Abstract
Brain autopsy and biomarker studies indicate that the pathology of Alzheimer’s disease (AD) is initiated at least 10–20 years before clinical symptoms. This provides a window of opportunity to initiate preventive treatment. However, this emphasizes the necessity for biomarkers that identify individuals at risk for developing AD later in life. In this cross-sectional study, originating from three epidemiologic studies in Sweden (n=1428), the objective was to examine whether amyloid pathology, as determined by low cerebrospinal fluid (CSF) concentration of the 42 amino acid form of β-amyloid (Aβ42), is associated with biomarker evidence of other pathological changes in cognitively healthy elderly. A total of 129 patients were included and CSF levels of Aβ42, total tau, tau phosphorylated at threonine 181 (p-tau), neurogranin, VILIP-1, VEGF, FABP3, Aβ40, neurofilament light, MBP, orexin A, BDNF and YKL-40 were measured. Among these healthy elderly, 35.6% (N=46) had CSF Aβ42 levels below 530 pg ml−1. These individuals displayed significantly higher CSF concentrations of t-tau (P<0.001), p-tau (181) (P<0.001), neurogranin (P=0.009) and FABP3 (P=0.044) compared with amyloid-negative individuals. Our study indicates that there is a subpopulation among healthy older individuals who have amyloid pathology along with signs of ongoing neuronal and synaptic degeneration, as well as tangle pathology. Previous studies have demonstrated that increase in CSF tau and p-tau is a specific sign of AD progression that occurs downstream of the deposition of Aβ. On the basis of this, our data suggest that these subjects are at risk for developing AD. We also confirm the association between APOE ɛ4 and amyloid pathology in healthy older individuals.
Similar content being viewed by others
Introduction
The pathological hallmarks of Alzheimer’s disease (AD), the most common cause of dementia, are the aggregation and deposition of β-amyloid (Aβ) peptides into plaques, hyperphosphorylation and aggregation of tau protein with formation of tangles along with atrophy due to neurodegeneration.1 Although still controversial, biomarkers reflecting the accumulation of Aβ deposition in the brain are believed to be the earliest detectable sign of AD in healthy elderly2, 3 and studies both in autosomal dominant AD and late-onset AD suggest that tangle formation occurs after deposition of Aβ in brain.2, 4 Three core cerebrospinal fluid (CSF) biomarkers, reflecting the key characteristics of AD pathology, are included in the diagnostic criteria.5 The presence of brain amyloid pathology is reflected by a decrease in CSF Aβ42 levels,6, 7 whereas high levels of tau correlate with greater intensity of neuronal degeneration and high levels of phosphorylated tau correlate with neurofibrillary tangle load in the brain.8
The concordance between amyloid PET images and CSF Aβ42 is above 90%.9, 10, 11 Recent failures in clinical trials, where patients who already have cognitive symptoms or dementia have been included, suggest that we need to treat AD at the prodromal or even preclinical phase of the disease. Brain autopsy studies, and more recent biomarker studies, indicate that the pathology is initiated at least 10–20 years before clinical symptoms.2, 12, 13, 14, 15, 16, 17, 18, 19 This knowledge provides a window of opportunity to initiate treatment to prevent the disease. However, this emphasizes the necessity for biomarkers that identify individuals at risk for developing AD later in life. Further, we need to gain knowledge on the development and progression of concomitant pathology.
Although presence of amyloid pathology is part of the diagnostic criteria,20 amyloid pathology is not specific for AD. Plaque pathology may be present in individuals with Parkinson’s disease21 in patients with both familial22 and iatrogenic23 Creutzfeldt–Jakob disease, and in cases with traumatic brain injury.24 We also know that around 30% of healthy elderly individuals have amyloid pathology.25, 26, 27 These data are cross-sectional and longitudinal studies are scarce. However, one longitudinal study indicates that around 20% of healthy elderly with amyloid pathology remain cognitively healthy with a follow-up of 8 years.28 In addition, other common dementias can overlap with AD both in terms of symptoms and CSF profile, and mixed pathologies are common.29 Genetic and in in vitro studies have indicated that inflammation30 and synaptic function31, 32 may be linked to Aβ production, aggregation and clearance, as well as Aβ toxicity. Previous biomarker studies support that CSF proteins may reflect such mechanisms.33, 34, 35, 36 The mechanistic and pathological similarities across neurodegenerative disorders further highlight the need for both cross-sectional studies comparing individuals with and without AD pathology and longitudinal studies starting when individuals are in the preclinical stage.
Within the framework of the population-based H70-studies in Gothenburg the aim of this study was to examine if amyloid pathology, as determined by low CSF concentration of Aβ42, is associated with biomarker evidence of other pathological changes, such as neurodegeneration, inflammation and lipid homeostasis, in cognitively healthy elderly. We have analyzed several CSF biomarkers reflecting the core pathological hallmarks of AD along with biomarkers reflecting the above-suggested pathology. Healthy elderly individuals were classified into those with (CSF Aβ42⩽530 pg ml−1) and without (CSF Aβ42>530 pg ml−1) amyloid plaque pathology.37
Materials and methods
Participants
This analysis originates from three epidemiologic studies in Gothenburg, Sweden, the Prospective Population Study of Women (PPSW) and the Gerontological and Geriatric Population Studies (H70), which have been described previously,38, 39, 40, 41 and the H85-study. The participants were sampled from the Swedish Population Register on the basis of their birth date and were born in 1914, 1918, 1922, 1923, 1924 and 1930. Both persons living in private households and in residential care were included. In the PPSW/H70 study, 1409 individuals were eligible in 2009–2010 and 857 agreed to participate (response rate 61%). Among these, 88 (10.3%) consented to a lumbar puncture (LP). The H85 study is a population study of 85-year olds born on specific dates in 1923–1924. There were 944 individuals eligible in 2008–2010, and 571 agreed to participate (response rate 61%). Among these, 62 (10.9%) consented to an LP. Overall, among the 150 with an LP, 16 were excluded due to dementia and 5 due to incomplete biomarker information, leaving 129 for the present study. These 129 participants are defined as cognitively healthy elderly as they do not fulfill the criteria for dementia and they have no previous history of memory complaints. Demographic data are shown in Table 1.
The studies were approved by the Regional Ethical Review Board in Gothenburg, and informed consent was obtained from all participants and/or their relatives in cases of dementia.
Study procedures
The clinical examination, performed at the inclusion of the population study, was conducted at an outpatient department or in the participant’s home and included comprehensive social, functional, physical, neuropsychiatric and neuropsychological examinations, as well as close informant interviews.
Neuropsychiatric examinations and interviews
Semistructured neuropsychiatric examinations were performed by trained psychiatric research nurses. These examinations included ratings of common symptoms and signs of dementia (for example, assessments of memory, orientation, general knowledge, apraxia, visuospatial function, understanding proverbs, following commands, naming ability and language) and have been described in detail previously.42, 43 Cognitive function was also measured with the Mini Mental State Examination (MMSE).44
The psychiatric nurses who performed the examinations were supervised and trained by psychiatrists. Inter-rater reliability between psychiatrists and nurses was studied in 50 individuals who had dual ratings by either psychiatric research nurses or psychiatrists. Inter-rater agreement for the symptoms and signs used to diagnose dementia was between good and excellent (kappa values between 0.74 and 1.00).45 Close informant interviews were also performed. The interviews were semistructured and comprised questions about changes in behavior and intellectual function, psychiatric symptoms and activities of daily living, and, in cases of dementia, age of onset and disease course.
Diagnoses
Dementia was diagnosed by geriatric psychiatrists according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R),46 based on symptoms rated during the neuropsychiatric examinations and information from the close informant interviews, as described previously.42, 43 Participants with dementia at baseline were excluded from further analysis.
Genotyping
Blood samples were collected and the single-nucleotide polymorphisms (SNPs) rs7412 and rs429358, in APOE (gene map locus 19q13.2) were genotyped with KASPar PCR SNP genotyping system (LGC Genomics, Hoddesdon, Herts, UK). Genotype data for these two SNPs were used to unambiguously define ɛ2, ɛ3 and ɛ4 alleles.
CSF sampling and biomarker analyses
All CSF samples were collected by LP in the L3/L4 or the L4/L5 interspace in the morning. The first 12 ml of CSF were collected in a polypropylene tube and immediately transported to the local laboratory for centrifugation at 1800 g in 20 °C for 10 min. The supernatant was gently mixed to avoid possible gradient effects, aliquoted in polypropylene tubes and stored at −70 °C.
The CSF total tau and tau phosphorylated at threonine 181 (p-tau) were determined using a sandwich enzyme-linked immunosorbent assay (ELISA; INNOTEST, Fujirebio, Ghent, Belgium) htau Ag and PHOSPHO_TAU (181P); Innogenetics, as previously described.47, 48 CSF Aβ42 was measured using a sandwich ELISA (INNOTEST β-amyloid1-42), specifically constructed to measure Aβ starting at amino acid 1 and ending at amino acid 42.49 Neurogranin and Aβ40 were measured on the Meso Scale Discovery (MSD) platform using an internally developed assay50 or the V-PLEX (Meso Scale Diagnostics, Rockland, MD, USA) Aβ Peptide Panel 1 (4G8) Kit, respectively. CSF levels of neurofilament light (NFL) were measured using the ELISA-kit from UmanDiagnostics (NF-light Umeå, Sweden).51 CSF levels of YKL-40 were determined using a sandwich ELISA (R&D Systems, Minneapolis, MN, USA)36 and levels of myelin basic protein (MBP) and brain-derived neuritic factor (BDNF) were analyzed by ELISA (Active MBP; Diagnostic Systems Laboratories, Webster, TX, USA;52 BDNF Emax Immunoassay System, Promega, Madison, WI, USA53), while the CSF levels of vascular endothelial growth factor (VEGF) and heart type fatty acid binding protein 3 (FABP3) were analyzed on the MSD platform (PLEX Plus Human VEGF Kit and Human FABP3 Kit, Meso Scale Diagnostics). CSF orexin A was analyzed by an in-house RIA.54 Finally, visinin-like protein 1 (VILIP-1) was analyzed using a commercially available ELISA (VILIP-1 Human ELISA, BioVendor R&D, Kassel, Germany) according to manufacture's instructions but with minor modifications, the calibration curve ranged from 1.25-0.02 ng ml−1 and samples were analyzed in a twofold dilution. All assays have been validated using CSF samples following a detailed protocol including precision and accuracy. CSF samples in the present study underwent a single freeze thaw cycle prior to analyses and all samples were analyzed in duplicate with a coefficient of variability (CV) acceptance criteria of <20%. Values had to pass quality control criteria, internal control samples for approval of individual plates, and kit quality controls within the expected range as defined by the Clinical Neurochemistry lab or the manufacturer.
Classification
The 129 cognitively healthy elderly individuals were classified as having brain amyloid pathology, defined as CSF Aβ42 levels (⩽530 pg ml−1), or not (>530 pg ml−1) where CSF Aβ42 was measured using ELISA (INNOTEST β-amyloid1-42). This cutoff was previously defined in a longitudinal study at the Sahlgrenska University Hospital Laboratory, to classify all subjects according to presence of biochemical evidence of AD pathology.37
Statistical analyses
Statistical analyses were performed using PASW Statistics for Windows (Version 18.0.; SPSS Chicago, IL, USA). Associations between each biomarker with age, gender, MMSE and APOE ɛ4 carrier status were tested using multivariate linear regression models. Differences in biomarker levels between the two categories of CSF Aβ42 were tested with Mann–Whitney U-tests, while differences in the distribution of APOE ɛ4 carriers between the two CSF Aβ42 categories were tested with Fisher’s exact test. Interaction effects between age group and categories of CSF Aβ42 were examined with general linear models. All tests were two-sided and statistical significance was defined as P-values <0.05.
Results
The subgroup without dementia who underwent LP had a tendency to more often be men (43.4% vs 33.8%, P=0.039), had higher MMSE (range in LP subgroup 23–30, mean 28.4 vs mean 27.6; P=0.003) and lower Brief Scale of Anxiety (BSA) score (mean 6.4 vs mean 7.7; P=0.025) compared with those who did not agree to LP. There was no difference in education, age at examination or Montgomery–Asberg Depression Scale.
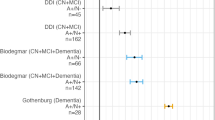
In this population-based sample, 36% of cognitively healthy individuals were biomarker positive for amyloid pathology. They had increased CSF levels of total tau (P<0.001), P-tau (181) (P<0.001), FABP3 (P=0.044) and neurogranin (P=0.009), compared with those who were biomarker negative for amyloid pathology (Figures 1a–d, Table 2). Levels of total tau, p-tau and neurogranin were significantly associated with levels of Aβ42 (P<0.001, P<0.001 and P=0.005, respectively) where lower levels of Aβ42 are linked to increased levels of the biomarker. There was no difference in the CSF levels of NFL, YKL-40, MBP, VILIP-1, BDNF, Aβ40, VEGF or orexin A between the two groups. There was no association between the CSF biomarker levels and either age, gender or MMSE.
Box plots of CSF biomarkers (a) total tau (P<0.001), (b) p-tau (P<0.001), (c) FABP3 (p0 0.044) and (d) neurogranin (P=0.009) Neurogranin, comparing those with low (< 530 pg ml−1) and high (> 530 pg ml−1) CSF Aβ42 (42 amino acid form of β-amyloid). Aβ42, amyloid β 42; CSF, cerebrospinal fluid; FABP3, fatty acid binding protein-3; p-tau, tau phosphorylated at 181.
APOE4 status was significantly associated with amyloid pathology (higher levels of AB42 were seen in those without allele 4, (P<0.001, Figure 2)) but no significant associations were seen with any other biomarker. After controlling for the effect of Aβ42 by stratifying by the cutoff value of 530 pg ml−1 there were still no apparent associations between APOE ɛ4 allele and the CSF biomarkers.
Sixty-five percent of APOE ɛ4 carriers had CSF Aβ42⩽530 pg ml−1, whereas only 20% of the non-carriers had CSF Aβ42⩽530 pg ml−1. Among APOE ɛ4 non-carriers, those biomarker positive for amyloid pathology had higher CSF levels of total tau (P<0.001), p-tau (P<0.001), neurogranin (P=0.005), YKL-40 (P=0.042), FABP3 (P=0.005) and VILIP-1 (P=0.006) than those biomarker negative for plaque pathology (Table 3). Comparing those with and without biomarker positivity for plaque pathology among the APOE ɛ4 carriers only, CSF levels of Aβ40 were significantly different, with lower levels in the group biomarker positive for plaque pathology.
Discussion
We found that 36% of cognitively healthy individuals with a mean age of 81.9 years had pathological CSF Aβ42, and that these individuals more often had two other ongoing neuropathological processes; tangle pathology, indicated by significantly increased CSF levels of p-tau, and neurodegeneration, indicated by significantly increased CSF levels of total tau (Figures 1a and b). Previous studies have demonstrated that increase in CSF p-tau is a specific sign of AD progression that occurs downstream of the deposition of Aβ.37 On the basis of this, our data suggest that these cognitively healthy older individuals are at risk for developing AD. Ongoing neurodegeneration is further supported by the significantly increased levels of neurogranin (Figure 1d), previously shown to be a specific and novel biomarker for synaptic degeneration in AD and MCI.33, 55
In further support for an ongoing neuronal degeneration associated with amyloid pathology, is the finding of increased CSF levels of the heart type FABP (FABP3; Figure 1c). FABP3 is a cytoplasmic protein abundantly expressed in tissues with an active fatty acid metabolism, such as heart, brain and liver.56 FABPs are considered as markers for neuronal damage as levels are increased after traumatic brain injury and Creutzfeldt–Jakob disease.57 Previous studies report that CSF levels of FABP3 have a diagnostic and prognostic value for AD.58, 59, 60, 61 In agreement with the present study, a recent study also found that CSF FABP3 levels (reflecting neurodegeneration) are influenced by amyloid pathology.62
We further showed a strong association between APOE ɛ4 and amyloid pathology (Figure 2). Thus, almost 70% of APOE ɛ4 carriers displayed amyloid pathology. This is in agreement with previous reports on the role of APOE ɛ4 in aggregation and clearance of Aβ,63, 64 as well as with previous biomarker studies in healthy elderly.65 Several previous studies65, 66 found a clear, allele-dependent, association between APOE ɛ4 and levels of CSF Aβ42 in older people. A recent study showed that amyloid PET-positive individuals, regardless of APOE ɛ4 status, have equally low CSF Aβ42, and PET-negative cases equally high CSF Aβ42, indicating that the lowering of CSF Aβ42 in APOE ɛ4 carriers is due to cortical Aβ deposition.67 No association between APOE ɛ4 and CSF total tau was found in agreement with previous studies.68 Further, no relationship between APOE ɛ4 status and any of the other CSF biomarkers could be demonstrated.
There was no difference in any CSF biomarkers between those with and without plaque pathology within the APOE ɛ4 carrier group, whereas CSF levels of total tau, p-tau, neurogranin, FABP3, VILIP-1 and YKL-40 were increased in those with plaque pathology in the APOE ɛ4 non-carrier group. These data indicate that amyloid pathology alone is driving concomitant pathology represented by neurodegeneration (VILIP-1, total tau and FABP3), synaptic degeneration (neurogranin), tangle pathology (p-tau) and inflammation (YKL-40), independently of the APOE ɛ4 carrier status. Longitudinal data are needed to elucidate whether these individuals have an even higher risk of developing AD, and whether the potential disease progression rate is different.
Individuals with no amyloid pathology and no APOE ɛ4 allele seem to present few signs of ongoing pathological processes indicating that they are at very low risk of developing AD or other neurodegenerative disorders. Long-term follow-up studies are of great importance to confirm this hypothesis. A recent study with longitudinal follow-up69 indicates that AD biomarker patterns are detected already during early middle age and that these are associated with amyloid PET positivity and cognitive decline, supporting that there is a long preclinical period where concomitant pathology is present. Although the present study is cross-sectional, our data support this conclusion.
The cutoff for classification into amyloid-positive and -negative has previously been defined in a longitudinal study at the Sahlgrenska hospital.37 Several studies have confirmed that there is a direct correlation between CSF Aβ42 levels and amyloid plaque load measured by PET in patients with AD and MCI. However, less is known about the correlation between these two readouts in healthy elderly and absence of amyloid PET in the present study is a potential weakness. However, a recent study by Sutphen et al.69 found an association between CSF Aβ42 and amyloid PET in middle-aged individuals. It is likely that this is true also in healthy older persons. It has also been suggested that CSF Aβ42 is an earlier indicator of Aβ aggregation compared with PET.2, 69 Our finding that 36% of healthy older persons in the population had amyloid pathology is consistent with previous findings. It is even slightly lower compared with a study where 65% of healthy elderly above 80 years were amyloid PET positive.70 The latter study support a gradual increase in number of PET-positive healthy elderly with age, 10% in the age between 50–59 years and 18% in the age between 60–69 years.
There was no increase in CSF levels of NFL, a suggested marker for subcortical pathology, among those with amyloid pathology. Previous studies indicate a positive correlation between CSF NFL and total tau in AD as well as an association between subcortical axonal degeneration and the three core biomarkers.71 However, these individuals were under clinical investigation for AD in a memory clinic, indicating that cognitive symptoms were present, which is not the case in the present study. One may speculate that changes in NFL may be a later event; however, this needs to be confirmed in a longitudinal follow-up study.
Among the strengths of this study are the representative population-based sample, the comprehensive examinations conducted by trained psychiatric nurses and the exclusion of participants with dementia. However, some limitations need to be addressed. First, the overall number of participants is relatively low. We therefore did not have the statistical power to carry out a stratified analysis regarding heterozygous and homozygous APOE ɛ4 status. Second, only ~15% consented to LP. This group had higher global cognitive function and is probably healthier than the general population of the same age. Finally, this is a population study focusing on Scandinavian participants aged 79–95 years at baseline, and results cannot be generalized to clinical samples to younger populations or to other ethnic groups.
Our study indicates that there is a subpopulation among healthy older individuals that have amyloid pathology have abnormal levels of the CSF biomarkers tau, p-tau, FABP3 and neurogranin. We also confirm the association between APOE ɛ4 and amyloid pathology in healthy elderly individuals. These findings support the notion that preclinical amyloid pathology is associated with biomarker evidence of neurodegeneration, tau pathology and synaptic dysfunction already in cognitively normal elderly.
References
Blennow K, de Leon MJ, Zetterberg H . Alzheimer's disease. Lancet 2006; 368: 387–403.
Bateman RJ, Xiong C, Benzinger TL, Fagan AM, Goate A, Fox NC et al. Clinical and biomarker changes in dominantly inherited Alzheimer's disease. N Engl J Med 2012; 367: 795–804.
Fagan AM, Head D, Shah AR, Marcus D, Mintun M, Morris JC et al. Decreased cerebrospinal fluid Abeta(42) correlates with brain atrophy in cognitively normal elderly. Ann Neurol 2009; 65: 176–183.
Buchhave P, Minthon L, Zetterberg H, Wallin AK, Blennow K, Hansson O . Cerebrospinal fluid levels of beta-amyloid 1-42, but not of tau, are fully changed already 5 to 10 years before the onset of Alzheimer dementia. Arch Gen Psychiatry 2012; 69: 98–106.
Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J et al. Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 2007; 6: 734–746.
Fagan AM, Mintun MA, Mach RH, Lee SY, Dence CS, Shah AR et al. Inverse relation between in vivo amyloid imaging load and cerebrospinal fluid Abeta42 in humans. Ann Neurol 2006; 59: 512–519.
Strozyk D, Blennow K, White LR, Launer LJ . CSF Abeta 42 levels correlate with amyloid-neuropathology in a population-based autopsy study. Neurology 2003; 60: 652–656.
Blennow K, Hampel H, Weiner M, Zetterberg H . Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat Rev Neurol 2010; 6: 131–144.
Mattsson N, Insel PS, Landau S, Jagust W, Donohue M, Shaw LM et al. Diagnostic accuracy of CSF Ab42 and florbetapir PET for Alzheimer's disease. Ann Clin Transl Neurol 2014; 1: 534–543.
Palmqvist S, Zetterberg H, Blennow K, Vestberg S, Andreasson U, Brooks DJ et al. Accuracy of brain amyloid detection in clinical practice using cerebrospinal fluid beta-amyloid 42: a cross-validation study against amyloid positron emission tomography. JAMA Neurol 2014; 71: 1282–1289.
Fagan AM, Mintun MA, Shah AR, Aldea P, Roe CM, Mach RH et al. Cerebrospinal fluid tau and ptau(181) increase with cortical amyloid deposition in cognitively normal individuals: implications for future clinical trials of Alzheimer's disease. EMBO Mol Med 2009; 1: 371–380.
Braak H, Braak E . Diagnostic criteria for neuropathologic assessment of Alzheimer's disease. Neurobiol Aging 1997; 18 (4 Suppl): S85–S88.
Fagan AM, Xiong C, Jasielec MS, Bateman RJ, Goate AM, Benzinger TL et al. Longitudinal change in CSF biomarkers in autosomal-dominant Alzheimer's disease. Sci Transl Med 2014; 6 226ra30.
Gomez-Isla T, Price JL, McKeel DW Jr., Morris JC, Growdon JH, Hyman BT . Profound loss of layer II entorhinal cortex neurons occurs in very mild Alzheimer's disease. J Neurosci 1996; 16: 4491–4500.
Hulette CM, Welsh-Bohmer KA, Murray MG, Saunders AM, Mash DC, McIntyre LM . Neuropathological and neuropsychological changes in "normal" aging: evidence for preclinical Alzheimer disease in cognitively normal individuals. J Neuropathol Exp Neurol 1998; 57: 1168–1174.
Markesbery WR, Schmitt FA, Kryscio RJ, Davis DG, Smith CD, Wekstein DR . Neuropathologic substrate of mild cognitive impairment. Arch Neurol 2006; 63: 38–46.
Morris JC, Price JL . Pathologic correlates of nondemented aging, mild cognitive impairment, and early-stage Alzheimer's disease. J Mol Neurosci 2001; 17: 101–118.
Price JL, Ko AI, Wade MJ, Tsou SK, McKeel DW, Morris JC . Neuron number in the entorhinal cortex and CA1 in preclinical Alzheimer disease. Arch Neurol 2001; 58: 1395–1402.
Villemagne VL, Burnham S, Bourgeat P, Brown B, Ellis KA, Salvado O et al. Amyloid beta deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer's disease: a prospective cohort study. Lancet Neurol 2013; 12: 357–367.
Dubois B, Feldman HH, Jacova C, Hampel H, Molinuevo JL, Blennow K et al. Advancing research diagnostic criteria for Alzheimer's disease: the IWG-2 criteria. Lancet Neurol 2014; 13: 614–629.
Kotzbauer PT, Cairns NJ, Campbell MC, Willis AW, Racette BA, Tabbal SD et al. Pathologic accumulation of alpha-synuclein and Abeta in Parkinson disease patients with dementia. Arch Neurol 2012; 69: 1326–1331.
Ghoshal N, Cali I, Perrin RJ, Josephson SA, Sun N, Gambetti P et al. Codistribution of amyloid beta plaques and spongiform degeneration in familial Creutzfeldt-Jakob disease with the E200K-129M haplotype. Arch Neurol 2009; 66: 1240–1246.
Jaunmuktane Z, Mead S, Ellis M, Wadsworth JD, Nicoll AJ, Kenny J et al. Evidence for human transmission of amyloid-beta pathology and cerebral amyloid angiopathy. Nature 2015; 525: 247–250.
Hong YT, Veenith T, Dewar D, Outtrim JG, Mani V, Williams C et al. Amyloid imaging with carbon 11-labeled Pittsburgh compound B for traumatic brain injury. JAMA Neurol 2014; 71: 23–31.
Aizenstein HJ, Nebes RD, Saxton JA, Price JC, Mathis CA, Tsopelas ND et al. Frequent amyloid deposition without significant cognitive impairment among the elderly. Arch Neurol 2008; 65: 1509–1517.
Jack CR Jr., Lowe VJ, Weigand SD, Wiste HJ, Senjem ML, Knopman DS et al. Serial PIB and MRI in normal, mild cognitive impairment and Alzheimer's disease: implications for sequence of pathological events in Alzheimer's disease. Brain 2009; 132 (Pt 5): 1355–1365.
Pike KE, Savage G, Villemagne VL, Ng S, Moss SA, Maruff P et al. Beta-amyloid imaging and memory in non-demented individuals: evidence for preclinical Alzheimer's disease. Brain 2007; 130 (Pt 11): 2837–2844.
Villemagne VL, Pike KE, Darby D, Maruff P, Savage G, Ng S et al. Abeta deposits in older non-demented individuals with cognitive decline are indicative of preclinical Alzheimer's disease. Neuropsychologia 2008; 46: 1688–1697.
Skillback T, Farahmand BY, Rosen C, Mattsson N, Nagga K, Kilander L et al. Cerebrospinal fluid tau and amyloid-beta1-42 in patients with dementia. Brain 2015; 138 (Pt 9): 2716–2731.
Bouvier DS, Murai KK . Synergistic actions of microglia and astrocytes in the progression of Alzheimer's disease. J Alzheimers Dis 2015; 45: 1001–1014.
Cirrito JR, Yamada KA, Finn MB, Sloviter RS, Bales KR, May PC et al. Synaptic activity regulates interstitial fluid amyloid-beta levels in vivo. Neuron 2005; 48: 913–922.
Koffie RM, Hyman BT, Spires-Jones TL . Alzheimer's disease: synapses gone cold. Mol Neurodegener 2011; 6: 63.
Kvartsberg H, Duits FH, Ingelsson M, Andreasen N, Ohrfelt A, Andersson K et al. Cerebrospinal fluid levels of the synaptic protein neurogranin correlates with cognitive decline in prodromal Alzheimer's disease. Alzheimers Dement 2014; 11: 1180–1190.
Lee JM, Blennow K, Andreasen N, Laterza O, Modur V, Olander J et al. The brain injury biomarker VLP-1 is increased in the cerebrospinal fluid of Alzheimer disease patients. Clin Chem 2008; 54: 1617–1623.
Olsson B, Hertze J, Lautner R, Zetterberg H, Nagga K, Hoglund K et al. Microglial markers are elevated in the prodromal phase of Alzheimer's disease and vascular dementia. J Alzheimers Dis 2013; 33: 45–53.
Rosen C, Andersson CH, Andreasson U, Molinuevo JL, Bjerke M, Rami L et al. Increased levels of chitotriosidase and YKL-40 in cerebrospinal fluid from patients with Alzheimer's disease. Dement Geriatr Cogn Dis Extra 2014; 4: 297–304.
Hansson O, Zetterberg H, Buchhave P, Londos E, Blennow K, Minthon L . Association between CSF biomarkers and incipient Alzheimer's disease in patients with mild cognitive impairment: a follow-up study. Lancet Neurol 2006; 5: 228–234.
Steen B, Djurfeldt H . The gerontological and geriatric population studies in Gothenburg, Sweden. Z Gerontol 1993; 26: 163–169.
Bengtsson C, Ahlqwist M, Andersson K, Bjorkelund C, Lissner L, Soderstrom M . The Prospective Population Study of Women in Gothenburg, Sweden, 1968-69 to 1992-93. A 24-year follow-up study with special reference to participation, representativeness, and mortality. Scand J Prim Health Care 1997; 15: 214–219.
Skoog I . Psychiatric epidemiology of old age: the H70 study—the NAPE lecture 2003. Acta Psychiatr Scand 2004; 109: 4–18.
Karlsson B, Klenfeldt IF, Sigstrom R, Waern M, Ostling S, Gustafson D et al. Prevalence of social phobia in non-demented elderly from a swedish population study. Am J Geriatr Psychiatry 2009; 17: 127–135.
Guo X, Waern M, Sjogren K, Lissner L, Bengtsson C, Bjorkelund C et al. Midlife respiratory function and Incidence of Alzheimer's disease: a 29-year longitudinal study in women. Neurobiol Aging 2007; 28: 343–350.
Skoog I, Nilsson L, Palmertz B, Andreasson LA, Svanborg A . A population-based study of dementia in 85-year-olds. N Engl J Med 1993; 328: 153–158.
Folstein MF, Folstein SE, McHugh PR . "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–198.
Wancata J, Borjesson-Hanson A, Ostling S, Sjogren K, Skoog I . Diagnostic criteria influence dementia prevalence. Am J Geriatr Psychiatry 2007; 15: 1034–1045.
American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 3rd edn. American Psychiatric Disorders: Washington DC, 1987.
Blennow K, Wallin A, Agren H, Spenger C, Siegfried J, Vanmechelen E . Tau protein in cerebrospinal fluid: a biochemical marker for axonal degeneration in Alzheimer disease? Mol Chem Neuropathol 1995; 26: 231–245.
Vanmechelen E, Vanderstichele H, Davidsson P, Van Kerschaver E, Van Der Perre B, Sjogren M et al. Quantification of tau phosphorylated at threonine 181 in human cerebrospinal fluid: a sandwich ELISA with a synthetic phosphopeptide for standardization. Neurosci Lett 2000; 285: 49–52.
Andreasen N, Hesse C, Davidsson P, Minthon L, Wallin A, Winblad B et al. Cerebrospinal fluid beta-amyloid(1-42) in Alzheimer disease: differences between early- and late-onset Alzheimer disease and stability during the course of disease. Arch Neurol 1999; 56: 673–680.
Kvartsberg H, Portelius E, Andreasson U, Brinkmalm G, Hellwig K, Lelental N et al. Characterization of the postsynaptic protein neurogranin in paired cerebrospinal fluid and plasma samples from Alzheimer's disease patients and healthy controls. Alzheimers Res Ther 2015; 7: 40.
Norgren N, Rosengren L, Stigbrand T . Elevated neurofilament levels in neurological diseases. Brain Res 2003; 987: 25–31.
Bjerke M, Jonsson M, Nordlund A, Eckerstrom C, Blennow K, Zetterberg H et al. Cerebrovascular biomarker profile is related to white matter disease and ventricular dilation in a LADIS substudy. Dement Geriatr Cogn Dis Extra 2014; 4: 385–394.
Pillai A, Bruno D, Sarreal AS, Hernando RT, Saint-Louis LA, Nierenberg J et al. Plasma BDNF levels vary in relation to body weight in females. PLoS ONE 2012; 7: e39358.
Portelius E, Soininen H, Andreasson U, Zetterberg H, Persson R, Karlsson G et al. Exploring Alzheimer molecular pathology in Down's syndrome cerebrospinal fluid. Neurodegener Dis 2014; 14: 98–106.
Wellington H, Paterson RW, Portelius E, Tornqvist U, Magdalinou N, Fox NC et al. Increased CSF neurogranin concentration is specific to Alzheimer disease. Neurology 2016; 86: 829–835.
Moulle VS, Cansell C, Luquet S, Cruciani-Guglielmacci C . The multiple roles of fatty acid handling proteins in brain. Front Physiol 2012; 3: 385.
Pelsers MM, Glatz JF . Detection of brain injury by fatty acid-binding proteins. Clin Chem Lab Med 2005; 43: 802–809.
Chiasserini D, Parnetti L, Andreasson U, Zetterberg H, Giannandrea D, Calabresi P et al. CSF levels of heart fatty acid binding protein are altered during early phases of Alzheimer's disease. J Alzheimers Dis 2010; 22: 1281–1288.
Olsson B, Hertze J, Ohlsson M, Nagga K, Hoglund K, Basun H et al. Cerebrospinal fluid levels of heart fatty acid binding protein are elevated prodromally in Alzheimer's disease and vascular dementia. J Alzheimers Dis 2013; 34: 673–679.
Rosen C, Mattsson N, Johansson PM, Andreasson U, Wallin A, Hansson O et al. Discriminatory analysis of biochip-derived protein patterns in CSF and plasma in neurodegenerative diseases. Front Aging Neurosci 2011; 3: 1.
Bjerke M, Kern S, Blennow K, Zetterberg H, Waern M, Borjesson-Hanson A et al. Cerebrospinal fluid fatty acid-binding protein 3 is related to dementia development in a population-based sample of older adult women followed for 8 years. J Alzheimers Dis 2015.
Desikan RS, Thompson WK, Holland D, Hess CP, Brewer JB, Zetterberg H et al. Heart fatty acid binding protein and Abeta-associated Alzheimer's neurodegeneration. Mol Neurodegener 2013; 8: 39.
Castellano JM, Kim J, Stewart FR, Jiang H, DeMattos RB, Patterson BW et al. Human apoE isoforms differentially regulate brain amyloid-beta peptide clearance. Sci Transl Med 2011; 3: 89ra–57.
Kim J, Basak JM, Holtzman DM . The role of apolipoprotein E in Alzheimer's disease. Neuron 2009; 63: 287–303.
Sunderland T, Mirza N, Putnam KT, Linker G, Bhupali D, Durham R et al. Cerebrospinal fluid beta-amyloid1-42 and tau in control subjects at risk for Alzheimer's disease: the effect of APOE epsilon4 allele. Biol Psychiatry 2004; 56: 670–676.
Prince JA, Zetterberg H, Andreasen N, Marcusson J, Blennow K . APOE epsilon4 allele is associated with reduced cerebrospinal fluid levels of Abeta42. Neurology 2004; 62: 2116–2118.
Lautner R, Palmqvist S, Mattsson N, Andreasson U, Wallin A, Palsson E et al. Apolipoprotein E genotype and the diagnostic accuracy of cerebrospinal fluid biomarkers for Alzheimer disease. JAMA Psychiatry 2014; 71: 1183–1191.
Andreasen N, Minthon L, Clarberg A, Davidsson P, Gottfries J, Vanmechelen E et al. Sensitivity, specificity, and stability of CSF-tau in AD in a community-based patient sample. Neurology 1999; 53: 1488–1494.
Sutphen CL, Jasielec MS, Shah AR, Macy EM, Xiong C, Vlassenko AG et al. Longitudinal cerebrospinal fluid biomarker changes in preclinical Alzheimer disease during middle age. JAMA Neurol 2015; 72: 1029–1042.
Rowe CC, Ellis KA, Rimajova M, Bourgeat P, Pike KE, Jones G et al. Amyloid imaging results from the Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging. Neurobiol Aging 2010; 31: 1275–1283.
Skillback T, Farahmand B, Bartlett JW, Rosen C, Mattsson N, Nagga K et al. CSF neurofilament light differs in neurodegenerative diseases and predicts severity and survival. Neurology 2014; 83: 1945–1953.
Acknowledgements
We acknowledge the work by Åsa Källén and Ulrika Törnqvist for the biochemical analyses as well as Tom Marlow for the statistical analyses. This work was supported by grants from The Swedish Research Council (The Swedish Research Council 14002, 11267, 2005-8460, 825-2007-7462, 825-2012-5041, 2013-8717), Swedish Research Council for Health, Working Life and Wellfare (2001-2835 AGECAP 2013-2300, 2013-2496, 2013-0475, Epilife 2006-1506), the Alzheimer's Association (IIRG-09-131338), the Eivind och Elsa K:son Sylvan Foundation, Stiftelsen Söderström-Königska Sjukhemmet, Stiftelsen för Gamla Tjänarinnor, Stiftelsen Professor Bror Gadelius’ Minnesfond, Hjalmar Svenssons Foundation, the Swedish Alzheimer Foundation, the Alma och Anna Yhlen Foundation, Konung Gustaf V:s och Drottning Victorias Stiftelse, Swedish Brain Power, Sahlgrenska University Hospital (ALF), the Knut and Alice Wallenberg Foundation, the Torsten Söderberg Foundation, Frimurarestiftelsen and Hjärnfonden. KB and HZ are co-founders of Brain Biomarker Solutions in Gothenburg AB, a GU Venture-based platform company at the University of Gothenburg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
KB and HZ are co-founders of Brain Biomarker Solutions in Gothenburg AB, a GU Venture-based platform company at the University of Gothenburg. KB has served as a consultant for Eli Lilly, Novartis, Roche Diagnostics, and Sanofi-Aventis and at Advisory Boards for Amgen and IBL International, and given lectures for Fujirebio Europe and Lundbeck. KB’s research team has received grants for collaborative research projects from Eli Lilly and Roche Diagnostics. KH, AZ, SK, IS and AB have nothing to disclose. As primary authors, KH and SK have had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Höglund, K., Kern, S., Zettergren, A. et al. Preclinical amyloid pathology biomarker positivity: effects on tau pathology and neurodegeneration. Transl Psychiatry 7, e995 (2017). https://doi.org/10.1038/tp.2016.252
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2016.252