Abstract
Alpha-blockers and antibiotics are most commonly used to treat chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) in clinical practice. Currently, increasing evidence also suggests acupuncture as an effective strategy. This network meta-analysis intended to assess the comparative efficacy and safety of acupuncture, alpha-blockers and antibiotics for CP/CPPS. Twelve trials involving 1203 participants were included. Based on decreases in the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) score, a network meta-analysis indicated that electro-acupuncture (standard mean difference [SMD]: 4.29; 95% credible interval [CrI], 1.96–6.65), acupuncture (SMD: 3.69; 95% CrI, 0.27–7.17), alpha-blockers (SMD: 1.85; 95% CrI, 1.07–2.64), antibiotics (SMD: 2.66; 95% CrI, 1.57–3.76), and dual therapy (SMD: 3.20; 95% CrI, 1.95–4.42) are superior to placebo in decreasing this score. Additionally, electro-acupuncture (SMD: 2.44; 95% CrI, 0.08–4.83) and dual therapy (SMD: 1.35; 95% CrI, 0.07–2.62) were more effective than alpha-blockers in decreasing the total NIH-CPSI total score. Other network meta-analyses did not show significant differences between interventions other placebo. The incidence of adverse events of acupuncture was relatively rare (5.4%) compared with placebo (17.1%), alpha-blockers (24.9%), antibiotics (31%) and dual therapy (48.6%). Overall, rank tests and safety analyses indicate that electro-acupuncture/acupuncture may be recommended for the treatment of CP/CPPS.
Similar content being viewed by others
Introduction
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) refers to National Institutes of Health (NIH) category III prostatitis, defined as urologic pain or discomfort in the pelvic region lasting for at least 3 months during the preceding 6 months that is associated with urinary symptoms, and not accompanied by a urinary tract bacterial infection1. CP/CPPS can impair both the physical and psychological function of patients and frequently diminishes their quality of life. It is the most common urological diagnosis among adult men under the age of 50 and accounts for 2 million office visits to urologists in the United States2,3. As the most common type of prostatitis, approximately 90% to 95% of men with symptoms of chronic prostatitis have CP/CPPS4. According to a survey conducted by Duloy and colleagues in 2007, the annual cost to treat prostatitis is approximately $84 million. Thus, prostatitis places a significant economic burden on both individuals and society attributed by causing productivity absenteeism and incurring health care cost3.
At present, a gold standard diagnostic test for CP/CPPS is not available because the aetiology of this disease is poorly understood. Thus, diagnosis typically based on exclusion5,6,7. In 1999, the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) was developed and has been widely used to rapidly assess the severity of CP/CPPS symptoms. This questionnaire covers the three most important symptom domains: evaluating pain, voiding and quality of life (QoL), which can provide an overall and valid assessment8.
Due to the lack of effective treatment for CP/CPPS, a wide range of therapies have been routinely used to treat this condition, including alpha-blockers, antibiotics, non-steroidal anti-inflammatory drugs (NSAIDs), and other agents9. Among these agents, alpha-blockers and antibiotics are most commonly used in clinical practice10,11. However, alpha-blockers and antibiotics exert only moderate, albeit significant, beneficial effects1. Moreover, adverse effects, such as dizziness, nausea, postural hypotension, and gastrointestinal complaints also reduce the patients’ compliance to therapy, which may affect the efficacy of treatment1,6.
In recent years, increasing evidence implicating acupuncture as a possible strategy for CP/CPPS treatment has accumulated12,13,14,15. A direct meta-analysis indicated that acupuncture is superior to sham acupuncture and partial drugs (levofloxacin, tamsulosin, and ibuprofen) in improving the symptoms of CP/CPPS16,17. However, a meta-analysis of direct comparisons between acupuncture and different classes of oral drugs is unavailable because such analyses are limited by the comparators and insufficient studies.
Network meta-analysis overcomes this limitation by creating indirect comparisons and allowing data synthesis, which could help identify the most effective interventions18,19. Therefore, we performed this Bayesian network meta-analysis and systematic review to discover both direct and indirect comparisons of acupuncture, alpha-blockers and antibiotics. To this end, we compared changes in the total NIH-CPSI score and three sub-domain scores. In addition, we also analysed the incidence rates of adverse events amongst included interventions.
Results
Study Selection
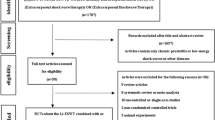
The search was performed on Feb 2nd, 2016 and identified 214 references. After duplicate studies were removed, another 87 records were excluded by reading the titles and abstracts, and the full texts of 44 articles were then assessed for eligibility. Finally, a total of 12 studies covering 7 groups, acupuncture, electro-acupuncture, alpha-blockers, antibiotics, dual therapy, sham acupuncture and placebo, were included12,13,20,21,22,23,24,25,26,27,28,29. The PRISMA flow chart of study selection is depicted in Fig. 1.
Study Description
Three trials compared acupuncture or electro-acupuncture to sham acupuncture12,20,27, one trial compared electro-acupuncture to antibiotics combined with NSAIDs13, eight trials were pooled to compare placebo with alpha-blockers or antibiotics or their combination21,22,23,24,25,26,28,29. Overall, 1203 patients were included in the network meta-analysis. The participants were come from Canada24,26,29, the United States21,23, Turkey12,13,22, Korea27, Malaysia20,21,24, and China26,29. The characteristics of included studies are summarized in Table 1. All studies reported NIH-CPSI total scores and subdomain scores as outcomes. The network plot of eligible comparisons for NIH-CPSI scores is shown in Fig. 2, and the risk of bias of studies is summarized in Table 2. Furthermore, more than half of the included trials did not provide the details of their allocation concealment. The mean, SD, and sample size between treatment groups for studies included in the network meta-analysis are summarized in Supplementary Table 1.
NIH-CPSI Total Score
Assessing primary outcome, the results of a pair-wise meta-analysis suggested that compared with sham acupuncture, acupuncture (SMD: 0.97; 95% CI, 0.17–1.78) and electro-acupuncture (SMD: 1.59; 95% CI, 0.65–2.53) resulted in significantly larger changes in the NIH-CPSI score than sham acupuncture. In addition, alpha-blockers (SMD: 1.38; 95% CI, 0.51–2.24) and antibiotics (SMD: 2.06; 95% CI, 0.18–3.96) significantly improved the NIH-CPSI score compared with placebo. The remaining 4 comparisons between other active treatments did not show the significant differences with the exception of electro-acupuncture, which was superior to dual therapy (SMD: 1.09; 95% CI, 0.52–1.67).
The network meta-analysis showed that all treatments other than sham acupuncture were more efficacious than placebo. Specifically, electro-acupuncture (SMD: 4.29; 95% CrI, 1.96–6.65), acupuncture (SMD: 3.69; 95% CrI, 0.27–7.17), alpha-blockers (SMD: 1.85; 95% CrI, 1.07–2.64), antibiotics (SMD: 2.66; 95% CrI, 1.57–3.76), and dual therapy (SMD: 3.20; 95% CrI, 1.95–4.42) were more efficacious than placebo, and network comparisons did not show no significant differences between the remaining pairs of indirect comparisons. The results of direct and indirect comparisons in the total NIH-CPSI score are shown in the lower and upper triangles of Table 3, and significant differences are underlined and bolded. The absolute effects and rank test indicated that electro-acupuncture was the most effective strategy in terms of reducing the total NIH-CPSI score, followed by acupuncture, dual therapy, antibiotics, sham acupuncture, alpha-blockers, and placebo. The surface under the cumulative ranking probabilities (SUCRA) of the total NIH-CPSI score is shown in Fig. 3.
NIH-CPSI Pain Score
The pair-wise meta-analysis showed that electro-acupuncture was preferred to sham acupuncture (SMD: 1.88; 95% CI, 2.87–0.89) and dual therapy (SMD: 0.82; 95% CI, 1.38–0.26) to improve the NIH-CPSI pain domain score. Alpha-blockers were better than placebo (SMD: 1.05; 95% CI, 0.27–1.83) in improving this score. No significant difference was detected in the remaining 6 direct comparisons.
The network meta-analysis indicated that electro-acupuncture (SMD: 2.30; 95% CrI, 0.03–4.63), dual therapy (SMD: 1.46; 95% CrI, 0.23–2.68), and antibiotics (SMD: 1.47; 95% CrI, 0.39–2.54), but not alpha-blocker, acupuncture, and sham acupuncture, were associated with a significantly higher improvement in pain relief than placebo. Compared with sham acupuncture, electro-acupuncture was better at relieving pain (SMD: 2.38; 95% CrI, 0.33–4.43). The remaining indirect comparisons did not show significant differences. The results of direct and indirect comparisons in the NIH-CPSI pain score are shown in lower and upper triangles of Table 4, and significant differences are underlined and bolded. The absolute effects and rank test indicated that electro-acupuncture ranked the first, followed by dual therapy, antibiotics, alpha-blockers, acupuncture, sham acupuncture, and placebo. The SUCRA of the NIH-CPSI pain score is shown in Fig. 4.
NIH-CPSI Voiding Score
A pair wise meta-analysis suggested that acupuncture was associated with a significantly larger improvement in the NIH-CPSI voiding domain score than sham acupuncture (SMD: 0.83; 95% CI, 0.21–1.45). Alpha-blockers (SMD: 0.75; 95% CI, 0.18–1.32) and antibiotics (SMD: 2.05; 95% CI, 0.18–3.93) resulted in larger improvements than placebo. No significant differences were detected in the remaining 6 direct comparisons.
A network meta-analysis indicated that antibiotics (SMD: 2.25; 95% CrI, 1.20–3.31), dual therapy (SMD: 1.68; 95% CrI, 0.47–2.89), and alpha-blockers (SMD: 0.91; 95% CrI, 0.14–1.67), but not acupuncture, electro-acupuncture, and sham acupuncture, were associated with significantly larger improvements than placebo. Alpha-blockers provided better voiding relief than antibiotics (SMD: 1.34; 95% CrI, 0.13–2.55). None of the other remaining indirect comparisons showed significant differences. Direct and indirect comparisons of the NIH-CPSI voiding score are shown in the lower and upper triangles of Table 5, and significant differences are underlined and bolded. The absolute effects and rank test indicated that antibiotics ranked the first, followed by acupuncture, electro-acupuncture, dual therapy, sham acupuncture, alpha-blockers, and placebo. The SUCRA of the NIH-CPSI voiding score is shown in Fig. 5.
NIH-CPSI QoL Score
A pair-wise meta-analysis showed that acupuncture was associated with a significantly larger improvement in the QoL than sham acupuncture (SMD: 1.10; 95% CI, 0.79–1.41), and alpha-blockers is superior to placebo in improving the QoL (SMD: 0.70; 95% CI, 0.09–1.31). The remaining 6 direct comparisons did not show significant differences.
A network meta-analysis indicated that dual therapy (SMD: 1.25; 95% CrI, 0.07–2.41), antibiotics (SMD: 1.22; 95% CrI, 0.20–2.25) and alpha-blockers (SMD: 0.85; 95% CrI, 0.11–1.59) significantly improved the QoL domain score compared with placebo. Antibiotics were more effective than alpha-blockers (SMD: 0.38; 95% CrI, 0.81–1.55). Drect and indirect comparisons of the NIH-CPSI QoL score are shown in the lower and upper triangles of Table 6, and significant differences are underlined and bolded. The absolute effects and rank test indicated that acupuncture ranked the first, followed by electro-acupuncture, dual therapy, antibiotics, sham acupuncture, alpha-blockers, and placebo. The SUCRA of the NIH-CPSI QoL score is shown in Fig. 6.
Safety
Eleven RCTs reported adverse events (AE)12,13,20,21,22,23,24,25,27,28,29. Dual therapy (DT) resulted in the highest incidence rate of AEs (48.6%), followed by antibiotics (31%), alpha-blockers (24.9%), and placebo (17.1%). Most of these AEs were moderate (e.g., dizziness, nausea, postural hypotension, and gastrointestinal complaints). Acupuncture was rarely associated with AEs (5.4%), which were generally mild (e.g., haematomas).
Sensitivity Analysis and Network Assumption
The heterogeneity in the pair-wise meta-analysis was high among the three pairs for each outcome (placebo compared with alpha-blockers, antibiotics, and dual therapy). After a sensitive analysis, the sources were explored in three longest studies of alpha-blockers (24 weeks) and antibiotics (12 weeks)22,26,29. However, insufficient studies in the network prevented a meta-regression. In total, 4 loops were part of this network meta-analysis. The pair-wise meta-analysis and the network meta-analysis results did not significantly differ. Moreover, the inconsistency test did not show inconsistency between loops because their 95% CI included 0, as indicated by forest plots (inconsistency test are shown in Supplementary Figures 1–4).
Discussion
The purpose of this systematic review and network meta-analysis was to identify the efficacy and safety of acupuncture and routine oral medications (alpha-blockers and antibiotics) for ameliorating the symptoms of CP/CPPS. Because dual therapy is commonly used in clinical practice, combinations of alpha blockers, antibiotics and NSAIDs were also included in the comparisons30. The assessment of the risk of bias (ROB) indicated that most included studies were characterized by a low ROB. Our primary analysis showed the following: although the direct and indirect comparison showed that all strategies except for sham acupuncture were associated with a significantly higher improvement in the total NIH-CPSI score than placebo, the results of indirect comparison of active strategies did not show significant differences between each active interventions. Ranking graphs of the primary outcome showed that electro-acupuncture was the most efficacious in improving the total NIH-CPSI score improvement, followed by acupuncture, dual therapy, antibiotics, sham acupuncture and alpha-blockers. Thus, both manual acupuncture and sham acupuncture are associated with improvement in outcomes, although an indirect comparison of these treatments did not show significant differences. Moreover, complex clinical devices seemed to have a stronger placebo effect than medication31; thus, acupuncture may associated with stronger placebo effect and expectation than medication. In terms of a safety analysis, acupuncture was associated with the lowest incidence of adverse events compared with alpha-blockers, antibiotics and dual therapy, and dual therapy was associated with the highest incidence of adverse events. In addition, for alpha-blockers and antibiotics, a longer treatment duration seemed to be more efficacious than short-term administration. These results might provide an overview of the efficacy and safety data for further clinical practice.
Because the aetiological factors of CP/CPPS remain poorly understood, treatment remains difficult. Based on clinical experience and mechanism-based reasoning, alpha-blockers and antibiotics are the two most commonly prescribed treatments prescribed by physicians. The bladder neck and prostate are rich in alpha-receptors, and alpha-receptors located in the central nervous system have been implicated in long-term pain syndromes. Recent preclinical data have suggested that alpha-blockers, such as alfuzosin, may reduce neurogenic inflammation in the lower urinary tract32,33. Moreover, alpha-blockers are commonly administered to men with BPH, which might have overlapping symptoms with CP/CPPS34,35. In addition to alpha-blockers, antibiotics such as quinolones and tetracycline are another treatment option for this disorder. Some studies have suggested that CP/CPPS is likely related to an infection with nanobacteria (NB), mainly because NB have been shown to cause multiple organic infections, especially urologic infection. However, NB are difficult to detected36,37. Nevertheless, antibiotics may be able to partially relieve the symptoms of patients with CP/CPPS because of possible underlying NB infection. With the exception of several Asian countries, acupuncture has not been used widely to treat CP/CPPS although its positive effects were initially demonstrated in 2008 by Lee in a randomized controlled trial28, and several randomized controlled trials were performed thereafter12,13,27. Acupuncture might may affect local peripheral events, spinal and central mechanisms or the combination thereof15. Furthermore, acupuncture regulates immune function, such as the cholinergic anti-inflammatory pathway, which may also be involved in inhibiting the inflammatory response38,39,40.
In 2011, Anothaisintawee and colleagues reported a network meta-analysis that compared mean symptom scores and treatment responses among oral managements for CP/CPPS, including alpha-blockers, antibiotics, anti-inflammatory drugs, and other active drugs41. This study suggested that alpha blockers, antibiotics and their combinations are appropriate strategies for the treatment of CP/CPPS. The results of our meta-analysis were consistent with the results concluded from the previous study. However, acupuncture was clearly more effective than not only placebo and sham acupuncture but also alpha blockers and antibiotics. Moreover, two pair-wise meta-analyses to assess the efficacy of acupuncture for CP/CPPS have recently been conducted16,17. The direct comparison indicated that acupuncture more effectively decrease the total NIH-CPSI score than sham acupuncture and standard medicine (levofloxacin, tamsulosin, and ibuprofen), and the evidence supported acupuncture as an effective treatment for CP/CPPS. Nonetheless, data on different classes of oral medication (alpha blocker, antibiotic, NSAIDs) were synthesized in the prior pair-wise meta-analysis due to limitations in methodology and the quantity of references, which limits the power of the aforementioned conclusion16,17. Multi-comparisons take advantage of indirect comparisons and provide a method to compare insufficient studies. In this network meta-analysis, acupuncture was compared with other routine strategies for men with CP/CPPS, and rank graphs based on absolute effects were provided.
The strengths of this study are as follows. We used a Bayesian framework to compare acupuncture with two mainstream active oral medications for CP/CPPS, and the results showed that acupuncture may be an efficacious and safe treatment for this condition. Although the results of the pooled indirect meta-analysis did not show significant differences between active treatments, an available ranking graph might be helpful for clinicians and further research. In addition, during the data synthesis, values that had been changed from baseline to final were used to arrive at a clinically worthwhile conclusion. Nevertheless, our study was also subject to limitations. Although 4 RCTs that assessed acupuncture as the control treatment, rendering direct comparison between acupuncture and oral drugs insufficient12,15,21. Additionally, half of the included studies reported changes from baseline to final13,22,24,27,28,29. In the remaining 7 studies, the changes in standard deviations were estimated with a R-value to equals to 0.5, which is a relatively conservative value and might enlarge the standard deviations compared with the originals values.
According to absolute effects and rank test, acupuncture/electro-acupuncture and dual therapy should be recommended to improve the total NIH-CPSI score. In addition, the evaluation of safety provides data to favour acupuncture. Due to the limitations in the quantity of currently available evidence, major direct comparisons were unavailable, and indirect comparisons between acupuncture and other active oral drugs did not show significant differences. High-quality randomized controlled trials with large numbers of participants that compare acupuncture to active medications should be conducted to explore the preferred options for clinical practice.
Methods
This study was developed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Network Meta-Analysis (PRISMA-NMA) checklist42. (see Supplementary Table 2, which presents the PRISMA-NMA checklist).
Study Selection
Two authors (JW and JZ) independently identified the eligible studies based on titles and abstracts. Full texts were scanned if a decision could not be made based on abstracts. Any disagreements in terms of study inclusion were resolved by discussion with a third party (ZL or ZQ).
Eligibility Criteria
Randomized controlled trials that met following criteria were included: (1) Participants diagnosed with CP/CPPS (category III prostatitis according to NIH classification)5, but participants also suffering from benign prostatic hyperplasia (BPH) were excluded. (2) Trials comparing any pair of the following interventions: electro-acupuncture, acupuncture, alpha-blockers, antibiotics, combination of alpha-blockers or antibiotics or NSAIDs, sham acupuncture and placebo. Sham acupuncture was defined as invasive needle piercing into the sham acupoints, which did not correspond to any true acupuncture points. (3) Trials reporting one of following outcomes. The primary outcome for this study was the change in the total NIH-CPSI score from baseline to final treatment. The NIH-CPSI was developed to assess the symptoms and quality of life in men with CP/CPPS (with scores ranging 0–43 points, and higher scores indicating worse symptoms); it consists of three sub-scores: pain (0–21 points), urinary symptoms (0–10 points), and quality of life (0–12 points)8. Secondary outcomes included changes in the NIH-CPSI subscales from baseline to final treatment. In addition, adverse events due to the treatments were recorded.
Data Sources and Searches
We performed electronic searches of following databases: Embase, PubMed, and the Cochrane Library. The search strategy consisted of three parts and included CP/CPPS (participants), alpha-blockers, antibiotics, acupuncture (interventions and controls), and a specific filter for randomized controlled trials (studies). The following keywords were used in combination with both MeSH terms and text words: chronic prostatitis, chronic pelvic pain, nonbacterial prostatitis, acupuncture, alpha blocker, alpha adrenergic receptor blocker, alpha adrenergic receptor antagonist, antibiotic, and antibacterial. No restriction were placed on language or publication status. In addition, to guarantee the saturation of literature, we also scanned relevant trials included by previous systematic reviews and meta-analyses for CP/CPPS as well. (see Supplementary Table 3, which describes the search terms and strategies).
Data Collection Process
Four authors independently extracted and assessed the data (data extraction: ZQ and JW; assessment: JZ and YL) using a standard spread sheet (performed by Excel; Version 15.19.1), consisting of four sheets, which included (1) general information (i.e. study design, arms, intervention types, and information about data extractor); (2) study characteristic (i.e. patients, name of intervention, content of intervention, dosage and frequency, duration and follow-up, and outcomes); (3) a risk of bias assessment (ROB: randomization, allocation, blinding of participants and personnel, blinding of outcome assessor, incomplete data, selective reporting, and other bias); and (4) a summary of outcome data (dichotomous and continuous data).
For the studies that failed to report a before-and-after difference in outcome and instead reported the mean and standard deviation at baseline and at after treatment, the change from baseline was estimated using the methods recommended in the Cochrane Handbook43. Because information on R is seldom available, so we used 0.5 to estimate R, which is considered conservative44.
Statistical Analysis
The pair-wise meta-analysis were initially performed to synthesize studies that compared the same interventions with random effects models (direct comparison) using the STATA software (Version 13.0; Stata Corporation, College Station, Texas, USA). Second, to determine comparative effectiveness, a random effects model network meta-analysis (combination of direct and indirect comparison) was developed in a Bayesian framework using Markov chain Monte Carlo simulation methods provided by the WinBUGS software (Version 1.4.3; MRC Biostatistics Unit, Cambridge, UK) with a Chaimani model45,46. The Markov chains were utilized for 50,000 simultaneous iterations based on the data and description of the proposed distributions for relevant parameters, of which, the first 10000 iterations were discarded because they may have an impact on the arbitrary value. The direct and indirect comparisons for each given pair of treatments were combined by modeling the continuous outcomes in every treatment group of enrolled studies. The NIH-CPSI score was reported as a standard mean difference (SMD) with a 95% confidence intervals (CI) for direct comparisons or 95% credible intervals (CrI) for indirect comparisons. In this process, the Brooks-Gelman-Rubin method was included to assess the convergence between direct and indirect variances47. To present the relationship among different treatments, we used a network plot to show the direct comparisons between arms. In addition, the effectiveness of each treatment among all available treatments was ranked by calculating the SMD in order48; plots of the SUCRA were generated by the STATA software49. Because the consistency among included trials is a basic principle used to conduct network meta-analyses, this result generated by an indirect comparison should be similar compared to the result derived from a direct comparison. We used the Z test to analyse the inconsistency of the model. A Z value and its corresponding p-value were calculated, and an R value less than 0.05 indicated a statistically significant difference50. The clinical, statistical, and methodological differences may be attributed to heterogeneity. The chi-squared test and I2 test were used to quantitatively assess heterogeneity quantitatively, and a p-value less than 0.1 in the chi-squared test or an I2 value statistic greater than 75% was considered significant. To identify the source of heterogeneity, sensitivity analyses were initially conducted by excluding trials with the longest or shortest duration of treatment. A meta-regression was not possible due to perform owing to the insufficient number of trials included.
Additional Information
How to cite this article: Qin, Z. et al. Network Meta-Analysis of the Efficacy of Acupuncture, Alpha-blockers and Antibiotics on Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Sci. Rep. 6, 35737; doi: 10.1038/srep35737 (2016).
References
Engeler, D. S. et al. The 2013 EAU guidelines on chronic pelvic pain: is management of chronic pelvic pain a habit, a philosophy, or a science? 10 years of development. European urology 64, 431–439 (2013).
Collins, M. M., Stafford, R. S., O’Leary, M. P. & Barry, M. J. How common is prostatitis? A national survey of physician visits. J Urol 159, 1224–1228 (1998).
Duloy, A. M., Calhoun, E. A. & Clemens, J. Q. Economic impact of chronic prostatitis. Curr Urol Rep 8, 336–339 (2007).
Roberts, R. O. et al. Prevalence of a physician-assigned diagnosis of prostatitis: the Olmsted County Study of Urinary Symptoms and Health Status Among Men. Urology 51, 578–584 (1998).
Krieger, J. N., Nyberg, L. Jr. & Nickel, J. C. NIH consensus definition and classification of prostatitis. JAMA 282, 236–237 (1999).
McNaughton, C., MacDonald, R. & Wilt, T. Interventions for chronic abacterial prostatitis. Cochrane Database Syst Rev 1, CD002080 (2001).
McNaughton, C., MacDonald, R. & Wilt, T. Diagnosis and treatment of chronic abacterial prostatitis: a systematic review. Ann Intern Med 133, 367–381 (2000).
Litwin, M. S. et al. The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. Chronic Prostatitis Collaborative Research Network. J Urol 162, 369–375 (1999).
Rees, J., Abrahams, M., Doble, A. & Cooper, A. Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline. BJU Int 116, 509–525 (2015).
Zhang, K. et al. Application of CUA Guidelines on Prostatitis in the management of chronic pelvic pain syndrome: a nationwide survey (Chinese). Zhonghua Nan Ke Xue 19, 127–131 (2013).
Murphy, A. B. & Nadler, R. B. Pharmacotherapy strategies in chronic prostatitis/chronic pelvic pain syndrome management. Expert Opin Pharmacother 11, 1255–1261 (2010).
Sahin, S. et al. Acupuncture relieves symptoms in chronic prostatitis/chronic pelvic pain syndrome: a randomized, sham-controlled trial. Prostate Cancer Prostatic Dis 18, 249–254 (2015).
Kucuk, E. V. et al. Effectiveness of acupuncture on chronic prostatitis-chronic pelvic pain syndrome category IIIB patients: a prospective, randomized, nonblinded, clinical trial. Urology 85, 636–640 (2015).
Lee, S. W., Liong, M. L., Yuen, K. H. & Krieger, J. N. Acupuncture and immune function in chronic prostatitis/chronic pelvic pain syndrome: a randomized, controlled study. Complement Ther Med 22, 965–969 (2014).
Lee, S. H. & Lee, B. C. Use of acupuncture as a treatment method for chronic prostatitis/chronic pelvic pain syndromes. Curr Urol Rep 12, 288–296 (2011).
Qin, Z., Wu, J., Zhou, J. & Liu, Z. Systematic Review of Acupuncture for Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Medicine (Baltimore) 95, e3095 (2016).
Chang, S. C., Hsu, C. H., Hsu, C. K., Yang, S. S. & Chang, S. J. The efficacy of acupuncture in managing patients with chronic prostatitis/chronic pelvic pain syndrome: A systemic review and meta-analysis. Neurourol Urodyn 6, doi: 10.1002/nau.22958 (2016).
Salanti, G., Higgins, J. P., Ades, A. E. & Ioannidis, J. P. Evaluation of networks of randomized trials. Stat Methods Med Res 17, 279–301 (2008).
Caldwell, D. M., Ades, A. E. & Higgins, J. P. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ 331, 897–900 (2005).
Lee, S. W. et al. Acupuncture versus sham acupuncture for chronic prostatitis/chronic pelvic pain. Am J Med 121, 79 e1-7 (2008).
Nickel, J. C. et al. Alfuzosin and symptoms of chronic prostatitis-chronic pelvic pain syndrome. N Engl J Med 359, 2663–2673 (2008).
Tugcu, V. et al. A placebo-controlled comparison of the efficiency of triple- and monotherapy in category III B chronic pelvic pain syndrome (CPPS). European urology 51, 1113–1117 (2007).
Alexander, R. B. et al. Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial. Ann Intern Med 141, 581–589 (2004).
Cheah, P. Y. et al. Terazosin therapy for chronic prostatitis/chronic pelvic pain syndrome: a randomized, placebo controlled trial. J Urol 169, 592–596 (2003).
Nickel, J. C. et al. Levofloxacin for chronic prostatitis/chronic pelvic pain syndrome in men: a randomized placebo-controlled multicenter trial. Urology 62, 614–617 (2003).
Zhou, Z. et al. Detection of nanobacteria infection in type III prostatitis. Urology 71, 1091–1095 (2008).
Lee, S. H. & Lee, B. C. Electroacupuncture relieves pain in men with chronic prostatitis/chronic pelvic pain syndrome: three-arm randomized trial. Urology 73, 1036–1041 (2009).
Nickel, J. C. et al. Silodosin for Men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome: Results of a Phase II Multicenter, Double-Blind, Placebo Controlled Study. The Journal of Urology 186, 125–131 (2011).
Chen, Y. et al. Effects of a 6-month course of tamsulosin for chronic prostatitis/chronic pelvic pain syndrome: a multicneter, randomized trial. World J Urol 29, 381–385 (2011).
Magistro, G. et al. Contemporary Management of Chronic Prostatitis/Chronic Pelvic Pain Syndrome. European urology 69, 286–297 (2016).
Kaptchuk, T. J., Goldman, P., Stone, D. A. & Stason, W. B. Do medical devices have enhanced placebo effects? J Clin Epidemiol 53, 786–792 (2000).
Andersson, K. E. & Gratzke, C. Pharmacology of alpha1-adrenoceptor antagonists in the lower urinary tract and central nervous system. Nat Clin Pract Urol 4, 368–378 (2007).
Geppetti, P., Nassini, R., Materazzi, S. & Benemei, S. The concept of neurogenic inflammation. BJU Int 101, Suppl 3, 2–6 (2008).
Strope, S. A. et al. Evaluative care guideline compliance is associated with provision of benign prostatic hyperplasia surgery. Urology 80, 84–89 (2012).
McVary, K. T. et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol 185, 1793–1803 (2011).
Kim, T. H., Kim, H. R. & Myung, S. C. Detection of nanobacteria in patients with chronic prostatitis and vaginitis by reverse transcriptase polymerase chain reaction. Korean J Urol 52, 194–199 (2011).
Shoskes, D. A., Thomas, K. D. & Gomez, E. Anti-nanobacterial therapy for men with chronic prostatitis/chronic pelvic pain syndrome and prostatic stones: preliminary experience. J Urol 173, 474–477 (2005).
Torres-Rosas, R. et al. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med 20, 291–295 (2014).
Kavoussi, B. & Ross, B. E. The neuroimmune basis of anti-inflammatory acupuncture. Integr Cancer Ther 6, 251–257 (2007).
Lee, S. H., Liong, M. L., Yuen, K. H. & Krieger, J. N. Acupuncture and immune function in chronic prostatitis/chornic pelvic pain syndrome: A randomized, controlled study. Complement Ther Med 22, 965–969 (2014).
Anothaisintawee, T. et al. Management of chronic prostatitis/chronic pelvic pain syndrome: a systematic review and network meta-analysis. JAMA 305, 78–86 (2011).
Hutton, B. et al. The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-analysis of Health Care Interventions: Checklist and Explanations. Ann Intern Med 162, 777–784 (2015).
Higgins, J. G. S. Cochrane handbook for systematic reviews of interventions v.5.1.0. Updated March 2011. Cochrane Web site http://handbookcochraneorg/ (2011). (Date of access:15/04/2016).
Abrams, K. R., Gillies, C. L. & Lambert, P. C. Meta-analysis of heterogeneously reported trials assessing change from baseline. Stat Med 24, 3823–3844 (2005).
Ades, A. E. et al. Bayesian methods for evidence synthesis in cost-effectiveness analysis. Pharmacoeconomics 24, 1–19 (2006).
Lu, G. & Ades, A. E. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med 23, 3105–3124 (2004).
van Valkenhoef, G. et al. Automating network meta-analysis. Res Synth Methods 3, 285–299 (2012).
Dias, S., Sutton, A. J., Ades, A. E. & Welton, N. J. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making 33, 607–617 (2013).
Chaimani, A., Higgins, J. P., Mavridis, D., Spyridonos, P. & Salanti, G. Graphical tools for network meta-analysis in STATA. PLoS One 8, e76654 (2013).
Song, F., Altman, D. G., Glenny, A. M. & Deeks, J. J. Validity of indirect comparison for estimating efficacy of competing interventions: empirical evidence from published meta-analyses. BMJ 326, 472 (2003).
Acknowledgements
The authors thanks Prof. Lawrence Mbuagbaw (Department of Clinical Epidemiology and Biostatistics, McMaster University) for his help in improving the methodology of statistical calculations and the quality of the manuscript.
Author information
Authors and Affiliations
Contributions
Z.Q. and Z.L. contributed the conception of study, had full access to all data and are responsible for the accuracy and precision of data. Acquisition of data: Z.Q. and J.W. Quality assessment: J.Z. and Y.L. Analysis and interpretation of data: Z.Q. and J.W. Statistical analysis: Z.Q., J.W. and J.T. Drafting of the manuscript: Z.Q. and J.W. Critical revision of the manuscript for important intellectual content: Z.Q. and Z.L. Administrative, technical and material support: J.W., J.T. and Y.L. Supervision: Z.L.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Qin, Z., Wu, J., Tian, J. et al. Network Meta-Analysis of the Efficacy of Acupuncture, Alpha-blockers and Antibiotics on Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Sci Rep 6, 35737 (2016). https://doi.org/10.1038/srep35737
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep35737
This article is cited by
-
The methodological quality assessment of systematic reviews/meta-analyses of chronic prostatitis/chronic pelvic pain syndrome using AMSTAR2
BMC Medical Research Methodology (2023)
-
A scoping review of network meta-analyses assessing the efficacy and safety of complementary and alternative medicine interventions
Systematic Reviews (2020)
-
Efficacy of acupuncture in the treatment of chronic prostatitis-chronic pelvic pain syndrome: a review of the literature
International Urology and Nephrology (2019)
-
Cupping therapy versus acupuncture for pain-related conditions: a systematic review of randomized controlled trials and trial sequential analysis
Chinese Medicine (2017)
-
Acupuncture for chronic prostatitis/chronic pelvic pain syndrome: study protocol for a randomized controlled trial
Trials (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.