Abstract
Objective
The authors aim to determine whether pediatric residents used DSM-IV criteria to diagnose major depressive disorder and how this related to residents’ confidence in diagnosis and treatment skills before and after clinical training with depressed adolescents.
Methods
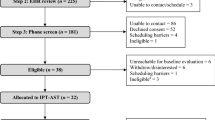
Pediatric residents evaluated two different standardized patients portraying major depressive disorder before and after learning about adolescent depression. Residents’ interactions with standardized patients were observed, and checklists containing DSM-IV criteria for major depressive disorder and other pertinent information, such as comorbidities, were completed for each interaction. After the encounter, residents completed a survey asking about the “patient’s” diagnosis and the residents’ confidence in their clinical skills.
Results
Residents assessed significantly more checklist items in the second encounter with a standardized patient. Residents’ confidence in treatment was significantly higher after the rotation, while confidence in diagnostic skills was unchanged, remaining high. Even after the rotation, residents did not use all DSM-IV criteria for major depressive disorder in their diagnoses.
Conclusion
Major depressive disorder is a common adolescent psychiatric disorder. Pediatricians must be equipped with appropriate interpersonal and diagnostic skills to detect this and other psychiatric disorders. Standardized patients represent one useful way to teach and assess these skills. This study suggests that residents’ interpersonal and diagnostic skills can improve with practice. Although resident scores improved, post-encounter checklists showed that residents were still not asking all the necessary questions for a DSM-IV diagnosis, concluding prematurely that the standardized patients had major depressive disorder before satisfying all diagnostic criteria. The majority did not consider other depressive conditions or comorbid disorders.
Similar content being viewed by others
References
Lubell KM, Kegler SR, Crosby AE, et al: Suicide trends among youths and young adults aged 10–24 years, United States, 1990–2004. MMWR Morb Mortal Wkly Rep 2007; 56: 905–908
Fleischmann A, Bertolote JM, Belfer M, et al: Completed suicide and psychiatric diagnoses in young people: a critical examination of the evidence. Am J Orthopsychiatry 2005; 75: 676–683
Shaffer D, Gould MS, Fisher P, et al: Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry 1996; 53: 339–348
Kessler RC, Berglund P, Demler O, et al: Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62: 593–602
Koppelman J: Children with mental disorders: making sense of their needs and the systems that help them. NHPF Issue Brief 2004; 4: 1–24
Sudak D, Roy A, Sudak H, et al: Deficiencies in suicide training in primary care specialties: a survey of training directors. Acad Psychiatry 2007; 31: 345–349
Olson AL, Kelleher KJ, Kemper KJ, et al: Primary care pediatricians’ roles and perceived responsibilities in the identification and management of depression in children and adolescents. Ambul Pediatr 2001; 1: 91–98
Gardner W, Kelleher KJ, Pajer KA, et al: Primary care clinicians’ use of standardized psychiatric diagnoses. Child Care Health Dev 2004; 30: 401–412
Barzansky B, Etzel SI: Educational programs in US medical schools, 2003–2004. JAMA 2004; 292: 1025–1031
United States Medical Licensing Examining: USMLE Bulletin Examination Content, 2007. Available at www.usmle.org/Examinations/step2/step2cs_content.html
Carney PA, Dietrich AJ, Eliassen MS, et al: Recognizing and managing depression in primary care: a standardized patient study. J Fam Pract 1999; 48: 965–972
Gerrity M, Cole SA, Dietrich AJ, et al: Improving the recognition and management of depression: is there a role for physician education? J Fam Pract 1999; 48: 949–957
Spitzer RL, Gibbon M, Skodol AE, et al: DSM-IV Case Book. Washington, DC, American Psychiatric Press, 1994
Armstrong TD, Costello EJ: Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol 2002; 70: 1224–1239
Perlis RH: Misdiagnosis of bipolar disorder. Am J Manag Care 2005; 11: S271–274
Learman LA, Gerrity MS, Field DR, et al: Effects of a depression education program on residents’ knowledge, attitudes, and clinical skills. Obstet Gynecol 2003; 101: 167–174
Colliver J, Swartz M: Assessing clinical performance with standardized patients. JAMA 1997; 278: 790–791
Author information
Authors and Affiliations
Corresponding author
Additional information
At the time of submission, the authors declared no competing interests.
Rights and permissions
About this article
Cite this article
Lewy, C., Sells, C.W., Gilhooly, J. et al. Adolescent Depression: Evaluating Pediatric Residents’ Knowledge, Confidence, and Interpersonal Skills Using Standardized Patients. Acad Psychiatry 33, 389–393 (2009). https://doi.org/10.1176/appi.ap.33.5.389
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1176/appi.ap.33.5.389