Abstract
The aim of this study was to explore concentrations differences of soluble amyloid precursor protein (sAPP) α and β in blood plasma in patients with probable Alzheimer’s disease (AD) and cognitively healthy age-matched control subjects, as well as patients with behavioural variant frontotemporal dementia (bvFTD). Concentrations of sAPPα and β were measured using enzyme-linked immunosorbent assay technology in 80 patients with probable AD, 37 age-matched control subjects and 14 patients with bvFTD. Concentration differences were explored using parametric tests. Significantly decreased plasma concentrations in the AD group compared with both the control group and the bvFTD group were detected for sAPPβ (P=0.03 for both group comparisons), but not for sAPPα. The study provides a further piece of evidence in support of sAPPβ as a promising new biomarker of AD, which may potentially improve the diagnostic accuracy of existing markers and also enable a less invasive diagnostic workup. Further research is required to establish normal ranges and to replicate the results in independent cohorts including larger numbers of participants covering a wider spectrum of cognitive impairment.
Similar content being viewed by others
Introduction
The soluble amyloid precursor proteins (sAPP) α and β, which are the products of physiological and amyloidogenic cleavage of APP, respectively, are related to central upstream pathophysiological events in Alzheimer’s disease (AD).1 Concentration changes in cerebrospinal fluid (CSF) have been repeatedly observed in AD, and the diagnostic utility of the markers is supported by a growing number of publications.2, 3 The present study explored whether AD is also associated with concentration changes of sAPP α and β in the blood plasma. Significantly decreased plasma sAPPβ concentrations were found in patients with probable AD compared with age-matched control subjects and patients with a non-Amyloid-β (Aβ) type of dementia, suggesting a potential role as diagnostic marker.
The clinical diagnosis of AD is traditionally based on evidence of a progressive memory-predominant type of dementia, and the exclusion of alternative causes. This simple set of criteria is neither sensitive for early clinical changes nor is it specific for AD. Indicators of the AD pathophysiological process rather than of its clinical manifestations are therefore urgently needed, especially in view of upcoming disease-modifying strategies. Established biomarkers such as the CSF proteins Aβ1–42, total-Tau and phosphorylated Tau1814 and structural and functional imaging techniques such as [18F]-fluorodeoxy-glucose positron emission tomography5 show reasonable but not perfect accuracy in distinguishing probable AD from physiological aging and other neurodegenerative disorders. However, the need for invasive manoeuvres such as a lumbar puncture or the necessity of cost- and technology intensive equipment such as cyclotrons and imaging facilities severely limit population-based screening programs and serial assessments of an individual patient. Less invasive procedures for biomarker ascertainment are therefore highly desirable, but no such biomarker is available at present; so far, most research in this area focussed on Aβ1–42 in blood, with studies showing mixed results.6 Our previous research indicates that sAPP α and β in CSF are promising novel biomarkers of AD.2, 3 The present study aimed to explore their diagnostic potential in plasma.
Materials and methods and results
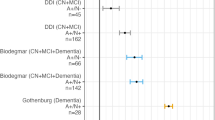
Eighty patients with probable AD (age, years: mean 73.86, s.d. 7.75; 51 men, 29 women; Mini-Mental-State Examination (MMSE) score: mean 19.54, s.d. 6.05) according to the National Institute of Neurological and Communicative Disorders and Stroke/AD and Related Disorders Association criteria, 14 patients with behavioural variant frontotemporal dementia (bvFTD) according to revised consensus criteria7 (age, years: mean 61.37, s.d. 8.89; 7 men, 7 women; MMSE score: mean 22.53, s.d.: 3.35) and 37 healthy age-matched control subjects with no subjective memory complaints and normal test results on the MMSE (age, years: mean 67.32, s.d. 9.21; 26 men, 11 women; MMSE score: mean 29.22, s.d.: 0.98) were recruited for the study at the Department of Psychiatry and Psychotherapy of Technische Universität München. The study was conducted in accordance with the 1975 Declaration of Helsinki and all study participants gave written informed consent. Plasma samples were collected as part of the clinical assessment and immediately stored in aliquots at −80 °C until further analyses. Plasma concentrations of sAPP α and β were measured in duplicate with commercial enzyme-linked immunosorbent assays (IBL, Gunma, Japan; detection range for both assays 0.78–50 ng ml−1).2 One-way analysis for variance with post-hoc Scheffé-test for normally distributed data (as indicated by the Kolmogorov–Smirnov test) were used to explore differences in plasma protein levels between patients with probable AD on the one hand and healthy control subjects and patients with bvFTD on the other. The analysis showed significantly decreased sAPPβ plasma concentrations in the AD group compared with both the healthy control group and the bvFTD group (AD: mean 3.94 ng ml−1, s.d. 4.36, range 0.78–22.32 ng ml−1; bvFTD: mean 8.01 ng ml−1, s.d. 8.26 ng ml−1, range 0.78–28.77 ng ml−1; controls: mean 5.73 ng ml−1, s.d. 0.94, range 0.78–24.03 ng ml−1; P=0.03 for both group comparisons; N=131; Figure 1), whereas the difference did not attain statistical significance for sAPPα due to a higher variability of the measured concentrations (AD: mean 18.24 ng ml−1, s.d. 17.90, range 0.78–86.24 ng ml−1; bvFTD: mean 17.93 ng ml−1, s.d. 15.99 ng ml−1, range 2.64–56.25 ng ml−1; controls: mean 9.37 ng ml−1, s.d. 1.60, range 0.78–49.93 ng ml−1; P=0.08 for AD vs controls and 0.38 for AD vs bvFTD, N=131; Figure 1). The plasma biomarker concentrations were not associated with age and gender in either of the diagnostic groups. There was no correlation between the respective protein concentrations in plasma and in CSF (N=47; results not shown).
Discussion
To the best of our knowledge, this is the first report on blood sAPP levels in AD. Our results clearly support sAPPβ in plasma as a novel, minimally invasive diagnostic marker of AD; this is an important finding in the light of urgently needed biomarkers to be used for large-scale screening purposes requiring easy and repeatable ascertainment. sAPPβ levels were decreased in our study compared with healthy aging and a non-Aβ type of dementia, which is in line with a reduced concentration of sAPPβ in AD brain cortex.8 Even though increased concentrations of full-length APP protein in blood platelets and APP mRNA levels in blood mononuclear cells have been reported in AD,9, 10 peripheral changes of APP cleavage products may be more closely related to cerebral changes due to AD than to a pathological response in the periphery. That is reduced sAPP levels possibly mirror decreased cortical APP expression in AD, which limits APP clearance across the blood-brain-barrier and/or decreased processing of APP into sAPP in blood.
Limitations of our study include the recruitment of participants at a specialized centre, the lack of histopathological verification of the clinical diagnoses, and the modest number of study participants. To conclude, our study provides a further piece of evidence in support of sAPPβ as a promising new biomarker of AD, which may potentially improve the diagnostic accuracy of existing markers and also enable a less invasive diagnostic workup. The central message of our study is that sAPPβ may serve as a blood-based marker of AD with far-reaching practical implications for patient management. Further research is required to establish normal ranges and to replicate our intriguing results in independent cohorts including larger numbers of participants covering a wider spectrum of cognitive impairment.
References
Zhang H, Ma Q, Zhang YW, Xu H . Proteolytic processing of Alzheimer's beta-amyloid precursor protein. J Neurochem 2012; 120: 9–21.
Perneczky R, Tsolakidou A, Arnold A, Diehl-Schmid J, Grimmer T, Forstl H et al. CSF soluble amyloid precursor proteins in the diagnosis of incipient Alzheimer disease. Neurology 2011; 77: 35–38.
Lewczuk P, Kamrowski-Kruck H, Peters O, Heuser I, Jessen F, Popp J et al. Soluble amyloid precursor proteins in the cerebrospinal fluid as novel potential biomarkers of Alzheimer's disease: a multicenter study. Mol Psychiatry 2010; 15: 138–145.
Schoonenboom NS, Reesink FE, Verwey NA, Kester MI, Teunissen CE, van de Ven PM et al. Cerebrospinal fluid markers for differential dementia diagnosis in a large memory clinic cohort. Neurology 2012; 78: 47–54.
Mosconi L, Tsui WH, Herholz K, Pupi A, Drzezga A, Lucignani G et al. Multicenter standardized 18F-FDG PET diagnosis of mild cognitive impairment, Alzheimer's disease, and other dementias. J Nucl Med 2008; 49: 390–398.
Song F, Poljak A, Valenzuela M, Mayeux R, Smythe GA, Sachdev PS . Meta-analysis of plasma amyloid-beta levels in Alzheimer's disease. J Alzheimers Dis 2011; 26: 365–375.
Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology 1998; 51: 1546–1554.
Wu G, Sankaranarayanan S, Hsieh SH, Simon AJ, Savage MJ . Decrease in brain soluble amyloid precursor protein beta (sAPPbeta) in Alzheimer's disease cortex. J Neurosci Res 2011; 89: 822–832.
Vignini A, Sartini D, Morganti S, Nanetti L, Luzzi S, Provinciali L et al. Platelet amyloid precursor protein isoform expression in Alzheimer's disease: evidence for peripheral marker. Int J Immunopathol Pharmacol 2011; 24: 529–534.
Jiang S, Zhang M, Ren D, Tang G, Lin S, Qian Y et al. Enhanced production of amyloid precursor protein mRNA by peripheral mononuclear blood cell in Alzheimer's disease. Am J Med Genet B Neuropsychiatr Genet 2003; 118B: 99–102.
Acknowledgements
The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We thank Dorottya Ruisz for proofreading.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Perneczky, R., Guo, LH., Kagerbauer, S. et al. Soluble amyloid precursor protein β as blood-based biomarker of Alzheimer’s disease. Transl Psychiatry 3, e227 (2013). https://doi.org/10.1038/tp.2013.11
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2013.11
Keywords
This article is cited by
-
Amyloid β-based therapy for Alzheimer’s disease: challenges, successes and future
Signal Transduction and Targeted Therapy (2023)
-
Advanced Overview of Biomarkers and Techniques for Early Diagnosis of Alzheimer’s Disease
Cellular and Molecular Neurobiology (2023)
-
Rivastigmine modifies the α-secretase pathway and potentially early Alzheimer’s disease
Translational Psychiatry (2020)
-
Plasma levels of soluble amyloid precursor protein β in symptomatic Alzheimer’s disease
European Archives of Psychiatry and Clinical Neuroscience (2018)
-
Mapping CSF biomarker profiles onto NIA–AA guidelines for Alzheimer’s disease
European Archives of Psychiatry and Clinical Neuroscience (2016)