Relaxation of the one child policy and trends in caesarean section rates and birth outcomes in China between 2012 and 2016: observational study of nearly seven million health facility births
BMJ 2018; 360 doi: https://doi.org/10.1136/bmj.k817 (Published 05 March 2018) Cite this as: BMJ 2018;360:k817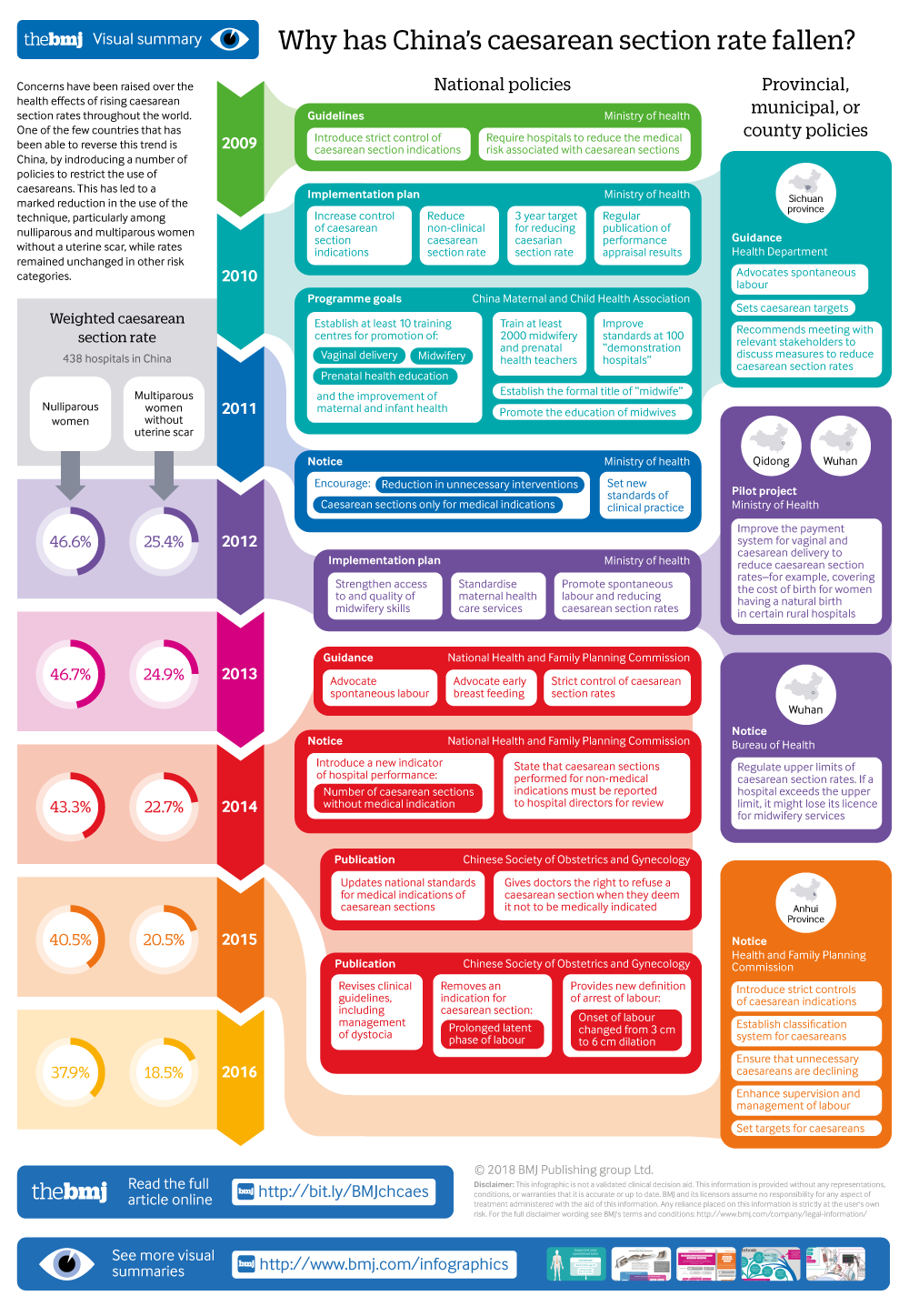
Infographic available
Click here for a visual overview of the falling rate of caesarean sections in China.
- Juan Liang, professor1,
- Yi Mu, research assistant1,
- Xiaohong Li, associate research fellow1,
- Wen Tang, research assistant1,
- Yanping Wang, professor2,
- Zheng Liu, research assistant1,
- Xiaona Huang, maternal and child health specialist3,
- Robert W Scherpbier, chief3,
- Sufang Guo, health specialist4,
- Mingrong Li, research assistant1,
- Li Dai, professor1,
- Kui Deng, research assistant1,
- Changfei Deng, research assistant1,
- Qi Li, research assistant1,
- Leni Kang, research assistant2,
- Jun Zhu, professor1 5,
- Carine Ronsmans, professor6 7
- 1National Office for Maternal and Child Health Surveillance of China, Department of Obstetrics, West China Second University Hospital, Sichuan University, Chengdu, Sichuan, China
- 2National Office for Maternal and Child Health Surveillance of China, Department of Pediatrics, West China Second University Hospital, Sichuan University, Chengdu, Sichuan, China
- 3Health, Nutrition and Water, Sanitation & Hygiene, UNICEF China, Beijing, China
- 4UNICEF Regional Office for South Asia, Kathmandu, Nepal
- 5Key Laboratory of Birth Defects and Related Diseases of Women and Children (Sichuan University), Ministry of Education, Chengdu, Sichuan, China
- 6West China School of Public Health, Sichuan University, Chengdu, Sichuan, China
- 7Department of Infectious Disease Epidemiology, London School of Hygiene & Tropical Medicine, London, UK
- Correspondence to: C Ronsmans, London School of Hygiene & Tropical Medicine, London WC1E 7HT, UK Carine.Ronsmans{at}lshtm.ac.uk
- Accepted 1 February 2018
Abstract
Objective To examine how the relaxation of the one child policy and policies to reduce caesarean section rates might have affected trends over time in caesarean section rates and perinatal and pregnancy related mortality in China.
Design Observational study.
Setting China’s National Maternal Near Miss Surveillance System (NMNMSS).
Participants 6 838 582 births at 28 completed weeks or more of gestation or birth weight ≥1000 g in 438 hospitals in the NMNMSS between 2012 and 2016.
Main outcome measures Obstetric risk was defined using a modified Robson classification. The main outcome measures were changes in parity and age distributions and relative frequency of each Robson group, crude and adjusted trends over time in caesarean section rates within each risk category (using Poisson regression with a robust variance estimator), and trends in perinatal and pregnancy related mortality over time.
Results Caesarean section rates declined steadily between 2012 and 2016 (crude relative risk 0.91, 95% confidence interval 0.89 to 0.93), reaching an overall hospital based rate of 41.1% in 2016. The relaxation of the one child policy was associated with an increase in the proportion of multiparous births (from 34.1% in 2012 to 46.7% in 2016), and births in women with a uterine scar nearly doubled (from 9.8% to 17.7% of all births). Taking account of these changes, the decline in caesarean sections was amplified over time (adjusted relative risk 0.82, 95% confidence interval 0.81 to 0.84). Caesarean sections declined noticeably in nulliparous women (0.75, 0.73 to 0.77) but also declined in multiparous women without a uterine scar (0.65, 0.62 to 0.77). The decrease in caesarean section rates was most pronounced in hospitals with the highest rates in 2012, consistent with the government’s policy of targeting hospitals with the highest rates. Perinatal mortality declined from 10.1 to 7.2 per 1000 births over the same period (0.87, 0.83 to 0.91), and there was no change in pregnancy related mortality over time.
Conclusions China is the only country that has succeeded in reverting the rising trends in caesarean sections. China’s success is remarkable given that the changes in obstetric risk associated with the relaxation of the one child policy would have led to an increase in the need for caesarean sections. China’s experience suggests that change is possible when strategies are comprehensive and deal with the system level factors that underpin overuse as well as the various incentives at work during a clinical encounter.
Introduction
China has made remarkable progress in achieving the Millennium Development Goals, but its success has come at a cost.123 While nearly all women now deliver in hospital, many do so by caesarean section, and many caesarean sections are thought not to be medically indicated.4567 In 2008, 29% of births in China were by caesarean section, increasing to 35% by 2014.8 National averages hide huge variation however: in 2014 the caesarean section rate was as high as 62% in the north eastern province of Jilin, while it was only 4% in Tibet.8
Overuse of caesarean section adversely affects the health of the mother and the child,910 although evidence from China is limited.4 Caesarean sections in China have been associated with childhood obesity11 and postpartum depression,12 but evidence that caesarean sections are associated with adverse psychological development in children is unconvincing.13 A large study in Shanghai found no difference in the frequency of severe maternal complications in women who underwent caesarean delivery on maternal request compared with women who tried vaginal delivery.14
The reasons underlying the high caesarean section rates in China are complex, with both demand and supply side factors driving the rate.4715 Women may request a caesarean section because they fear the consequences of vaginal delivery or they think a caesarean section is safer.516 Perverse financial incentives that encourage costly procedures have certainly been important, as have medicolegal concerns.17 Total expenditure on caesarean section has increased noticeably and the procedure has become an important source of revenue for hospitals and healthcare providers.1618 The increased funding available through insurance schemes may also have boosted demand, although evidence that health insurance has encouraged caesarean section is weak.2619 The facility based doctor led model of maternal healthcare where women give birth in large hospitals replete with advanced technology and costly interventions might also have contributed to the high rates.31520
In the past 10 years, the Chinese government has become increasingly concerned about rising caesarean section rates, and various policies and programmes have been put in place at central, provincial, district, county, and hospital levels.8212223 Concerns about increasing caesarean section rates intensified particularly from 2010 onwards after the publication of a report that showed China had one of the highest caesarean section rates in the world.24 Appendix table 1 shows examples of specific policies. Interventions include hands-on training for doctors and midwives, the revision of guidelines for the management of dystocia, education of women on the advantages of natural birth and the risk of caesarean delivery, audits of caesarean sections without indications, removing financial incentives for caesarean sections, setting targets for a maximum caesarean section rate, and linking the success in reaching targets to financial and other incentives.8212225 Although overall caesarean section rates continued to increase until 2014, the speed of change slowed and rates started to decline in large urban areas and in areas with very high caesarean section rates in 2008.82122 In Beijing, the caesarean section rate declined from 60% in 2009 to 43% in 2014. Similar figures for Shanghai are 67% and 52%, respectively.8
As China relaxed its one child policy in November 2013,26 and many Chinese couples are now allowed and encouraged to have a second child, the careful monitoring of caesarean sections becomes more urgent. As the number of repeat caesarean sections increase, the risk to benefit ratio of a caesarean section may well change.2728 Evidence on how the changes in the one child policy have affected the obstetric risk distribution of women giving birth is, however, lacking. If obstetric risk changes, the need for caesarean sections might change, caesarean sections might become less safe, and perinatal and pregnancy related mortality might increase.
We examined how the relaxation of the one child policy and policies to reduce caesarean sections might have affected trends in caesarean section rates and perinatal and pregnancy related mortality rates in hospitals in China between 2012 and 2016. We take account of the effects of the relaxation of the one child policy by adjusting all time trends for changes in the obstetric profile of women, including age and parity, and by reporting trends in nulliparous and multiparous women separately.
Methods
Data sources
We used three data sources: individual level data collected through China’s National Maternal Near Miss Surveillance System (NMNMSS) covering births in hospital between 1 January 2012 and 31 December 2016; institutional data collected from each hospital through the NMNMSS in 2015; and a survey conducted in 2016 inquiring about policies that may have influenced caesarean section rates in the sampled hospitals.
The NMNMSS covers 441 hospitals at county level or above; however, we excluded three hospitals who did not report any data after 2012. The sampling strategy has been detailed elsewhere.29 In 2010 the NMNMSS sampled 273 urban districts and rural counties randomly from the National Maternal and Child Mortality Surveillance System (fig 1). At the same time 53 counties and districts that were part of the provincial Maternal and Child Mortality Surveillance System were added to ensure proportional representation of urban and rural populations across all three regions in China. Within each of the sampled districts or counties, two health facilities with more than 1000 deliveries each year were randomly selected (or one facility if only one was available). Because some districts or counties did not have hospitals with the necessary number of births, large hospitals in urban districts were oversampled. As a result, urban populations were over-represented in the NMNMSS, particularly in central and western regions. Within each hospital, sociodemographic and obstetric information were collected prospectively on all pregnant or postpartum women admitted to the obstetric department. Doctors responsible for patient care collected data, which included the date of delivery, the number of antenatal visits, maternal education and marital status, maternal age, birth order, gestational age at delivery (based on date of last menstrual period or ultrasonography findings), mode of delivery, presentation of the fetus, single or multiple pregnancy, maternal complications (at any time during hospital admission), and the birth weight of the baby.
Map of sites in National Maternal Near Miss Surveillance System in mainland China, 2012-16
In 2015 the NMNMSS collected standard data on each hospital, including whether the hospital was located in an urban district or a rural county, the level of the hospital (levels 1-3 based on the number of beds (level 3 hospitals have more beds than level 1 and 2 hospitals), categories of clinical departments, numbers of medical staff, type and quantity of equipment, and hospital funding),30 and the number of obstetricians.
In 2016, we conducted a survey of caesarean section policies in all the surveillance hospitals. Through this survey we documented policies established by the national or local health administrative department or the administrative department of the hospital, which aimed to reduce the caesarean section rates in the hospital. The survey was conducted during the national training of NMNMSS staff in October 2016, which brings together all staff responsible for the surveillance work in the hospitals. The structured survey questionnaire included information on whether the hospitals had any policy to reduce the caesarean section rate, including whether the hospitals had a list of medical indications for caesarean sections and whether the hospitals had an upper target for the caesarean section rate.
Definition of variables
We used commonly used definitions for maternal age, marital status, and education.29 We classified maternal complications into mutually exclusive categories of direct obstetric complications and medical diseases. Direct obstetric complications included uterine rupture, placenta praevia, abruptio placentae, unspecified antepartum haemorrhage, pre-eclampsia, eclampsia, HELLP syndrome, or any fetal malpresentation (breech, shoulder, or other). Medical diseases included heart disease, embolism/thrombophlebitis, hepatic disease, severe anaemia (haemoglobin <70 g/L), renal disease (including urinary tract infection), lung disease (including upper respiratory tract infection), HIV/AIDS, connective tissue disorders, gestational diabetes mellitus, and cancer.
We categorised women into risk groups for caesarean section using a modified version of the Robson classification.3132 Because there is no agreement on the optimal caesarean section rate in the population, and indications for caesarean sections are not standardised, Robson proposed a system that classifies women into 10 groups based on their obstetric characteristics (parity, previous caesarean section, gestational age, onset of labour, fetal presentation, and number of fetuses).31 The size of each group and the caesarean section rate within each group correspond to an expected range. Monitoring caesarean sections within the Robson groups therefore allows the evaluation of clinical practice, including whether the caesarean section rate is justified. We adapted Robson’s classification because the NMNMSS did not collect information on whether or not the labour was induced. We created eight mutually exclusive categories: nulliparous, singleton, cephalic, ≥37 weeks’ gestation; multiparous, singleton, cephalic, ≥37 weeks’ gestation without a uterine scar; uterine scar, singleton, cephalic, ≥37 weeks’ gestation; all nulliparous women with a singleton breech; all multiparous women with a singleton breech, including those with a uterine scar; all multiple pregnancies, including those with uterine scar; all women with a single pregnancy in other abnormal lie, including those with uterine scar; and all singleton, cephalic, ≤36 weeks’ gestation pregnancies, including those with uterine scar.
For the institutional data we calculated the number of obstetricians per 1000 births using the number of births reported in the NMNMSS in 2015. We also report the region in which the hospital is located, using China’s standard definitions for region (western, central, and eastern).33 We extracted the day of the week from the date of delivery.
We report the number of perinatal deaths (stillbirths and early neonatal deaths within seven days of delivery before discharge), pregnancy related deaths, and uterine rupture. Stillbirths were defined as reported previously.29 Pregnancy related deaths were defined as deaths from any cause in women who died after 28 completed weeks of gestation or with a fetus of birth weight 1000 g or higher (including women who died undelivered). Uterine rupture was defined as uterine or lower uterine dehiscence in late pregnancy or during childbirth, including complete and incomplete rupture.34
Statistical analysis
We restricted the analysis to women who delivered at or after 28 completed weeks of gestation or with a fetus of birth weight 1000 g or higher, consistent with the definition of the perinatal period in China.35 Since the NMNMSS oversampled large urban hospitals, we weighed the caesarean section rate for the sampling distribution of the population according to the 2010 census of China, as detailed elsewhere.29 We used Poisson regression with a robust variance estimator in STATA version 13.1 to examine the strength of association between institutional and women’s characteristics and the proportion of caesarean sections, reporting the findings from three models. Model 1 describes the crude relative risk and 95% confidence intervals, taking account of the NMNMSS sampling strategy and clustering of births within hospitals.36 Model 2 adjusts the effect estimates described in model 1 for institutional (region, hospital level, number of obstetricians per 1000 births, day of the week) and individual socioeconomic characteristics (number of antenatal visits, education, marital status). In model 3, we further adjust the relative risks for individual demographic and clinical factors that are known to be associated with caesarean sections and that might have changed after the relaxation of the one child policy: maternal age, Robson classification, maternal complications, and birth weight. We did not adjust for parity separately because such adjustment is built into the Robson classification. To identify the most robust and stable model we investigated both multicollinearity and model goodness-of-fit.
To examine whether trends over time in caesarean sections were similar within maternal age groups, in nulliparous and multiparous women, in each Robson group, and by the caesarean section rate in the hospital in 2012, we repeated models 1 and 3 testing for an interaction between year and each of these exposures. We obtained the P value for the interaction terms by comparing models with and without interaction terms using a likelihood ratio test. We also report changes in the age, parity, and Robson distributions of women over time.
To examine trends over time in perinatal and pregnancy related mortality we repeated models 1 and 3 against these outcomes, restricting the sample to singleton births for perinatal deaths and to all births for pregnancy related deaths. We repeated the analysis in nulliparous and multiparous women separately, adding an interaction term. We also report the incidence of uterine rupture over time among nulliparous, multiparous women with a uterine scar, and multiparous women without a uterine scar, using models 1 and 3 (but removing the Robson classification and complications from the model).
Lastly, we describe the proportion of hospitals reporting a policy to reduce caesarean section rates, including whether or not a target has been set for caesarean section or whether clinical indications for caesarean sections have been defined. We also report the median cost of caesarean sections and vaginal deliveries.
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design or implementation of the study. No patients were asked to advise on interpretation or writing up of results. There are no plans to disseminate the results of the research to study participants or the relevant patient community.
Results
Changes over time in the obstetric risk population
Between 2012 and 2016 there were 6 838 582 deliveries at 28 completed weeks or more of gestation or with a fetus of birth weight 1000 g or more in 438 hospitals in the NMNMSS. Substantial changes occurred over time in the age and parity distributions of the women, the proportion of women with a uterine scar, and the proportion of women in each modified Robson group (table 1). The proportion of births to women aged 35 or more increased from 7.8% in 2012 to 10.9% in 2016 (table 1). More importantly, the proportion of births of birth order two or more increased from 34.1% in 2012 to 46.7% in 2016, and the proportion of women with a uterine scar nearly doubled, from 9.8% to 17.7% (table 1). Correspondingly, the greatest change in individual Robson groups was in the proportion of women with a uterine scar and a singleton birth at term (from 8.6% to 15.6%).
Changes over time in age and parity distributions of women and modified Robson categories (438 hospitals in China in 2012-16). Values are numbers (percentages) unless stated otherwise
Determinants of caesarean sections
Three million (3 078 101) women delivered by caesarean section, giving a weighted caesarean section rate of 43.5%. Caesarean section rates were higher in hospitals located in urban areas than in rural areas (see appendix table 2). Level 3 referral hospitals did more caesarean sections than lower level hospitals, but this was fully explained by the varying sociodemographic and obstetric characteristics of the women seeking care in these hospitals (adjusted relative risk comparing level 3 and level 2 hospitals 1.04, 95% confidence interval 0.98 to 1.10). Hospitals with six or more obstetricians per 1000 births had the highest caesarean section rates, and this effect persisted after adjustment for the level of hospital and the sociodemographic and obstetric profile of the women (adjusted relative risk comparing hospitals with ≥6 obstetricians per 1000 births with hospitals with <4 obstetricians per 1000 births 1.15, 1.08 to 1.23). Caesarean sections were less common on Sundays (adjusted relative risk 0.89, 0.88 to 0.91) and Saturdays (0.93, 0.92 to 0.95) compared with Wednesdays. The lowest caesarean section rates were among women with few antenatal visits (caesarean rate 35.8%), those with no education (35.2%), and unmarried women (28.8%).
Caesarean section rates increased noticeably with maternal age. The caesarean section rate in women younger than 20 was 27.5% (crude relative risk compared with women aged 25-29 0.64, 95% confidence interval 0.61 to 0.68) whereas the rate in women aged 40 or older was 60.7% (1.42, 1.38 to 1.45). These differences persisted after adjustment for institutional, sociodemographic, and obstetric factors. As expected, caesarean section rates were high in women with direct obstetric complications (83.1%) or medical diseases (51.2%), but they were also high (40.1%) among women in whom the hospital record noted no such complications. The caesarean section rate was lowest among multiparous women without a uterine scar with a singleton cephalic birth at term (19.5%), and highest among women with a uterine scar who had a singleton cephalic birth at term (91.2%).
Trends over time in caesarean section rates
The caesarean section rate declined from 45.3% in 2012 to 41.1% in 2016 (crude relative risk 0.91, 95% confidence interval 0.89 to 0.93; table 2). Adjusting the time trends for institutional, sociodemographic, and obstetric characteristics reduced the relative risk to 0.82 (0.81 to 0.84), suggesting that caesarean section rates declined by 18% between 2012 and 2016.
Time trends in caesarean section rates in all women and by parity (438 hospitals in China in 2012-16)
Table 2 and appendix table 3 show the trends over time in caesarean section rates within parity and age groups. Crude caesarean section rates declined in nulliparous women (crude relative risk 0.81, 0.79 to 0.84) and in multiparous women without a uterine scar (0.73, 0.70 to 0.76; interaction parity and year, P=0.00; table 2). Adjustment for sociodemographic and obstetric factors further strengthened the relative risk. Caesarean section rates declined in all age groups, although the speed of decline was greater in younger women than in older women (interaction age and year, P=0.00; see appendix table 3).
Table 3 shows trends over time in caesarean section rates in each modified Robson group. Caesarean section rates declined substantially in two groups: nulliparous women with a singleton, cephalic birth at ≥37 weeks of gestation (from 45.0% to 35.2%, adjusted relative risk 0.75, 95% confidence interval 0.73 to 0.77) and multiparous women without a uterine scar and a single cephalic birth at term (from 22.9% to 15.6%, 0.65, 0.62 to 0.68), Women in other Robson groups did not experience such declines (interaction Robson groups and year, P=0.00).
Time trends in caesarean section rates in each Robson group (438 hospitals in China in 2012-16)
Caesarean section rates declined particularly in women giving birth in hospitals with high caesarean section rates in 2012 (table 4). For example, in hospitals with a caesarean section rate of 60% or more in 2012 rates decreased from 68.8% in 2012 to 56.8% in 2016 (adjusted relative risk 0.78, 0.75 to 0.81). In hospitals with moderately high caesarean section rates (baseline rates of 20-39%), however, the rates remained stable over time, although adjustment for sociodemographic and obstetric factors resulted in an adjusted relative risk of 0.90 (0.87 to 0.93). In hospitals with relatively low caesarean section rates in 2012 rates continued to increase over time (1.17, 1.04 to 1.31); interaction baseline caesarean section rate and year P=0.00).
Time trends in caesarean section rates by caesarean section rate in hospital in 2012 (438 hospitals in China in 2012-16)
Trends over time in perinatal and maternal outcomes
Perinatal mortality declined substantially (table 5), from 10.1 per 1000 births in 2012 to 7.2 per 1000 births in 2016 (crude relative risk 0.72, 95% confidence interval 0.67 to 0.77). These trends persisted after adjustment for sociodemographic and obstetric factors (adjusted relative risk 0.87, 0.83 to 0.91). Perinatal mortality declined at the same rate in nulliparous and multiparous women (interaction parity and year P=0.48). There was no change in pregnancy related mortality over time (from 7.7 per 100 000 in 2012 to 7.1 per 100 000 in 2016, crude relative risk 0.91, 0.64 to 1.30; table 6).
Time trends in perinatal mortality rates in all births and by parity (438 hospitals in China in 2012-16)
Time trends in pregnancy related mortality rates by parity (438 hospitals in China in 2012-16)
Table 7 shows trends in the incidence of uterine rupture. The incidence of uterine rupture was much higher in women with a uterine scar than in those without a scar. Among women with a uterine scar the incidence of uterine rupture increased steadily, from 28.4 per 10 000 births in 2012 to 87.3 per 10 000 births in 2106 (adjusted relative risk 2.83, 95% confidence interval 1.89 to 4.23). Among nulliparous women, there was an increase in the incidence of uterine rupture between 2012 and 2013, but rates remained relatively stable thereafter.
Time trends in incidence of uterine rupture by parity and presence of uterine scar (438 hospitals in China in 2012-16)
Survey on policies to reduce caesarean section rates
Overall, 398 (90.9%) hospitals completed the survey on policies potentially influencing caesarean section rates (see appendix table 4). The cost of caesarean sections (median ¥5000; £562; $788; €635) was twice as high as the cost of vaginal deliveries (median ¥2500). Nearly all (92.7%) hospitals reported that they had a policy to reduce caesarean sections, two thirds (67.1%) had set a target caesarean section rate, and nearly all reported that they had a list of clinical indications for caesarean sections (93.0%), trained health providers in the use of caesarean sections (86.9%), or offered health education to women (95.0%).
Discussion
Using data from more than six million births in 438 large hospitals in China, we found that caesarean section rates declined steadily between 2012 and 2016 (crude relative risk 0.91, 95% confidence interval 0.89 to 0.93), reaching an overall hospital based rate of 41.1% in 2016. The relaxation of the one child policy in China led to an increase in the proportion of multiparous births (from 34.1% in 2012 to 46.7% in 2016), and births in women with a uterine scar nearly doubled (from 9.8% to 17.7% of all births). Taking account of these changes amplified the decline in caesarean sections over time (adjusted relative risk 0.82, 95% confidence interval 0.81 to 0.84), suggesting that caesarean sections declined by 18% between 2012 and 2016. The fall in caesarean section rates was most pronounced in hospitals with the highest rates in 2012, consistent with the Chinese government’s policy of targeting such hospitals. Perinatal mortality declined from 10.1 to 7.2 per 1000 births over the same period (adjusted relative risk 0.87, 0.83 to 0.91), and there was no change in pregnancy related mortality over time.
Comparison with other studies
The relaxation of the one child policy in November 2013 and the introduction of the two child policy in October 201526 has led to more families having a second child.37 In our data, the proportion of multiparous births increased from about a third of all births (34.1%) in 2012 to nearly half of all births (46.7%) in 2016. Multiparous births are highly heterogeneous, however, and associated risks vary—particularly whether or not the woman has a uterine scar. While multiparous births without a uterine scar increased from 24.2% to 28.9% of all births between 2012 and 2016, the contribution of those with a uterine scar nearly doubled (from 9.8% to 17.7% of all births). These proportions are consistent with those found in the World Health Organization facility based surveys in China in 2007-08 and 2010-11.32
The caesarean section rates reported here are similar to those described by WHO in 2008 and 2010 in a sample of large hospitals in China,2432 but are higher than the rates obtained from population based sources. The 2009-2011 National Health Service Survey reported a rate of 36.3% in 2011,19 and the 2013 National Health Service Survey reported a rate of 40.9% in 2013 (unpublished), whereas the National Maternal and Child Health Statistics office published a rate of 34.9% for 2014.8 The NMNMSS oversampled large referral hospitals in urban districts, where caesarean section rates were higher than those in smaller hospitals. Weighing the data by the population distribution in urban districts and rural counties in each region accounted for the NMNMSS’s oversampling of urban districts, but whether this adjusted fully for the oversampling of large hospitals is not known.
Findings of this study
China is the only country that has succeeded in reverting the rising trends in caesarean sections.3238 In a review of global trends in caesarean sections between 1990 and 2014, one study found only two countries—Guinea and Nigeria—where the caesarean section rate decreased, but these were countries with extremely low caesarean section rates. In countries with excessively high caesarean section rates, such as Brazil and the Dominican Republic, caesarean section rates have grown steadily, to reach 56% in 2013.38 China’s success is even more remarkable, since the decrease in caesarean sections is most pronounced in women less in need of a caesarean section (eg, nulliparous and multiparous singleton cephalic births at term without a uterine scar), while the rates remained unchanged among those clinically needing a caesarean section.
A key question is whether the decline in caesarean section rates is due to the decision by the Chinese government to change its one child policy or to the introduction of policies specifically aimed at reversing the high caesarean section rate. The demographic changes brought about by the one child policy—for example, more women giving birth at older ages or with a uterine scar—would have led to an increase rather than a decline in caesarean section rates. Indeed, adjusting the time trends in caesarean section rates for the changes associated with the one child policy amplified the time trends, suggesting that the downward trend in caesarean section rates happened regardless of the relaxation of the one child policy. Whether the decline in caesarean section rates among nulliparous women can be explained, at least in part, by changes in the assessment of the risk to benefit ratio of a caesarean section now that more women can have another pregnancy, is uncertain. Knowledge that more women can have a subsequent pregnancy, where the risks of a caesarean section are greater, may well lead some clinicians and women to opt for a vaginal delivery in the woman’s first pregnancy. However, the greatest decline in caesarean sections was observed among multiparous women without a uterine scar, a group in which the relaxation of the one child policy is unlikely to have had an impact. Most women who are pregnant for the first time may not know whether they want another child, and it is unlikely that changes in the number of children that women are planning to have will change their or their clinician’s decision making around the first delivery.
Longer time trends in caesarean section rates may further elucidate the contribution of the relaxation of the one child policy to the decrease in caesarean section rates in China. Three studies have reported on national caesarean section rates over time in China.81519 Feng and colleagues,15 using data from four nationally representative surveys between 1993 and 2008, reported increasing rates in urban and rural areas in nulliparous and multiparous women between 1993 and 2008. Meng et al,19 using the same survey data for 2003 and 2008 but adding a new nationally representative survey in 2011 reported continually increasing rates in rural areas between 2008 and 2011 (from 25.0% to 33.3%). However, for the first time, the authors reported decreasing caesarean section rates in urban areas (from 53.3% in 2008 to 46.8% in 2011). Lastly, Li et al,8 using national report data from all counties in China between 2008 and 2014 reported increasing caesarean section rates overall (from 28.8% to 34.9%) but declining rates in large cities and counties that had high rates in 2008. In the largest cities, caesarean section rates declined steadily from 53% in 2009/10 to 47% in 2014; in areas with high caesarean section rates in 2008 the decline was similar (from 60% in 2009 to 53% in 2014). Unfortunately, neither Meng et al19 nor Li et al8 report data by parity, but a comparison of our data with the data from the WHO surveys in 2007/08 and 2010/11 suggests that the decline may have started before 2010/11.32 This suggests that caesarean section rates in China started declining a few years before the relaxation of the one child policy.
The timing of the decline in caesarean sections coincides with the Chinese government’s explicitly stated concern about the risks associated with caesarean sections and its introduction of several policies to deal with the high caesarean section rates (see appendix table 1). China’s approach to reducing caesarean sections has been largely top-down, with national or local government and obstetric societies setting caesarean section targets and introducing financial and other incentives when targets are reached, or penalties when targets are exceeded. The number of caesarean sections without medical indication are now used as an indicator to assess the performance of hospitals, including whether the hospital qualifies as a baby friendly hospital, and caesareans performed for non-medical indications need to be reported to the hospital director for review.25 Some hospitals have also taken initiatives themselves, including health education for pregnant women.821 In a tertiary centre in Shanghai, for example, the local government set caesarean section targets and introduced a fixed reimbursement rate regardless of mode of delivery.21 At the same time the hospital introduced a multifaceted intervention, including antenatal classes informing women about the benefits of vaginal delivery, pain relief for vaginal delivery, and a bonus to individual providers whose caesarean section rates are low. As a result, caesarean sections in the hospital declined from 51% to 43% over a four year period. In our study, many hospitals (78%) reported that a caesarean section target had been set and most (93%) had clinical guidelines on indications for caesarean sections. The costs of caesarean sections remained much higher than the costs of vaginal deliveries, however, and few hospitals had introduced a fixed reimbursement rate regardless of mode of delivery.
Other measures to support the reduction in caesarean sections include a revision of clinical guidelines for the management of labour, training in the use of forceps and vacuum extraction, and the training and deployment of midwives. First, in 2014, the Association of Gynaecologists and Obstetricians in China issued an “expert consensus on caesarean sections,” which gave doctors the right to refuse a caesarean section on request when they deemed it not to be medically indicated.39 If women persisted in their request for a caesarean section their case was referred to the head of the obstetric department for review. Second, revisions to clinical guidelines introduced changes to some dystocia related indications for caesarean sections. A prolonged latent phase of labour, previously an indication for caesarean section, was removed from the list of indications, and a new definition of arrest of labour, shifting the onset of labour from 3 cm to 6 cm dilation, was introduced.40 Third, training on the use of the partograph, forceps delivery, and vacuum extraction was reinforced across the country. Fourth, in an effort to reduce the workload of obstetricians, the Chinese government introduced a new training curriculum for midwives in 2012. By 2014, eight regional training centres were providing midwifery training, and most high level referral hospitals now have a cadre of midwives to manage labour and delivery.
Repeat caesarean birth is associated with an increase in the risk of placenta praevia or placenta accreta, infection, damage to the bladder and bowel, deep vein thrombosis, and, on rare occasions, uterine rupture.2728 Evidence to date suggests that in women with a uterine scar, a planned caesarean or a planned vaginal birth carries similar risks to the mother and baby, but the evidence is observational and bias cannot be excluded.27 In China, repeat caesarean section is the preferred mode of delivery for women with a uterine scar, and opinions on whether more women should undergo a trial of labour vary.4142 Caesarean section rates remained high among women with a uterine scar, and vaginal birth after caesarean section was uncommon. The dramatic increase in the incidence of uterine rupture among women with a uterine scar is potentially worrying, although some of these ruptures may have been a dehiscence with no major clinical consequence. We were unable to investigate the reasons for this increase, but policy makers, clinicians, and researchers across China will need to give urgent attention to how obstetric services cope with the added stress of an increasing number of women with a uterine scar.
Perinatal mortality rates declined over the study period, while pregnancy related mortality remained unchanged, consistent with findings from Beijing, Tianjin, and Zhejiang.84344 Declining trends in perinatal mortality persisted after adjustment for sociodemographic factors, including parity, suggesting that changes over time in the characteristics of the obstetric population did not explain the findings. We did not examine trends in adverse neonatal outcomes such as birth trauma or respiratory distress, but in a large tertiary hospital in Shanghai the noticeable decline in caesarean sections was not associated with changes in such outcomes, although the frequency of neonatal infection increased slightly.21 Caesarean sections remained unchanged among high risk births such as twin or breech deliveries and those with abnormal lie, thereby protecting the most vulnerable infants. In addition, the Chinese government has introduced several strategies that might have contributed to a reduction in perinatal mortality, including a greater number of focused antenatal visits, a system of supervision between tertiary and lower level hospitals, the introduction of neonatal intensive care units in county hospitals, and specific training in neonatal care and resuscitation.34546
Strengths and limitations of this study
The NMNMSS is a well established surveillance system with rigorous quality controls,2947 but data and analytical limitations need to be acknowledged. Firstly, this is not an intervention study and it is not possible to attribute the decline in caesarean sections to one particular policy. However, the timing of the decline and the faster decline in caesarean sections in hospitals with the highest baseline rates are consistent with the government’s policy of targeting hospitals with the highest caesarean section rates. By using a statistical model that adjusted for the main demographic and clinical changes potentially associated with the relaxation of the one child policy (including maternal age, Robson classification, maternal complications, and birth weight), we were able to separate the effects of the relaxation of the one child policy from policies specifically aimed at reversing the high caesarean section rate. Secondly, the accuracy of the caesarean section rates over time need careful scrutiny, particularly when the reporting of lower rates can generate positive incentives. The NMNMSS was designed to enumerate maternal deaths and near-miss rather than caesarean sections, however, and those filling out the form for each woman did not know that the mode of delivery would become a focus of investigation. Given that data were collected on individual women, it would have been extremely difficult to manipulate data so that aggregate rates would show declining trends over time. Thirdly, data were only collected in obstetric departments, and babies at high risk of dying who were admitted to a paediatric intensive care unit will have been missed. The early neonatal mortality rate was surprisingly low, although it was consistent with that found in other studies.48 While early neonatal mortality rates in the NMNMSS may be biased downward, there is no reason for this to have changed over time. Fourthly, the Robson classification has been recommended as the most appropriate to compare caesarean section rates,3249 but we were unable to separate women who had spontaneous labour from those who delivered after induction or had a caesarean section before labour, a critical element in understanding caesarean section rates. In the WHO surveys in 2007-08 and 2010-11, caesarean sections fell among single nulliparous births where the labour was induced or the caesarean section was done before labour.32 Lastly, the definition of complications relied on the provider’s clinical diagnosis, which may be prone to bias. In particular, the ascertainment of uterine rupture in the presence of a scar may be variable. Since the data do not discriminate between an asymptomatic dehiscence that may present at the time of a repeat elective caesarean section and that of uterine rupture which presents as an emergency during labour, the clinical relevance of the findings is uncertain. Although the incidence of uterine rupture reported here among women with a uterine scar is similar to that noted in many other studies,50 trends over time have to be interpreted with caution.
Conclusion and policy implications
Rigorous evidence of which strategies contribute to reductions in caesarean sections is limited, and interventions that have been shown to work, such as the implementation of guidelines with mandatory second opinion and nurse led preparation classes have resulted in relatively small reductions in caesarean section rates.515253 China’s experience suggests that change is possible when strategies address the system level factors that underpin overuse as well as the various incentives at work during a clinical encounter.54 As the two child policy gathers momentum in China, and the proportion of births in women with a uterine scar increases further, conditions will have to be created to maintain the safety of repeat caesarean sections, while strategies to avoid medically unnecessary primary caesarean section need to be continually reinforced.
What is already known on this topic
Concerns have been raised over the health effects of increasing caesarean section rates throughout the world, but so far no country has managed to reverse this trend
Many studies have reported rising caesarean section rates in China, but few have included the period after the relaxation of the one child policy
The Chinese government has introduced several policies to reduce caesarean sections, but it is not known how this has affected caesarean section rates in various obstetric risk categories
What this study adds
The relaxation of the one child policy has resulted in an increased proportion of multiparous births, particularly with a uterine scar, and women giving birth at older ages
Caesarean section rates declined steadily between 2012 and 2016, particularly among nulliparous and multiparous births without a uterine scar, while rates remained unchanged in other risk categories
Perinatal mortality declined from 10.1 per 1000 births to 7.2 per 1000 births over the same period, and pregnancy related mortality did not change
Acknowledgments
We thank the institutions and staff of the National Maternal Near Miss Surveillance System for data collection.
Footnotes
Contributors: JL and YM are joint first authors. JZ (zhujun028@163.com) and CR contributed equally to the correspondence work. JL, YM, JZ, and CR designed the study with contribution from all authors. YM and WT did the statistical analysis with support from XL and CR. CR wrote the first draft of the paper and all authors contributed to critical interpretation of the results and development of the report. All authors saw and approved the final version. JZ and CR are guarantors.
Funding: This study was supported by the National Health and Family Planning Commission of the People’s Republic of China, the National Natural Science Foundation of China (grant No 81330016), the China Medical Board (grant No 11-065), WHO (grant No: CHN-12-MCN-004888), UNICEF (grant No 2016EJH016), and the National “Twelfth Five-Year” Plan for Science and Technology Support (2014BAI06B01).
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study was approved by the ethics committee of the West China Second University Hospital (protocol ID, 2012008).
Data sharing: No additional data available.
Transparency: The lead authors (JZ and CR) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.

