Abstract
Background
None of the current pleurodesing agents fulfil all the criteria for best pleural sclerosant. Therefore, the search for the ideal agent for chemical pleurodesis still continues. The aim of the present study was to compare the effectiveness of erythromycin, tetracycline, Aerosil™ 200 (hydrophilic fumed amorphous silica), and erythromycin plus Aerosil™ 200 in producing pleurodesis in rats. In the present study, talc was not used as a pleurodesing agent due to an unavailability of its sterile and pure form in Iran.
Methods
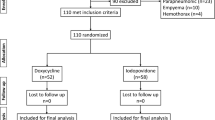
Overall, 75 adult male Spraque-Dawley rats were randomized to 5 treatment groups. Each group received an intrapleural injection via 5 Fr Silastic tubes of one of the following sterile agents: 35mg/kg erythromycin in 2 ml of saline, 35mg/kg tetracycline in 2 ml of saline, 35mg/kg Aerosil™ 200 in 2ml of saline, erythromycin (35mg/kg in 2 ml of saline) plus Aerosil™ 200 (35mg/kg in 2 ml of saline), or 2 ml of saline as a control. The animals were euthanized and necropsied 30 days after injection. The pleurae were assessed for macroscopic and microscopic evidence of surrounding inflammation and fibrosis.
Results
The median macroscopic score in the Aerosil™ 200 group was significantly higher than that in the erythromycin group (P < 0.005). The median microscopic score in the erythromycin group was significantly lower than that in the Aerosil™ 200 and erythromycin plus Aerosil™ 200 groups (P < 0.005). Furthermore, maximum and minimum pleural fibrosis was observed in the erythromycin plus Aerosil™ 200 and erythromycin groups, respectively (P < 0.05).
Conclusion
This study suggests that Aerosil™ 200 with or without erythromycin may be more potent pleurodesis agent than erythromycin and tetracycline.
Similar content being viewed by others
Background
Obliteration of the pleural space (pleurodesis) to prevent recurrent pleural effusion (mostly malignant) or pneumothorax is chiefly achieved through the use of chemical pleural sclerosants [1]. The best pleural sclerosant should be safe, inexpensive, widely available, and easily administered. However, none of the pleurodesing agents including talc, the sclerosant of choice in clinical practice, fulfil all these criteria [1–3]. Intrapleural administration of the most preferred pleurodesing agent, the talc, is believed to accompany with severe complications such as adult respiratory distress syndrome. On the other hand, parenteral tetracycline which was once the sclerosant agent of choice in clinical practice is no longer commercially available [4]. In addition, intrapleural application of some antineoplastic agents such as bleomycin is costly [5]. Therefore, the search for the ideal agent for chemical pleurodesis still continues.
Silica is the common name for silicon dioxide (SiO2). Silica may have a crystalline or a non-crystalline (amorphous) structure. Among synthetic amorphous silicas, pyrogenic (fumed) silica is widely used as reinforcing filler for silicon rubber, thickening and anti-settling agents in liquid systems of coating, adhesives, printing inks and cosmetics [6]. Aerosil™ 200, a hydrophilic fumed silica, is the most widely used form of the amorphous silica. Silica-based materials have been of great interest in chemical pleurodesis. Bioglass, a silica-based biomaterial similar to the Aerosil™ 200, has been found as a pleurodesing agent as effective as talc [7, 8]. The pleurodesing effect of bioglass, talc and Aerosil™ 200 may be attributed to their major content, the silicon dioxide. Interestingly, pulmonary changes following inhalation of Aerosil™ 200 have been reported in the literature [9, 10]. However, pleurodesing effect of Aerosil™ 200 has not been hitherto investigated. Therefore, the aim of the present study was to compare the effectiveness of erythromycin, tetracycline, Aerosil™ 200, and erythromycin plus Aerosil™ 200 in producing pleurodesis in rats compared with saline control. We did not investigate talc as a sclerosing agent in the present study due to an unavailability of its sterile and pure form.
Methods
Adult male Spraque-Dawley rats were used in this study in accordance with the NIH Guide for the Care and Use of Laboratory Animals and local institutional guidelines for humane use of animals in research. The animals were housed three to five per cage and were provided with free access to compact food and water. Their food consisted of all essential ingredients including vitamins and minerals. The animals were kept under constant laboratory conditions with respect to humidity, illumination and temperature before and after surgery [11, 12].
Overall, 75 adult male Spraque-Dawley rats, weighing 220–250 g, were anesthetized with an intramuscular injection of xylazine hydrochloride (5mg/kg) and ketamine hydrochloride (35mg/kg). Under the sterile conditions, a 1-cm incision was made over the seventh rib in the posterior axillary line on the rat’s right side, and a subcutaneous tunnel was extended to the fifth intercostal space. A 5 Fr Silastic tube was inserted through the incision and placed in the right pleural cavity. The rats were randomly assigned to one of five intrapleural treatment groups as follows: fifteen rats received erythromycin ethylsuccinate (35mg/kg) in 2 ml of saline (0.9% NaCl); fifteen animals were given tetracycline (35mg/kg) in 2 ml of saline; fifteen rats were given sterile Aerosil™ 200 (35mg/kg) in 2 ml of saline; fifteen animals received erythromycin ethylsuccinate (35mg/kg in 2 ml of saline) plus sterile Aerosil™ 200 (35mg/kg in 2 ml of saline); and fifteen control animals received 2 ml of normal saline. All the sclerosing agents were given sterile. These agents were instilled into the tube and flushed with air, and the animals were rotated to assure dispersion to the entire pleural surface. The control group received normal saline in a similar approach. All residual air was aspirated from the pleural space. After a perioperative chest radiograph demonstrated a fully expanded lung, the tube was removed, and the incision was closed. All animals were left to heal with both lungs expanded.
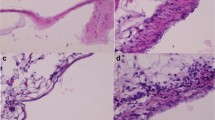
All animals in the experimental and control groups were euthanized on 30th postoperative day by intravenous Beuthanasia-D, a pentobarbital/phenytoin commercial euthanasia solution. The thorax was removed en bloc. Lungs were fully expanded by instilling 10% formalin into trachea. After tracheal injection, the entire thorax was submerged in 10% neutral buffered formalin for 48 hours. Thereafter, a veterinary pathologist, blinded to the treatment group, performed thoracic necropsy. On macroscopic and gross observations, pleurodesis was graded as: 0 = normal pleura, 1 = multifocal fibrosis, 2 = diffuse adhesions and 3 = complete obliteration [2, 13]. For microscopic evaluation, tissue sections from the lung and pleura were prepared and stained with hematoxylin and eosin (HE) and Masson’s trichrome. Light microscopic assessment of the sections was performed by a pathologist blinded to the study protocol. The slides were graded for inflammation/cellularity and scored using the following system: 0 (absence of cellularity and neovascularisation), 1 (mild cellularity and neovascularisation), 2 (moderate cellularity and neovascularisation), and 3 (severe cellularity and neovascularisation) [14]. Moreover, microscopic fibrosis was defined based on the similar grading system as absent (0), mild (1), moderate (2), and severe (3).
Data were presented as mean = standard deviation (SD), median or percentage. Statistical analysis was performed with SPSS for windows version 13.0. The chi-square test (P < 0.05) was used to compare the incidence of pleural fibrosis, pleural cellularity and neovascularization, and pleural adhesions among the groups. The Kruskal-Wallis test (P < 0.05) was used to compare the median macroscopic, microscopic, cellularity, neovascularization and fibrosis scores among the groups. Thereafter, comparisons between two groups were conducted with the Mann–Whitney ranking test. In order to avoid accumulation of errors due to multiple comparisons, the significance level was modified dividing it (P < 0.05) by the number of comparisons made (Bonferroni correction) with P < 0.005 considered as significant.
Results
Gross necropsy
No deaths occurred in any of the studied groups. At 30 days, the normal saline (control) group produced no considerable adhesions or pleurodesis on gross observation. In the erythromycin group, adhesions were grossly visible between the parietal and the visceral pleurae in 66.6% (10/15) of the rats. Although Aerosil™ 200 group had the greatest number of rats with pleural adhesions (93.3%), there was no significant difference between the studied groups in this regard (P > 0.05, Table 1). Furthermore, Aerosil™ 200 and erythromycin plus Aerosil™ 200 groups showed higher numbers of diffuse adhesion (score 2) and complete obliteration (score 3) on gross observation (P > 0.05, Figure 1). The median macroscopic score in the Aerosil™ 200 group was significantly higher than that in the erythromycin group (P < 0.005, Bonferroni-corrected Mann–Whitney U test, Table 2).
Histopathology
The normal saline (control) group produced no considerable cellularity, neovascularisation, or fibrosis on microscopic observation at 30 days. Microscopically, all the erythromycin-treated rats exhibited inflammation, while only 40% (6/15) had pleural fibrosis. Pleural fibrosis was significantly lower in the erythromycin group compared with other treatment groups (P = 0.007, Table 1). Moreover, all rats in the treatment groups showed pleural inflammation (Table 1). In addition, pleural fibrosis was significantly higher in the erythromycin plus Aerosil™ 200 group compared with other treatment groups (P = 0.02, Table 1).
Figure 2 illustrates the number of each microscopic (inflammation/cellularity) score in the studied treatment groups. Accordingly, none of the treatment groups had absence of cellularity and neovascularisation in the microscopic assessment (score 0). Furthermore, Aerosil™ 200 and erythromycin plus Aerosil™ 200 groups showed higher numbers of severe cellularity and neovascularisation (score 3) on microscopic observation (P > 0.05, Figure 2). Overall, the median microscopic score in the erythromycin group was significantly lower than that in the Aerosil™ 200 and erythromycin plus Aerosil™ 200 groups (P < 0.005, Bonferroni-corrected Mann–Whitney U test, Table 2). On the other hand, the Aerosil™ 200 group showed higher cellularity score than erythromycin and tetracycline groups (P < 0.005, Bonferroni-corrected Mann–Whitney U test, Table 2). In addition, neovascularization and fibrosis scores in erythromycin plus Aerosil™ 200 group were significantly higher than those in the erythromycin group (P < 0.005, Bonferroni-corrected Mann–Whitney U test, Table 2).
Frequency of microscopic (inflammation/cellularity) scores in the treatment groups. Microscopic (inflammation/cellularity) scores were 0 = absence of cellularity and neovascularisation, 1 = mild cellularity and neovascularisation, 2 = moderate cellularity and neovascularisation, and 3 = severe cellularity and neovascularisation.
Discussion
This rat model evaluated the effectiveness of erythromycin, tetracycline, Aerosil™ 200 and erythromycin plus Aerosil™ 200 as pleural sclerosing agents. This study demonstrated that Aerosil™ 200 with or without erythromycin was more potent pleurodesis agent both grossly and microscopically. To the best of our knowledge, the present study is the first investigation to study the pleurodesing effect of intrapleural Aerosil™ 200. However, there are a few studies on the health effects of Aerosil™ 200. In an animal investigation by Reuzel and colleagues, subchronic inhalation of Aerosil™ 200 induced the most severe changes in the lungs among other examined amorphous silicas [9]. In another study, Johnston et al. observed reversible inflammatory responses in bronchoalveolar lavage after inhalation of amorphous silica (Aerosil™ 200), while no mutagenic events were noted [10]. Likewise, recent experimental studies confirmed the pulmonary fibrogenetic effects of amorphous silica such as Aerosil™ 200 [15–17].
Chemical pleurodesis with silica-containing materials has been of utmost interest. Yeginsu and colleagues found that bioglass was as effective as talc in terms of pleurodesis [7, 8]. It is believed that silicon dioxide or silica contributes to the pleurodesing effect of bioglass, talc and Aerosil™ 200. Silicon dioxide or silica exposure has been found to cause lung damage through direct cytotoxicity, generation of reactive oxygen species from alveolar macrophages, and stimulation of secretion of inflammatory cytokines, chemokines, and fibrogenic factors from alveolar macrophages and/or epithelial cells [7, 18]. Although similar mechanism might be deemed for the Aerosil™ 200 particles, further investigations orchestrated on the mechanisms of Aerosil™ 200-induced pleurodesis are recommended.
Both in gross and microscopic assessments, erythromycin was less potent pleurodesis agent than the Aerosil™ 200. This finding is in contrast to that of the previous experimental study indicating that erythromycin was an ideal pleural sclerosing agent, compared with talc, doxycycline and diazepam [2]. Moreover, in a recent clinical study by Balassoulis et al., erythromycin was found as an effective and safe pleurodesing agent in patients with recurrent malignant pleural effusions [19]. However, we do not have an explanation for such a difference in the pleurodesing effect of erythromycin. Furthermore, tetracycline was not superior to the other pleurodesing agents in the present study. This finding is compatible with that of the previous reports; fibrin tissue adhesive [20], talc [21], and mitoxantrone were found as more effective sclerosing agents than tetracycline for pleurodesis [22]. In contrast, Vargas and colleagues found that tetracycline, rather than bleomycin and Corynebacterium parvum, was more potent pleurodesing agent in a rabbit model [23, 24]. In a systematic review, tetracycline was reported to be associated with more recurrences when compared to talc [3]. The available clinical evidence supports the use of talc as the sclerosant of choice rather than other sclerosants (tetracycline, bleomycin, or mustine) [1].
This study has certain limitations. We did not investigate talc as a sclerosing agent in the present study. The rationale behind this exclusion was the lack of sterile and pure talc in Iran. Moreover, other routinely used pleurodesing agents such as bleomycin and parenteral doxycycline were not available due to their high costs. Therefore, further studies are recommended to be orchestrated in order to investigate the probable advantage of the Aerosil™ 200 over the most commonly used pleurodesis agents such as sterile and pure talc in terms of efficacy, safety, rapidity of action, mechanism of action or cost. In addition, one may consider the rabbit model as generally more established method for experimental pleurodesis. However, there are a number of experimental studies of pleurodesis on the rats [20, 25–27]. Only single dose of 35 mg/kg was studied for each sclerosant, and different doses might have resulted in more favorable responses. However, the applied treatment dosages were based on those of the previous studies. Future studies with larger doses of erythromycin and tetracycline may achieve higher response rates. Furthermore, distant sequelae of the studied pleurodesing agents in the contralateral lung as well as the liver along with their systemic effects were not evaluated. Liver enzyme tests, histopathological assessment of the contralateral lung and the liver, and serum and tissue angiotensin-converting enzyme could have provided precious information regarding the toxicity of the studied pleurodesing agents, in particular the Aerosil™ 200. In addition, grading of the pleurodesis immediately after sacrificing the animals while the tissues were fresh and soft might have yielded to different results. The formalin exposure makes the tissues firm and shrunk, resulting in difficult evaluation of the pleural adhesions [8].
Conclusion
In conclusion, this preliminary study suggests that Aerosil™ 200 with or without erythromycin may be more potent pleurodesis agent than erythromycin and tetracycline. As superiority between Aerosil™ 200 alone and Aerosil™ 200 plus erythromycin could not be determined with the results of the present study, further cost-effective investigations targeting at the distant sequelae of these treatments are required.
Abbreviations
- SiO2:
-
Silicon dioxide
- HE:
-
Hematoxylin and eosin.
References
Shaw P, Agarwal R: Pleurodesis for malignant pleural effusions. Cochrane Database Syst Rev. 2004, 1: CD002916-
Miller Q, Meschter C, Neumaster T, Pratt J, Moulton M, Downey D, Harre J: Comparison of pleurodesis by erythromycin, talc, doxycycline, and diazepam in a rabbit model. J Surg Educ. 2007, 64: 41-45. 10.1016/j.cursur.2006.07.006.
Tan C, Sedrakyan A, Browne J, Swift S, Treasure T: The evidence on the effectiveness of management for malignant pleural effusion: a systematic review. Eur J Cardiothorac Surg. 2006, 29: 829-838. 10.1016/j.ejcts.2005.12.025.
Marchi E, Teixeira LR, Vargas FS: Management of malignancy-associated pleural effusion: current and future treatment strategies. Am J Respir Med. 2003, 2: 261-273.
Dikensoy O, Light RW: Alternative widely available, inexpensive agents for pleurodesis. Curr Opin Pulm Med. 2005, 11: 340-344. 10.1097/01.mcp.0000166587.24127.91.
Merget R, Bauer T, Küpper HU, Philippou S, Bauer HD, Breitstadt R, Bruening T: Health hazards due to the inhalation of amorphous silica. Arch Toxicol. 2002, 75: 625-634. 10.1007/s002040100266.
Yeginsu A, Filiz NO, Köseoğlu D, Etikan I: Bioglass as a pleurodesing agent as effective as talc in rabbits. Turkish J Thorac Cardiovasc Surg. 2005, 13: 386-391.
Yeginsu A, Ergin M, Ozyurt H, Bassorgun CI: Pleurodesic effect of bioglass in experimental rabbits. Iran Red Crescent Med J. 2009, 11: 254-258.
Reuzel PG, Bruijntjes JP, Feron VJ, Woutersen RA: Subchronic inhalation toxicity of amorphous silicas and quartz dust in rats. Food Chem Toxicol. 1991, 29: 341-354. 10.1016/0278-6915(91)90205-L.
Johnston CJ, Driscoll KE, Finkelstein JN, Baggs R, O’Reilly MA, Carter J, Gelein R, Oberdörster G: Pulmonary chemokine and mutagenic responses in rats after subchronic inhalation of amorphous and crystalline silica. Toxicol Sci. 2000, 56: 405-413. 10.1093/toxsci/56.2.405.
Jouyban A, Shoja MM, Ardalan MR, Khoubnasabjafari M, Sadighi A, Tubbs RS, Agutter PS, Ghabili K: The effect of quince leaf decoction on renal injury induced by hypercholesterolemia in rabbits: a pilot study. J Med Plants Res. 2011, 5: 5291-5295.
Ashrafi H, Ghabili K, Alihemmati A, Jouyban A, Shoja MM, Aslanabadi S, Adl FH, Ghavimi H, Hajhosseini L: The effect of quince leaf (Cydonia oblonga Miller) decoction on testes in hypercholesterolemic rabbits: a pilot study. Afr J Tradit Complement Altern Med. 2013, 10: 277-282.
Mitchem RE, Herndon BL, Fiorella RM, Molteni A, Battie CN, Reisz GR: Pleurodesis by autologous blood, doxycycline, and talc in a rabbit model. Ann Thorac Surg. 1999, 67: 917-921. 10.1016/S0003-4975(99)00160-5.
Hurewitz AN, Lidonicci K, Wu CL, Reim D, Zucker S: Histologic changes of doxycycline pleurodesis in rabbits. Effect of concentration and pH. Chest. 1994, 106: 1241-1245. 10.1378/chest.106.4.1241.
Chen Y, Chen J, Dong J, Jin Y: Comparing study of the effect of nanosized silicon dioxide and microsized silicon dioxide on fibrogenesis in rats. Toxicol Ind Health. 2004, 20: 21-27. 10.1191/0748233704th190oa.
Choi M, Cho WS, Han BS, Cho M, Kim SY, Yi JY, Ahn B, Kim SH, Jeong J: Transient pulmonary fibrogenic effect induced by intratracheal instillation of ultrafine amorphous silica in A/J mice. Toxicol Lett. 2008, 182: 97-101. 10.1016/j.toxlet.2008.08.019.
Costantini LM, Gilberti RM, Knecht DA: The phagocytosis and toxicity of amorphous silica. PLoS One. 2011, 6: e14647-10.1371/journal.pone.0014647.
Castranova V, Vallyathan V: Silicosis and coal workers’ pneumoconiosis. Environ Health Perspect. 2000, 108: 675-684.
Balassoulis G, Sichletidis L, Spyratos D, Chloros D, Zarogoulidis K, Kontakiotis T, Bagalas V, Porpodis K, Manika K, Patakas D: Efficacy and safety of erythromycin as sclerosing agent in patients with recurrent malignant pleural effusion. Am J Clin Oncol. 2008, 31: 384-389. 10.1097/COC.0b013e318165c061.
Cetin B, Atalay C, Arzu Koçkaya E, Turan Akay M: The efficacy of fibrin tissue adhesives in pleurodesis in rats. Exp Lung Res. 2005, 31: 713-718. 10.1080/01902140500248597.
Mourad IA, Abdel Rahman AR, Aziz SA, Saber NM, Fouad FA: Pleurodesis as a palliative treatment of advanced lung cancer with malignant pleural effusion. J Egypt Natl Canc Inst. 2004, 16: 188-194.
Light RW, Wang NS, Despars JA, Gruer SE, Sassoon C, Vargas FS: Comparison of mitoxantrone and tetracycline as pleural sclerosing agents in rabbits. Lung. 1996, 174: 373-381.
Vargas FS, Wang NS, Lee HM, Gruer SE, Sassoon CS, Light RW: Effectiveness of bleomycin in comparison to tetracycline as pleural sclerosing agent in rabbits. Chest. 1993, 104: 1582-1584. 10.1378/chest.104.5.1582.
Vargas FS, Wang NS, Teixeira LR, Carmo AO, Silva LM, Light RW: Corynebacterium parvum versus tetracycline as pleural sclerosing agents in rabbits. Eur Respir J. 1995, 8: 2174-2177. 10.1183/09031936.95.08122174.
Gözübüyük A, Ozpolat B, Ciçek AF, Caylak H, Yücel O, Kavaklı K, Gürkök S, Genç O: Comparison of side effects of oxytetracycline and talc pleurodesis: an experimental study. J Cardiothorac Surg. 2010, 5: 128-10.1186/1749-8090-5-128.
Ozpolat B, Gazyagci S, Gözübüyük A, Ayva S, Atinkaya C: Autologous blood pleurodesis in rats to elucidate the amounts of blood required for reliable and reproducible results. J Surg Res. 2010, 161: 228-232. 10.1016/j.jss.2009.01.027.
Fraticelli A, Robaglia-Schlupp A, Riera H, Monjanel-Mouterde S, Cau P, Astoul P: Distribution of calibrated talc after intrapleural administration: an experimental study in rats. Chest. 2002, 122: 1737-1741. 10.1378/chest.122.5.1737.
Acknowledgments
This study was financially supported by a grant from the Tuberculosis and Lung Disease Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
S.H., K.H., K.M., and R.A. participated in the design of study and performed the experimental parts of the research. E.A., S.G. and K.G. participated in acquisition of data, analysis and interpretation of data, drafting the article, and final approval of this version. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hashemzadeh, S., Hashemzadeh, K., Mamaghani, K. et al. Pleurodesis by erythromycin, tetracycline, Aerosil™ 200, and erythromycin plus Aerosil™ 200 in a rat model: a preliminary study. DARU J Pharm Sci 20, 79 (2012). https://doi.org/10.1186/2008-2231-20-79
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2008-2231-20-79