Adv Anat Embryol Cell Biol 196, 1 (2008).
Maluf, N. On the enlargement of the normal congenitally solitary kidney. Br J Urol 79, 836 (1997).
Moritz, K. M., Wintour, E. M. & Dodic, M. Fetal Uninephrectomy Leads to Postnatal Hypertension and Compromised Renal Function. Hypertension 39, 1071 (2002).
Singh, R. et al. Reduced nephron endowment due to fetal uninephrectomy impairs renal sodium handling in male sheep. Clin Sci (Lond) 118(11), 669 (2010).
Singh, R. et al. Urine concentrating defects exacerbate with age in male offspring with a low nephron endowment. Am J Physiol Renal Physiol 301, F1168 (2011).
Singh, R. R. et al. Increased cardiovascular and renal risk is associated with low nephron endowment in aged females: an ovine model of fetal unilateral nephrectomy. PLos One 7(8), e42400 (2012).
Lankadeva, Y. et al. Renal dysfunction is associated with a reduced contribution of nitric oxide and enhanced vasoconstriction following a congenital renal mass reduction: An ovine model of fetal uninephrectomy Circulation 131, 280 (2015).
Alexander, B., Dasinger, J. & Intapad, S. Fetal programming and cardiovascular pathology. Compr Physiol 5, 997 (2015).
Chevalier, R. Functional adaptation to reduced renal mass in early development. Am J Physiol Renal Physiol 242, F190 (1991).
Sener, A. & Smith, F. G. Dose-dependent effects of nitric oxide synthase inhibition on systemic and renal hemodynamics in conscious lambs. Can J Physiol Pharmacol 77(1), 1 (1999).
Baylis, C., Mitruka, B. & Deng, A. Chronic blockade of nitric oxide synthesis in the rat produces systemic hypertension and glomerular damage. J Clin Invest 90(1), 278 (1992).
Granger, J. P., Alberola, A. M., Salazar, F. J. & Nakamura, T. Control of renal hemodynamics during intrarenal and systemic blockade of nitric oxide synthesis in conscious dogs. J Cardiovasc Pharmacol 20 Suppl 12, S160 (1992).
Baylis, C., Harton, P. & Engels, K., Endothelial derived relaxing factor controls renal hemodynamics in the normal rat kidney. J Am Soc Nephrol 1(6), 875 (1990).
Denton, K. M. & Anderson, W. P., Intrarenal haemodynamic and glomerular responses to inhibition of nitric oxide formation in rabbits. J Physiol 475(1), 159 (1994).
Davis, D. et al. Age dependent expression and distribution of nitric oxide (NO) synthase isoforms in the ovine kidney. Open J Mol Integr Physiol 3, 61 (2013).
Salom, M. G., Lahera, V., Miranda-Guardiola, F. & Romero, J. C., Blockade of pressure natriuresis induced by inhibition of renal synthesis of nitric oxide in dogs. Am J Physiol 262 (5 Pt 2), F718 (1992).
Lahera, V. et al. Effects of NG-nitro-L-arginine methyl ester on renal function and blood pressure. Am J Physiol 261(6 Pt 2), F1033 (1991).
Johnson, R. A. & Freeman, R. H., Pressure natriuresis in rats during blockade of the L-arginine/nitric oxide pathway. Hypertension 19(4), 333 (1992).
Aperia, A., Broberger, O., Herin, P. & Joelsson, I., Renal hemodynamics in the perinatal period. A study in lambs. Acta Physiol. Scand. 99, 261 (1977).
Aperia, A., Broberger, O. & Herin, P. Maturational changes in glomerular perfusion rate and glomerular filtration rate in lambs. Pediatr Res 8, 758 (1974).
Mian, A. I. et al. Urinary nitrate might be an early biomarker for pediatric acute kidney injury in the emergency department. Pediatr Res 70(2), 203 (2011).
Blum, M. et al. Low nitric oxide production in patients with chronic renal failure. Nephron 79(3), 265 (1998).
Jepson, R. E., Syme, H. M., Vallance, C. & Elliott, J., Plasma asymmetric dimethylarginine, symmetric dimethylarginine, l-arginine and nitrite/nitrate concentrations in cats with chronic kidney disease and hypertension. J Vet Intern Med 22(2), 317 (2008).
Fleck, C. et al. Serum concentrations of asymmetric (ADMA) and symmetric (SDMA) dimethylarginine in patients with chronic kidney diseases. Clin Chim Acta 336(1–2), 1 (2003).
Szabo, A. J. et al. Renal neuronal nitric oxide synthase protein expression as a marker of renal injury. Kidney Int 64(5), 1765 (2003).
Landmesser, U. et al. Oxidation of tetrahydrobiopterin leads to uncoupling of endothelial cell nitric oxide synthase in hypertension. J Clin Invest 111(8), 1201 (2003).
Thum, T. et al. Endothelial Nitric Oxide Synthase Uncoupling Impairs Endothelial Progenitor Cell Mobilization and Function in Diabetes. Diabetes 56(3), 666 (2007).
Montezano, A. C. & Touyz, R. M., Reactive oxygen species and endothelial function-role of nitric oxide synthase uncoupling and Nox family nicotinamide adenine dinucleotide phosphate oxidases. Basic Clin Pharmacol Toxicol 110(1), 87 (2012).
Rafikov, R. et al. eNOS activation and NO function: structural motifs responsible for the posttranslational control of endothelial nitric oxide synthase activity. J Endocrinol 210(3), 271 (2011).
Stewart, T., Jung, F. F., Manning, J. & Vehaskari, V. M., Kidney immune cell infiltration and oxidative stress contribute to prenatally programmed hypertension. Kidney Int 68(5), 2180 (2005).
Araujo, M. & Wilcox, C. S., Oxidative stress in hypertension: role of the kidney. Antioxid Redox Signal 20(1), 74 (2014).
Gao, X. et al. NADPH oxidase in the renal microvasculature is a primary target for blood pressure-lowering effects by inorganic nitrate and nitrite. Hypertension 65(1), 161 (2015).
Bagby, S. Maternal nutrition, low nephron number and hypertension in later life: Pathways of nutritional programming. J Nutr 137, 1066 (2007).
Moritz, K. M., Singh, R. R., Probyn, M. E. & Denton, K. M., Developmental programming of a reduced nephron endowment: more than just a baby’s birth weight. Am J Physiol Renal Physiol 296(1), F1 (2009).
Singh, R. R. et al. Reduced nephron endowment due to fetal uninephrectomy impairs renal sodium handling in male sheep. Clin Sci (Lond) 118(11), 669 (2010).
Lankadeva, Y. R. et al. Blunted sodium excretion in response to a saline load in 5 year old female sheep following fetal uninephrectomy. PLos One 7(10), e47528 (2012).
Mozaffari, M. S., Warren, B. K., Russell, C. M. & Schaffer, S. W., Renal function in the noninsulin-dependent diabetic rat: effects of unilateral nephrectomy. J Pharmacol Toxicol Methods 37(4), 197 (1997).
Fehrman-Ekholm, I. et al. No evidence of accelerated loss of kidney function in living kidney donors: results from a cross-sectional follow-up. Transplantation 72, 444 (2001).
Lankadeva, Y. R. et al. Loss of a kidney during fetal life: Long term consequences and lessons learnt. Am J Physiol Renal Physiol 306, F791 (2014).
Sutherland, M. R. et al. Accelerated maturation and abnormal morphology in the preterm neonatal kidney. J Am Soc Nephrol 22(7), 1365 (2011).
Singh, R. et al. Development of cardiovascular disease due to renal insufficiency in male sheep following fetal unilateral nephrectomy. J Hypertens 27(2), 386 (2009).
Agarwal, R., Rapid microplate method for PAH estimation. Am J Physiol Renal Physiol 283(2), F236 (2002).
Acknowledgements
The authors would like to thank Mr Alan McDonald and Dr Ross Young for assistance with surgeries. This work was supported by a project grant (#1046594) and fellowships to Prof Kate Denton (#1041844) and Prof Karen Moritz (#1078164) from the National Health Research Council of Australia.
Author information
Authors and Affiliations
Contributions
R.R.S. and L.K.E. performed the surgeries with personnel listed in acknowledgment and with additional assistance from K.M.M. and L.C.B. R.R.S. and L.K.E. performed all the experiments. R.R.S., L.K.E. and K.M.D. analysed the data and prepared the figures. R.R.S., K.M.M. and K.M.D. designed and planned the experiments. R.R.S. wrote the manuscript with intellectual input from L.K.E., L.C.B., M.P.S., G.A.H., K.M.M. and K.M.D.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Singh, R., Easton, L., Booth, L. et al. Renal Nitric Oxide Deficiency and Chronic Kidney Disease in Young Sheep Born with a Solitary Functioning Kidney. Sci Rep 6, 26777 (2016). https://doi.org/10.1038/srep26777
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep26777
This article is cited by
-
Blunted natriuretic response to saline loading in sheep with hypertensive kidney disease following radiofrequency catheter-based renal denervation
Scientific Reports (2021)
-
Life with one kidney
Pediatric Nephrology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.