Abstract
Oxygen therapy is widely used in emergency and critical care settings, while there is little evidence on its real therapeutic effect. The study aimed to explore the impact of arterial oxygen partial pressure (PaO2) on clinical outcomes in patients with sepsis. A large clinical database was employed for the study. Subjects meeting the diagnostic criteria of sepsis were eligible for the study. All measurements of PaO2 were extracted. The primary endpoint was death from any causes during hospital stay. Survey data analysis was performed by using individual ICU admission as the primary sampling unit. Quadratic function was assumed for PaO2 and its interaction with other covariates were explored. A total of 199,125 PaO2 samples were identified for 11,002 ICU admissions. Each ICU stay comprised 18 PaO2 samples in average. The fitted multivariable model supported our hypothesis that the effect of PaO2 on mortality risk was in quadratic form. There was significant interaction between PaO2 and SAPS-I (p = 0.007). Furthermore, the main effect of PaO2 on SOFA score was nonlinear. The study shows that the effect of PaO2 on mortality risk is in quadratic function form, and there is significant interaction between PaO2 and severity of illness.
Similar content being viewed by others
Introduction
Oxygen therapy is widely used in emergency and critical care settings, aiming to prevent and/or correct hypoxemia and hypoxia1. Tissue hypoxia is a common and devastating condition occurring in various medical conditions including infection, trauma, acute respiratory distress syndrome and circulatory shock. If not promptly treated, tissue hypoxia may further lead to multiple organ dysfunction syndrome that has been associated with significantly increased risk of death. As a result, most critical care specialists prefer early initiation of oxygen therapy, even without documented hypoxia.Furthermore, clinical guidelines seldom recommend the titration of oxygen therapy to prevent potential hyperoxemia2,3. Such situation is a result of the underestimation of adverse effect of hyperoxemia, and the side effect may not be directly observable in clinical setting.
There is a few evidence showing the association between hyperoxia and tissue damage. Short-term hyperoxia (<10 min) during anesthesia induction has been associated with the development of atelectasis4,5. For prolonged hyperoxia, inflammatory changes in the airway membrane are noted6. However, there is no empirical data showing the association of hyperoxia and mortality in the intensive care unit (ICU). Patients with sepsis are at increased risk of hypoxia because of the well-known gap between oxygen supply and oxygen demand7. On the other hand, septic patients are prone to the adverse effect of hyperoxia. Some animal studies have shown that oxygen therapy greatly influences the progression and clinical manifestation of sepsis-induced multiple system organ dysfunction8, while others reported conflicting results9,10. The underlying mechanisms for such disparity remain largely unknown based on current evidence but we proposed that different degrees of illness severity might have impact on the effect of oxygen therapy. The present study aimed to investigate the association between hyperoxia and ICU mortality in patients with sepsis. We hypothesized that (1) the effect of arterial oxygen pressure (PaO2) on mortality followed a quadratic form that both low and high PaO2 were associated with high mortality risk; (2) there is an interaction between PaO2 and severity of illness.
Methods
Database and data extraction
We employed the critical care big data named Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC-II) for the study. The latest version of MIMIC-II was version 2.6, which comprised more than 30000 ICU admissions. The database contained all clinical information during ICU stay, including demographics, laboratory findings, imaging studies, vital signs and progress notes were available11,12. The establishment of MIMIC- II was approved by the Institutional Review Boards of the Massachusetts Institute of Technology (Cambridge, MA) and Beth Israel Deaconess Medical Center (Boston, MA). De-identification was performed to ensure patients’ confidentiality. Our access to the database was approved after completion of the NIH web-based training course named “Protecting Human Research Participants” by the author Z.Z. (certification number: 1132877). Informed consent was waived because this was a study of clinical database.
Clinical information on demographics (age, gender), care unit types, physiological variables (e.g. hear rate, temperature, mean arterial blood pressure), white blood cells, ICD-9 diagnosis, microbiological results and PaO2 were extracted. The severity of illness was represented by simplified acute physiology score (SAPS-I) and sequential organ failure assessment (SOFA) scores. In the database, blood oxygen pressure was recorded without denoting whether it was venous or arterial. In patients with sepsis and/or septic shock it is common to measure both central venous and arterial blood gas. In order to distinguish between venous and arterial blood gas, we screened consecutive blood gas samples measured within 10 minutes. The difference of oxygen pressure between the two measurements should more than 20 mmHg. The one with oxygen pressure <80 mmHg was considered to be the venous oxygen pressure. As a result, a total of 4222 samples were considered to be venous oxygen pressure. The mean value of venous oxygen pressure was 36 mmHg (95% CI: 28–56 mmHg).
Inclusion criteria
Subjects meeting the diagnostic criteria of sepsis were identified from the database. Sepsis was defined according to that defined in Surviving sepsis Campaign13. SIRS was defined as more than one of the following criteria within 24 hours after ICU admission: 1) fever (>38.3 °C) or hypothermia (<36 °C); 2) tachycardia (>90/min); (3) leukocytosis (WBC count > 12000/μL) or leukopenia (WBC count < 4000/μL); (4) tachypnea (>20/min). If there were multiple records during that time period, the one most likely to fulfill the criteria was adopted (e.g. highest or lowest temperature, highest heart rate). Infection was defined as documented or suspected. Infection was defined in the database as fulfilling one of the following criteria (1) ICD9 contains the term “infection” or “pneumonia”; (2) microbiological culture was positive. The Stata codes for extracting sepsis patients from the database were described elsewhere14.
Study endpoint
The primary endpoint was death from any causes during hospital stay. Secondary endpoint was the maximum SOFA and the length of stay in ICU.
Statistical analysis
Categorical variables were expressed as the number and percentage, and their differences between survivors and non-survivors were compared using Chi-square test. Continuous variables were expressed as mean and standard deviations (SD) and compared by using t test15.
Because measurements of arterial blood gas was repeated several times for each subjects, survey data analysis was performed using individual ICU admission as the primary sampling unit. There was no stratification.
The purpose of the present study was to explore the association of PaO2 with mortality outcome, thus we forced all variables into the model for risk adjustment. These selected variables (e.g. age, sex, serum lactate, SOFA score, SAPSI, care unit type) are well documented as a risk factor for mortality16,17. To make full use of data information, missing values were replaced with the mean value of that variable18. For example, missing serum lactate was replaced by the mean value of 2.76 mmol/l. Because we hypothesized that PaO2 followed a U-shaped relationship with mortality risk, a quadratic form function was assumed for model specification. Our interests are to estimate the coefficients for the quadratic and linear term of PaO2. A quadratic function allows for one turning point at which the value of PaO2 corresponds to lowest morality rate. After determination of the quadratic main effect of PaO2, interactions between PaO2 and other variables were investigated. We employed a conservative p = 0.01 for inclusion of interaction terms. Graphical examination of the interaction effect was performed to give subject audiences a visual impression of how the effect of PaO2 changed with different levels of severity of illness. Goodness-of-fit test of the fitted model was examined by using F-adjusted mean residual test after survey data analysis19. Because the severity of illness scores could be treated as continuous variables, a multivariable linear regression model was built to investigate the association of PaO2 and the maximum SOFA score.
All statistical analyses were performed by using Stata 13.1 (StataCorp, College Station, Texas 77845 USA). A level of p < 0.05 was considered statistically significant.
Results
There are 28432 ICU admissions met the criteria of SIRS, among which only 11002 had both positive culture and partial pressure of arterial oxygenation measured. A total of 199,125 PaO2 samples were identified for 11,002 ICU admissions. Each ICU stay comprised 18 PaO2 samples in average. The distribution of PaO2 was shown in Fig. 1, which is nearly normal with an average around 120 mmHg (95% CI: 44–317 mmHg). There were 9352 survivors and 1650 non-survivors with a mortality rate of 15% (Table 1). Survivors showed significantly higher values of PaO2 than non-survivors (175.41 ± 125.42 vs. 157.30 ± 118.27 mmHg, p < 0.001). As expected, non-survivors were significantly older than survivors (69.3 ± 16.1 vs. 63.9 ± 20.0 years, p < 0.001). Serum lactate was also higher in non-survivors than in survivors (3.69 ± 3.31 vs. 2.45 ± 2.020020 mmol/l, p < 0.001). SAPS-I (19.32 ± 5.54 vs. 15.50 ± 4.92, p < 0.001) and SOFA (10.11 ± 4.51 vs. 7.04 ± 3.73, p < 0.001) were both significantly higher in non-survivors than in survivors. Overall, the care unit type was significantly different between survivors and non-survivors. Patients from MICU were more likely to die than those from other care unit types (51% vs. 41%, p < 0.05). There was no significant difference in sex between survivors and non-survivors.
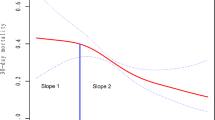
The fitted model supported our hypothesis that the effect of PaO2 on mortality risk was in quadratic form (Table 2). The odds ratio for the quadratic term was 1 (p < 0.001). Also there was significant interaction between PaO2 and SAPS-I (p = 0.007). Other potential interaction terms were not statistically significant and were excluded from the model. Covariates entered into the model were quadratic term of PaO2 (OR: 1.000, 95% CI: 1.000–1.000), linear term of PaO2 (OR: 0.990, 95% CI: 0.987–0.993), age (OR: 1.015, 95% CI: 1.009–1.020), lactate (OR: 1.081, 95% CI: 1.039–1.125), CSRU (OR: 0.474, 95% CI: 0.376–0.598), and SOFA (OR: 1.075, 95% CI: 1.042–1.109). The area under curve of the model was 0.84. Figure 2 shows the marginal effect of PaO2 on mortality risk after adjustment for other covariates. In the range of less than 300 mmHg, increasing PaO2 was associated with reduced risk of death. However, in the range of more than 300 mmHg increasing PaO2 was associated with increased risk of death. The nadir of mortality risk was at a PaO2 value of approximately 300 mmHg. Figure 3 shows the relationship between PaO2 and mortality stratified by severity of illness. At SASP-I = 6, the nadir of mortality risk occurred at a PaO2 value of 450 mmHg, after which the mortality increased. However, at SASP-I = 30 the nadir of mortality risk occurred at a PaO2 value of 200 mmHg.
The relationship between PaO2 and mortality risk at different levels of severity of illness.
Covariates except for SOFA were adjusted for in each curve. As expectedly, patients with SAPS-1 = 30 showed highest risk of death and the nadir of the curve was at the PaO2 value of 210 mmHg. In contrast, those with SAPS-1 = 6 showed the lowest risk of death across the entire PaO2 range, and the curve reaches a nadir at the PaO2 value of 420 mmHg.
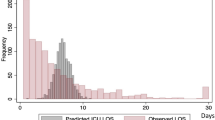
The maximum Organ failure score was the secondary endpoint reported in our analysis. Multivariable linear regression model was fitted. Again the main effect of PaO2 on SOFA score was nonlinear. The coefficient of the quadratic term was statistically significant (Table 3). The SOFA score increased monotonously with increasing PaO2 before 450 mmHg. After that further increase in PaO2 has no effect on reducing SOFA (Fig. 4).
Discussion
The study showed a significant quadratic term for the effect of PaO2 on mortality risk, indicating that hyperoxia is harmful at high levels. Furthermore, there was interaction between PaO2 and simplified physiological score, with greater negative effect of hyperoxia in patients with higher SASP-I scores. The study focused on patients with sepsis and organ failure score was employed as the secondary outcome. In our study the maximum SOFA score showed a negative correlation with PaO2, but at PaO2 > 450 mmHg the relationship disappeared. With large clinical database and sophisticated model building technique, our data support the notion that hyperoxia is harmful in critically ill patients with sepsis.
In a recent study involving patients with cardiac arrest, Elmer J. and coworkers20 reported that severe hyperoxia (defined as PaO2 > 300 mmHg) was associated with increased risk of death in both unadjusted and adjusted approaches. It is surprising that the cutoff points for negative effect of hyperoxia are so consistent in both studies, although they included different kind of patient populations. However, Elmer’s study failed to identify the association between moderate or probable hyperoxia (PaO2: 101–299 mmHg) and improved survival. This can be partly explained by the small sample size (n = 184) in their study, which lacks statistical power to detect small effect size. In our study, moderate hyperoxia was associated with significantly improved survival, and the relationship between PaO2 and risk of death was monotonically decreasing at PaO2 < 300 mmHg. Other studies involving cardiac arrest patients yielded conflicting results21,22,23. Rodríguez-González R and coworkers have investigated the effect of hyperoxia on organ dysfunction in experimental model of sepsis8. The result showed that hyperoxia had negative impact on sepsis-induced organ dysfunction. They further proved that the negative impact was mediated via inflammatory cytokines and reactive oxygen species. However, the result was not replicated in human studies. Our study showed that SOFA decreased with increasing PaO2, but the decreasing rate (slope) was reduced at higher levels of PaO2. There is a few evidence suggesting beneficial effects of hyperoxia on inflammatory response, providing support to our findings9. With respect to the mortality outcome, Stolmeijer R and coworkers reported that hyperoxia was associated with increased risk of death in sepsis patients, which is consistent with our findings24. However, they reported inspired oxygen saturation but not PaO2, which hampered further comparison with our study.
One important indication of our study is that higher levels of oxygen can be given to patients with sepsis. In convention, it is recommended to use the least inspiratory O2 fraction associated with an arterial O2 tension of 55 to 80 mm Hg or an arterial oxygen saturation of 88 to 95% 25. Our data showed that the risk of death decreases monotonously at the PaO2 values below 300 mmHg, suggesting additional benefits by increasing PaO2 to 300 mmHg. Further increment in PaO2 beyond 300 mmHg will exert negative impact on survival. Probably, the negative pathophysiological effect of hyperoxia found in experimental studies outweighs its beneficial effect at such high PaO2 levels26. On the other hand, because causal inference cannot be made in our study, it is also probable that it is the severity of illness that result in inability of the lung to transport more oxygen to arterial blood. For instance, severe acute respiratory distress syndrome with hypoxemia is a prognosticator of adverse outcome. PaO2 cannot be elevated even with aggressive treatment. Another implication of the study is that sepsis patients with higher SASP-I score are more subject to the negative impact of hyperoxia. This is somewhat contradictory to conventional ideas that more oxygen should be given to more critically ill patients. Because the interaction effect in our study used relatively conservative p value, it should be reliable and robust to further test.
The strength of the study was the use of a large clinical database. A large sample size allows for complex model building strategy with many degrees of freedom. To make our result robust, especially for interaction effect, we used conservative p value of 0.01 as the significance level. The result showed that there was interaction between PaO2 and severity of illness. Several limitations need to be acknowledged in the study. First, the selection of sepsis subjects based on data mining was not straightforward as can be done in prospective design. The diagnosis of sepsis was not incorporated into ICD-9 and we had to extract vital signs and information on possible infection to confirm the existence of sepsis. The diagnosis of SIRS can be accurate based on documented physiological signs, but infection was somewhat illusive. For example, the confirmation of infection relies partly on microbiological findings. Sometimes the positive culture result may be colonization instead of true infection. However, this method has been fully discussed by experts, reflecting the best way to define sepsis based on data extracted from electronic medical record system. Second, the study was retrospective in design and was subject to selection bias. For instance, the physician may not order arterial blood gas for patients with better conditions. Exclusion of this group of patients results in potential selection bias. Third, it is well known that sepsis combined with shock is associated with increased risk of death, and this subgroup of patients is subject to imbalance between oxygen demand and supply. It is technically challenging to distinguish between patients with and without shock. However, we used surrogate lactate to represent tissue hypoxia, which after inclusion into the model showed significant association with mortality. Forth, oxygen therapy was not fully explored in the study. There are varieties of techniques to improve oxygenation in ICU, including high-flow nasal oxygen therapy, mechanical ventilation and even extracorporeal membrane oxygenation. However, including these interventions into analysis is technically challenging. At the start point, we hypothesized that no matter what kind of intervention is employed, the ultimate goal is to improve PaO2.
In conclusion, the study shows that the effect of PaO2 on mortality risk is in quadratic function form. The increment in PaO2 was associated with reduced risk of death with PaO2 < 300 mmHg. Thereafter, the increase in PaO2 beyond 300 mmHg was associated with increased risk of death. Due to retrospective nature of the study, further experimental trials are needed to confirm our result.
Additional Information
How to cite this article: Zhang, Z. and Ji, X. Quadratic function between arterial partial oxygen pressure and mortality risk in sepsis patients: an interaction with simplified acute physiology score. Sci. Rep. 6, 35133; doi: 10.1038/srep35133 (2016).
References
Sjoberg, F. & Singer, M. The medical use of oxygen: a time for critical reappraisal. Journal of internal medicine 274, 505–528, doi: 10.1111/joim.12139 (2013).
Australian Resuscitation, C. & New Zealand Resuscitation, C. Equipment and techniques in adult advanced life support. ARC and NZRC Guideline 2010. Emergency medicine Australasia: EMA 23, 286–291, doi: 10.1111/j.1742-6723.2011.01422_14.x (2011).
Gonzalez, M. M. et al. I guideline for cardiopulmonary resuscitation and emergency cardiovascular care–Brazilian Society of Cardiology: executive summary. Arquivos brasileiros de cardiologia 100, 105–113 (2013).
Derosa, S. et al. Reabsorption atelectasis in a porcine model of ARDS: regional and temporal effects of airway closure, oxygen, and distending pressure. Journal of applied physiology 115, 1464–1473, doi: 10.1152/japplphysiol.00763.2013 (2013).
Hedenstierna, G. Alveolar collapse and closure of airways: regular effects of anaesthesia. Clinical physiology and functional imaging 23, 123–129 (2003).
Konradova, V., Janota, J., Sulova, J., Sukova, B. & Copova, M. Effects of 90% oxygen exposure on the ultrasructure of the tracheal epithelium in rabbits. Respiration; international review of thoracic diseases 54, 24–32 (1988).
Tanczos, K. & Molnar, Z. The oxygen supply-demand balance: a monitoring challenge. Best practice & research. Clinical anaesthesiology 27, 201–207, doi: 10.1016/j.bpa.2013.06.001 (2013).
Rodriguez-Gonzalez, R. et al. Multiple system organ response induced by hyperoxia in a clinically relevant animal model of sepsis. Shock 42, 148–153, doi: 10.1097/SHK.0000000000000189 (2014).
Waisman, D. et al. Dose-related effects of hyperoxia on the lung inflammatory response in septic rats. Shock 37, 95–102, doi: 10.1097/SHK.0b013e3182356fc3 (2012).
Xie, K. et al. Combination therapy with molecular hydrogen and hyperoxia in a murine model of polymicrobial sepsis. Shock 38, 656–663, doi: 10.1097/SHK.0b013e3182758646 (2012).
Saeed, M. et al. Multiparameter Intelligent Monitoring in Intensive Care II: a public-access intensive care unit database. Critical care medicine 39, 952–960, doi: 10.1097/CCM.0b013e31820a92c6 (2011).
Zhang, Z. Accessing critical care big data: a step by step approach. J Thorac Dis 7, 238–242, doi: 10.3978/j.issn.2072-1439.2015.02.14 (2015).
Dellinger, R. P. et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive care medicine 39, 165–228, doi: 10.1007/s00134-012-2769-8 (2013).
Zhang, Z., Chen, L. & Ni, H. Antipyretic therapy in critically ill patients with sepsis: an interaction with body temperature. PLoS One 10, e0121919, doi: 10.1371/journal.pone.0121919 (2015).
Zhang, Z. Univariate description and bivariate statistical inference: the first step delving into data. Ann Transl Med 4, 91, doi: 10.21037/atm.2016.02.11 (2016).
Zhang, Z. & Xu, X. Lactate clearance is a useful biomarker for the prediction of all-cause mortality in critically ill patients: a systematic review and meta-analysis*. Critical care medicine 42, 2118–2125, doi: 10.1097/CCM.0000000000000405 (2014).
Zhang, Z., Xu, X. & Chen, K. Lactate clearance as a useful biomarker for the prediction of all-cause mortality in critically ill patients: a systematic review study protocol. BMJ open 4, e004752, doi: 10.1136/bmjopen-2013-004752 (2014).
Zhang, Z. Missing data imputation: focusing on single imputation. Ann Transl Med 4, 9, doi: 10.3978/j.issn.2305-5839.2015.12.38 (2016).
Archer, K. J. & S., L. Goodness-of-fit test for a logistic regression model fitted using survey sample data. The Stata Journal 6, 97–105 (2006).
Elmer, J. et al. The association between hyperoxia and patient outcomes after cardiac arrest: analysis of a high-resolution database. Intensive care medicine 41, 49–57, doi: 10.1007/s00134-014-3555-6 (2015).
Bellomo, R. et al. Arterial hyperoxia and in-hospital mortality after resuscitation from cardiac arrest. Critical care 15, R90, doi: 10.1186/cc10090 (2011).
Kilgannon, J. H. et al. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. Jama 303, 2165–2171, doi: 10.1001/jama.2010.707 (2010).
Wang, C. H. et al. The effect of hyperoxia on survival following adult cardiac arrest: a systematic review and meta-analysis of observational studies. Resuscitation 85, 1142–1148, doi: 10.1016/j.resuscitation.2014.05.021 (2014).
Stolmeijer, R., ter Maaten, J. C., Zijlstra, J. G. & Ligtenberg, J. J. Oxygen therapy for sepsis patients in the emergency department: a little less? European journal of emergency medicine : official journal of the European Society for Emergency Medicine 21, 233–235, doi: 10.1097/MEJ.0b013e328361c6c7 (2014).
Calzia, E. et al. Hyperoxia may be beneficial. Critical care medicine 38, S559–568, doi: 10.1097/CCM.0b013e3181f1fe70 (2010).
Barth, E. et al. Effects of ventilation with 100% oxygen during early hyperdynamic porcine fecal peritonitis. Critical care medicine 36, 495–503, doi: 10.1097/01.CCM.0B013E318161FC45 (2008).
Author information
Authors and Affiliations
Contributions
Z.Z. conceived the idea and designed the study, and contributed to the manuscript drafting and statistical analysis. X.J. contributed to data analysis and manuscript drafting. All authors approved the manuscript. Z.Z. is the guarantor of the paper, taking responsibility for the integrity of the work as a whole, from inception to published article.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhang, Z., Ji, X. Quadratic function between arterial partial oxygen pressure and mortality risk in sepsis patients: an interaction with simplified acute physiology score. Sci Rep 6, 35133 (2016). https://doi.org/10.1038/srep35133
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep35133
This article is cited by
-
The PaO2/FiO2 is independently associated with 28-day mortality in patients with sepsis: a retrospective analysis from MIMIC-IV database
BMC Pulmonary Medicine (2023)
-
Hyperoxemia in postsurgical sepsis/septic shock patients is associated with reduced mortality
Critical Care (2022)
-
Perioperative Oxygenation Targets in Adults
Current Anesthesiology Reports (2019)
-
The paramount parameter: arterial oxygen tension versus arterial oxygen saturation as target in trials on oxygenation in intensive care
Critical Care (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.