Abstract
Surfactant protein D (SP-D) is a collectin that plays an important role in the innate immune system and takes part in the surfactant homeostasis by regulating the surfactant pool size. The aims of this study were to investigate the values of SP-D in umbilical cord blood and capillary blood of premature infants and to relate the levels to perinatal conditions. A total of 254 premature infants were enrolled in the present study. Umbilical cord blood was drawn at the time of birth and capillary blood at regular intervals throughout the admission. The concentration of SP-D in umbilical cord blood and capillary blood was measured using ELISA technique. The median concentration of SP-D in umbilical cord blood was twice as high as in mature infants, 769 ng/mL (range 140–2,551), with lowest values in infants with intrauterine growth retardation (IUGR) and rupture of membranes (ROM). The median concentration of SP-D in capillary blood day 1 was 1,466 ng/mL (range 410–5,051 ng/mL), with lowest values in infants born with ROM and delivered vaginally. High SP-D levels in umbilical cord blood and capillary blood on day 1 were found to be more likely in infants in need for respiratory support or surfactant treatment and susceptibility to infections. We conclude that SP-D concentrations in umbilical cord blood and capillary blood in premature infants are twice as high as in mature infants and depend on several perinatal conditions. High SP-D levels in umbilical cord blood and capillary blood on day 1 were found to be related to increased risk of RDS and infections.
Similar content being viewed by others
Main
Respiratory distress syndrome (RDS) is a main contributor to increased mortality and morbidity among premature infants. RDS is caused by lack of pulmonary surfactant leading to atelectasis and ventilation-perfusion mismatch of the lungs (1). Biochemically, pulmonary surfactant is a mixture of phospholipids and associated proteins which are synthesized, stored, secreted and recycled by type II cells in the airways (2). This mixture forms a monolayer at the air-liquid interface which lowers the surface tension, stabilizes alveoli and terminal airways at low lung volume and prevents alveolar collapse at the end of the expiration. Treatment with synthetic or naturally developed surfactant has been associated with a decline in the mortality of RDS among premature infants (3,4).
Four specific surfactant proteins have been identified, called surfactant protein (SP) A-D. SP-B and SP-C have been characterized as hydrophobic polypeptides that enhance the adsorption of lipid to the surface of the alveoli (5), while SP-A and SP-D are hydrophilic and participate in the innate host defense immune system. SP-D binds to macrophages and neutrophils and promotes phagocytosis and killing of bacteria, fungi, and viruses (6). Polymorphism in the amino acid residue 11 of the SPD gene has been found to increase severity of respiratory syncytial virus infection and susceptibility to tuberculosis (7,8).
SP-A and SP-B are instrumental in surfactant storage in lamellar bodies and in the formation of tubular myelin and surfactant monolayer (9). The role of SP-D in surfactant homeostasis is not yet fully understood. SP-D knockout mice however, accumulate phospholipids in the alveolar space leading to emphysematous changes (10) and increased susceptibility to infections (6). SP-D regulates the surfactant pool size by influencing the surfactant ultrastructure and its reuptake in type II cells (11). SP-D is a large, complex glycoprotein with monomeric structure forming trimers that cluster to form a quaternary cruciate structure (12).
SP-D plays an important role in the innate immune system. In premature infants the innate immune system is especially important, since efficient transfer of maternal antibodies occurs only after 34 wk of gestation, leading to low levels of IgG at birth in premature infants (13). SP-D in bronchoalveolar lavage increases during the first days of life in prematurely born infants, and low concentration of SP-D was found to predict worse clinical outcome (14). The levels of SP-A in cord blood has been found to predict RDS among prematurely born infants (15). We have demonstrated that levels of SP-D in cord blood and capillary blood of mature newborn infants depend on several maternal and perinatal conditions (16) including labor, mode of delivery and maternal smoking. In this study we report, to our knowledge for the first time, cord blood and capillary blood levels of SP-D in premature infants and their influence on respiratory distress syndrome and susceptibility to neonatal infections.
MATERIALS AND METHODS
Subjects.
From August, 2000 to January, 2002, prematurely born infants with gestational age < 36 wk were included in the present study. The infants were born at Odense University Hospital or transferred from district hospitals shortly after birth. Infants with major anomalies and missing informed consent from the parents were excluded. Umbilical cord blood was drawn from infants born at our hospital immediately after birth. The midwives were instructed to draw blood preferably from the umbilical artery.
Capillary blood was sampled daily when routine blood sampling was done until the infant was stable, then weekly. The capillary blood was sampled by heel-prick. All samples were stored at −20°C until measurement of SP-D.
The infants were treated according the clinic's usual guidelines with early nasal continuous positive airway pressure (CPAP) (17) and early rescue surfactant (18).
Methods.
SP-D concentrations in plasma were measured by ELISA. The assay is based on pepsin-digested polyclonal rabbit anti-SP-D antibody as first layer antibody and monoclonal anti-SP-D antibody as detector antibody as described earlier (19). The samples were tested in duplicates and accepted with a coefficient of variation of 5%.
Statistics.
Data were analyzed using the STATA program. Mann-Witney U-test was used to compare levels of SP-D between two groups, and nonparametric test for trend across ordered groups for more than two groups. Wilcoxon sign rank test was used to analyze paired data. The variance between SP-D levels in arterial, venous and capillary blood was tested using Bland-Altman's plot with Pitman's test of difference in variance. Correlations between continuous variables and SP-D levels were analyzed by simple regression analysis. In all statistical methods, p < 0.05 were considered significant. Results are expressed as medians (range) unless otherwise noted.
Ethical considerations.
Written informed consent was given for every child enrolled in the study. The study was conducted according to the Helsinki II recommendations and was approved by the Regional Committee for Research on Human Subjects in the Counties of Funen and Vejle.
RESULTS
A total of 254 infants with gestational age 322 weeks (235–356) were included in the study out of a number of 276 premature infants treated in Odense University Hospital during this time period. The clinical data are shown in Table 1. Umbilical cord blood was drawn from 165 of the infants. The levels of SP-D in these samples was 769 ng/mL (140–2,551). The SP-D level in umbilical cord blood did not depend on gestational age. The reasons for missing umbilical cord blood samples were in 60 cases infants transferred to the institution after birth, and 39 infants from whom no blood could be drawn from the umbilical cord. The umbilical cord blood was sampled from the arterial side in 71 infants. There was no significant difference between the arterial SP-D levels, 705 ng/mL (140–2,551) and the venous SP-D levels, 806 ng/mL (176–2,079). The SP-D levels in umbilical cord blood were lower in infants with intrauterine growth retardation (IUGR) and rupture of membranes (ROM) (Table 2).
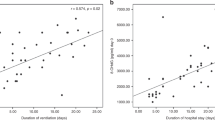
The population of infants had in median five capillary samples drawn (1–29) during their admission. There was a good correlation between umbilical cord blood levels and the measured capillary levels throughout the first 35 d (p < 0.0001). The SP-D levels in capillary blood from the first day of life were significantly lower in infants with ROM, after vaginal delivery or when the infants were born by mothers who smoked (Table 2).
The capillary SP-D levels on day 1 was 1,466 ng/mL (410–5,051) and increased to 1,788 ng/mL (374–13,154) on day 4, and then decreased during the next week (Fig. 1). However, this alteration was only found in infants requiring ventilatory support, i.e., oxygen, CPAP or ventilator treatment (Fig. 2). From day 1 till day 49 the SP-D levels in infants with need of respiratory support (data shown for oxygen only) were significantly increased.
Capillary SP-D levels on days 1–77 in infants with (Ė) (n = 71) and without (τ) (n = 166) need of oxygen. Capillary SP-D levels in infants with need of oxygen increased rapidly until day 4 and then slowly decreased. The values were significantly higher than values for infants without oxygen from day 1 to day 49. Values are given as median (95% confidence interval).
The SP-D levels in capillary blood on day 1 in the 34 (13%) infants treated with surfactant were significantly higher than the levels in infants not treated (Table 3), but there was no difference in the umbilical cord levels. Of the survivors, 172 (73%) were treated with CPAP, 71 (30%) with oxygen and 14 (6%) needed ventilator treatment. Their SP-D levels in capillary blood on day 1 were significantly higher than the levels observed in infants without need of respiratory support, and the SP-D levels in umbilical cord blood were increased in infants later treated with oxygen. Notably, the SP-D levels in umbilical cord blood and on day 1 were significantly higher among the 23 (9%) infants who developed septicemia later during the admission. These infants developed septicemia with a median of day 11 (range 1–42). The higher levels were seen independently of the time interval to development of septicemia.
The SP-D levels in the 12 (5%) infants who developed chronic lung disease (CLD), with need of oxygen at 36 wk gestational age, were not increased in umbilical cord blood or capillary blood on day 1, but at age 36 wk the levels were significantly increased (p = 0.001).
The SP-D levels in the 17 (6.7%) non-surviving infants were not significantly different from levels in survivors. Four of the infants died within 24 h. Their SP-D levels in umbilical cord blood tended to be lower, 407 ng/mL (191–1083), than in the 13 infants who died later, 814 (209–1,611).
DISCUSSION
We have recently demonstrated that SP-D levels in cord blood and capillary blood of mature infants are influenced by mode of delivery, labor and maternal smoking (16). In this study we have determined the levels of SP-D in prematurely born infants. We found that the levels of SP-D both in umbilical cord blood and capillary blood were highly variable and depended on several perinatal conditions. Furthermore, we observed that the SP-D levels were related to morbidity in prematurely born infants.
RDS is a major cause of increased morbidity and mortality among premature infants. This clinical entity is caused by lack of pulmonary surfactant, leading to collapse of the alveoli and damage to the alveolar septae. We found high SP-D capillary levels in infants in need of oxygen or CPAP treatment and in infants treated with surfactant. Increased levels of SP-D are also found in adults with acute and chronic lung injury (20) and children with interstitial lung disease (21). These findings may at least partly be due to the alveolar-to-vascular leakage of surfactant proteins from the alveoli to the bloodstream (22). Increased permeability of the lung vessels leads to leakage of serum proteins into the alveoli, resulting in inactivation of the surfactant (23) and further lack of surfactant at the alveolar membrane. Elevations of SP-D in the serum could also reflect increased type II cell activity as a reparative process following lung injury with a resultant leak back into the blood (24). SP-D is mainly produced in the epithelial cells in the lungs, but is also found in epithelial cells and secretory glands in the gastrointestinal tract and in other tissues (25). The contribution of this production to the values measured in serum is not known.
Exposure of rats to hyperoxia leads to increased expression of SP-D mRNA, but to decreased amount of immunodetectable SP-D in lung tissue (26), leading to the assumption that SP-D is excreted into the alveolar space and from there enters the circulation. The increase in SP-D is therefore probably due to both capillary leak and increased release of SP-D from epithelial cells due to the inflammatory response (19). Mechanical ventilation of the lungs has been shown to modulate SP-D gene expression and increase SP-D production (27) and probably the pressure delivered to the lungs by the nasal CPAP used to treat respiratory distress (28) has the same effect.
SP-D regulates the surfactant pool size by influencing the surfactant ultrastructure and its reuptake in type II cells (11). SP-D does not localize to lamellar bodies, but can, in absence of SP-A, form atypical but highly surface-active tubular aggregates by binding phosphatidylinositol, a component of mammalian surfactant that is increased in lung damage (29).
Low levels of SP-D in bronchial lavage have been found to predict bad outcome and increased susceptibility to infections (14). We found markedly increased levels of SP-D in umbilical cord blood and capillary blood on the first day of life in infants that later developed sepsis independent of interval between birth and the diagnosis of septicemia. This finding is consistent with our data obtained in mature newborn infants (16). One could speculate that the high SP-D levels were due to an increased capillary leak leading to decreased levels of SP-D in the lungs. Such an effect may add to the newborn's susceptibility to infections as observed experimentally in premature baboons (30). However, this explanation does not take into account the higher levels found in umbilical cord blood before breathing is started. There is some evidence that alveolar-vascular permeation is influenced by the degree of lung maturation (24). One could speculate that the lungs of the infants who later develop septicemia have less mature alveolar-vascular integrity and that the leakage of proteins into the circulation therefore takes place before birth.
The SP-D levels in umbilical cord blood from premature infants were twice as high as in mature infants, and did not decrease with gestational age as we previously described in mature infants for gestational age 36–43 wk (16). These data suggest that the decrease in SP-D levels occurs late in pregnancy. The production of SP-D in fetal human lungs begins in the bronchiolar and terminal epithelium from about 21 wk of gestation (31). Several studies of human fetuses show low production of SP-D in the lungs and amniotic fluid in early gestation, increasing through gestation, but decreasing late in gestation (32–34). Besides the lungs, SP-D is synthesized in various exocrine ducts, the mucosa of the gastrointestinal and genitourinary tracts and placenta (25,34). The high blood levels found in premature infants in our study may therefore be due to relative larger production in placenta and other extra-pulmonary tissue.
IUGR is often the result of a poorly functioning placenta, and SP-D is synthesized in the trophoblast sub-populations in the placenta (34). However, we found low levels of SP-D not only in venous cord blood, but also in arterial cord blood, indicating that also the infants' production is decreased as a consequence of IUGR. IUGR is found to decrease production rates of lung saturated phosphatidylcholine (35) and the production of total lung liquid (36). The low production is probably due to diminished amounts of substrates.
The capillary SP-D levels the first day of life were twice as high as the umbilical cord blood levels. The levels of SP-D in the lungs of newborn infants have been found to rise significantly the first days of life (14). This could be due to the physiologic re-absorption of lung liquid across the pulmonary epithelium to the circulation during the start of the respiration (37).
Smoking during pregnancy decreases trophoblast proliferation and reduces the length of villous capillaries in the placenta leading to diminished area for gas and nutrients exchange (39,40). Recently we have shown by immunohistochemical analysis that SP-D is synthesized in all villous and extravillous trophoblast sub-populations in the placenta (34). Consistent with this, we have demonstrated decreased SP-D levels in umbilical venous blood in mature infants of smoking mothers (16). However, in the present study the SP-D levels of infants from smoking mothers were only lower in capillary blood and not in umbilical venous cord blood.
In summary, we have in this study determined normal levels of SP-D in blood of premature infants. Perinatal events may influence SP-D levels both in umbilical and capillary blood in opposing directions. High levels of SP-D in umbilical blood and capillary blood day 1 indicate development of RDS and susceptibility to infection. A study of the connection between genetic polymorphisms, SP-D levels in blood and clinical symptoms are in progress. Further studies are needed to clarify if SP-D can be used as a prognostic marker in premature infants.
Abbreviations
- CPAP:
-
nasal continuous positive airway pressure
- IUGR:
-
intrauterine growth retardation
- RDS:
-
respiratory distress syndrome
- ROM:
-
rupture of membrane for more than 1 hour before birth
- SP:
-
surfactant protein
References
Avery ME 2000 Surfactant deficiency in hyaline membrane disease: the story of discovery. Am J Respir Crit Care Med 161: 1074–1075
Wright JR 1990 Clearance and recycling of pulmonary surfactant. Am J Physiol 259: L1–L12
Cole FS, Hamvas A, Nogee LM 2001 Genetic disorders of neonatal respiratory function. Pediatr Res 50: 157–162
Verder H, Robertson B, Greisen G, Ebbesen F, Albertsen P, Lundstrom K, Jacobsen T 1994 Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome. Danish-Swedish Multicenter Study Group. N Engl J Med 331: 1051–1055
Whitsett JA, Ohning BL, Ross G, Meuth J, Weaver T, Holm BA, Shapiro DL, Notter RH 1986 Hydrophobic surfactant-associated protein in whole lung surfactant and its importance for biophysical activity in lung surfactant extracts used for replacement therapy. Pediatr Res 20: 460–467
LeVine AM, Whitsett JA, Gwozdz JA, Richardson TR, Fisher JH, Burhans MS, Korfhagen TR 2000 Distinct effects of surfactant protein A or D deficiency during bacterial infection on the lung. J Immunol 165: 3934–3940
Floros J, Lin HM, Garcia A, Salazar MA, Guo X, DiAngelo S, Montano M, Luo J, Pardo A, Selman M 2000 Surfactant protein genetic marker alleles identify a subgroup of tuberculosis in a Mexican population. J Infect Dis 182: 1473–1478
Lahti M, Lofgren J, Marttila R, Renko M, Klaavuniemi T, Haataja R, Ramet M, Hallman M 2002 Surfactant protein D gene polymorphism associated with severe respiratory syncytial virus infection. Pediatr Res 51: 696–699
Creuwels LA, van Golde LM, Haagsman HP 1997 The pulmonary surfactant system: biochemical and clinical aspects. Lung 175: 1–39
Botas C, Poulain F, Akiyama J, Brown C, Allen L, Goerke J, Clements J, Carlson E, Gillespie AM, Epstein C, Hawgood S 1998 Altered surfactant homeostasis and alveolar type II cell morphology in mice lacking surfactant protein D. Proc Natl Acad Sci U S A 95: 11869–11874
Ikegami M, Na CL, Korfhagen TR, Whitsett JA 2005 Surfactant protein D influences surfactant ultrastructure and uptake by alveolar type II cells. Am J Physiol Lung Cell Mol Physiol 288: L552–L561
Mason RJ, Greene K, Voelker DR 1998 Surfactant protein A and surfactant protein D in health and disease. Am J Physiol 275: L1–L13
Morell A, Sidiropoulos D, Herrmann U, Christensen KK, Christensen P, Prellner K, Fey H, Skvaril F 1986 IgG subclasses and antibodies to group B streptococci, pneumococci, and tetanus toxoid in preterm neonates after intravenous infusion of immunoglobulin to the mothers. Pediatr Res 20: 933–936
Beresford MW, Shaw NJ 2003 Bronchoalveolar lavage surfactant protein A, B, and D concentrations in preterm infants ventilated for respiratory distress syndrome receiving natural and synthetic surfactants. Pediatr Res 53: 663–670
Cho K, Matsuda T, Okajima S, Matsumoto Y, Sagawa T, Fujimoto S, Kobayashi K 2000 Prediction of respiratory distress syndrome by the level of pulmonary surfactant protein A in cord blood sera. Biol Neonate 77: 83–87
Dahl M, Juvonen PO, Holmskov U, Husby S 2005 Surfactant protein D in newborn infants. Factors influencing surfactant protein D levels in umbilical cord blood and capillary blood. Pediatr Res 58: 908–912
Kamper J, Wulff K, Larsen C, Lindequist S 1993 Early treatment with nasal continuous positive airway pressure in very low-birth-weight infants. Acta Paediatr 82: 193–197
Verder H, Albertsen P, Ebbesen F, Greisen G, Robertson B, Bertelsen A, Agertoft L, Djernes B, Nathan E, Reinholdt J 1999 Nasal continuous positive airway pressure and early surfactant therapy for respiratory distress syndrome in newborns of less than 30 weeks' gestation. Pediatrics 103:E24
Leth-Larsen R, Nordenbaek C, Tornoe I, Moeller V, Schlosser A, Koch C, Teisner B, Junker P, Holmskov U 2003 Surfactant protein D (SP-D) serum levels in patients with community-acquired pneumonia. Clin Immunol 108: 29–37
Eisner MD, Parsons P, Matthay MA, Ware L, Greene K 2003 Plasma surfactant protein levels and clinical outcomes in patients with acute lung injury. Thorax 58: 983–988
Honda Y, Kuroki Y, Matsuura E, Nagae H, Takahashi H, Akino T, Abe S 1995 Pulmonary surfactant protein D in sera and bronchoalveolar lavage fluids. Am J Respir Crit Care Med 152: 1860–1866
Robertson B, Curstedt T, Herting E, Sun B, Akino T, Schafer KP 1995 Alveolar-to-vascular leakage of surfactant protein A in ventilated immature newborn rabbits. Biol Neonate 68: 185–190
Jobe A, Ikegami M, Jacobs H, Jones S, Conaway D 1983 Permeability of premature lamb lungs to protein and the effect of surfactant on that permeability. J Appl Physiol 55: 169–176
Hermans C, Bernard A 1999 Lung epithelium-specific proteins: characteristics and potential applications as markers. Am J Respir Crit Care Med 159: 646–678
Madsen J, Kliem A, Tornoe I, Skjodt K, Koch C, Holmskov U 2000 Localization of lung surfactant protein D on mucosal surfaces in human tissues. J Immunol 164: 5866–5870
Aderibigbe AO, Thomas RF, Mercer RR, Auten RL 1999 Brief exposure to 95% oxygen alters surfactant protein D and mRNA in adult rat alveolar and bronchiolar epithelium. Am J Respir Cell Mol Biol 20: 219–227
Awasthi S, Coalson JJ, Crouch E, Yang F, King RJ 1999 Surfactant proteins A and D in premature baboons with chronic lung injury (Bronchopulmonary dysplasia). Evidence for an inhibition of secretion. Am J Respir Crit Care Med 160: 942–949
Kamper J, Ringsted C 1990 Early treatment of idiopathic respiratory distress syndrome using binasal continuous positive airway pressure. Acta Paediatr Scand 79: 581–586
Poulain FR, Akiyama J, Allen L, Brown C, Chang R, Goerke J, Dobbs L, Hawgood S 1999 Ultrastructure of phospholipid mixtures reconstituted with surfactant proteins B and D. Am J Respir Cell Mol Biol 20: 1049–1058
Awasthi S, Coalson JJ, Yoder BA, Crouch E, King RJ 2001 Deficiencies in lung surfactant proteins A and D are associated with lung infection in very premature neonatal baboons. Am J Respir Crit Care Med 163: 389–397
Mori K, Kurihara N, Hayashida S, Tanaka M, Ikeda K 2002 The intrauterine expression of surfactant protein D in the terminal airways of human fetuses compared with surfactant protein A. Eur J Pediatr 161: 431–434
Dulkerian SJ, Gonzales LW, Ning Y, Ballard PL 1996 Regulation of surfactant protein D in human fetal lung. Am J Respir Cell Mol Biol 15: 781–786
Stahlman MT, Gray ME, Hull WM, Whitsett JA 2002 Immunolocalization of surfactant protein-D (SP-D) in human fetal, newborn, and adult tissues. J Histochem Cytochem 50: 651–660
Leth-Larsen R, Floridon C, Nielsen O, Holmskov U 2004 Surfactant protein D in the female genital tract. Mol Hum Reprod 10: 149–154
Chen CM, Wang LF, Su B 2004 Effects of maternal undernutrition during late gestation on the lung surfactant system and morphometry in rats. Pediatr Res 56: 329–335
Cock ML, Albuquerque CA, Joyce BJ, Hooper SB, Harding R 2001 Effects of intrauterine growth restriction on lung liquid dynamics and lung development in fetal sheep. Am J Obstet Gynecol 184: 209–216
Pfister RE, Ramsden CA, Neil HL, Kyriakides MA, Berger PJ 2001 Volume and secretion rate of lung liquid in the final days of gestation and labor in the fetal sheep. J Physiol 535: 889–899
Kalache KD, Chaoui R, Marks B, Wauer R, Bollmann R 2002 Does fetal tracheal fluid flow during fetal breathing movements change before the onset of labor?. BJOG 109: 514–519
Larsen LG, Clausen HV, Jonsson L 2002 Stereologic examination of placentas from mothers who smoke during pregnancy. Am J Obstet Gynecol 186: 531–537
Shiverick KT, Salafia C 1999 Cigarette smoking and pregnancy I: ovarian, uterine and placental effects. Placenta 20: 265–272
Acknowledgements
The authors would like to thank Ivan Iachine for statistical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from Direktør Ib Henriksens Foundation, Dagmar Marshalls Foundation, Gudrun Krauses Mindelegat, Overlægera°dets legatudvalg and Fonden for lægevidenskabelig forskning.at Odense University Hospital.
Rights and permissions
About this article
Cite this article
Dahl, M., Holmskov, U., Husby, S. et al. Surfactant Protein D Levels in Umbilical Cord Blood and Capillary Blood of Premature Infants. The Influence of Perinatal Factors. Pediatr Res 59, 806–810 (2006). https://doi.org/10.1203/01.pdr.0000219122.81734.03
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000219122.81734.03