ABSTRACT
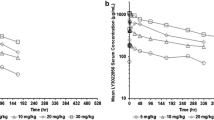
In this investigation, we test the hypothesis that treatment with sorafenib, an anti-angiogenic agent, decreases tumor vascularization and, consequently, hinders the delivery of monoclonal antibodies (mAb) to xenograft tumors. Severe combined immunodeficiency mice bearing carcinoembryonic antigen (CEA) expressing tumor xenografts were divided into control and sorafenib-treated groups. Sorafenib was administered to the latter group at 50 mg/kg IP every 48 h, starting 4 days post-tumor implantation. When tumors attained a size of 200–300 mm3, mice were evaluated for (a) tumor microvessel density (using immunohistochemical analysis), (b) tumor macromolecular extravasation (using Evans Blue Dye (EBD)), (c) pharmacokinetics of an anti-CEA mAb, T84.66, following an intravenous dose of 10 mg/kg, and (d) intra-tumoral spatial distribution of T84.66 (using autoradiography). Sorafenib treatment resulted in a substantial reduction in tumor growth rate, a visible reduction in tumor microvessel density, and in a 46.4% decrease in EBD extravasation in tumor tissue (p < 0.0455). For control and treated mice, no significant difference was found for the area under the mAb plasma concentration-time curve (AUC(0–7d): 1.67 × 103 ± 1.28 × 102 vs. 1.76 × 103 ± 1.75 × 102 nM × day, p = 0.51). However, tumor AUC(0–7d) was reduced by 40.8% in sorafenib-treated mice relative to that observed in control mice (5.61 × 102 ± 4.27 × 101 vs. 9.48 × 102 ± 5.61 × 101 nM × day, p < 0.001). Sorafenib therapy was also found to markedly alter mAb tumor spatial distribution. The results collectively suggest that sorafenib treatment causes a significant reduction in mAb delivery to, and distribution within, solid tumors.










Similar content being viewed by others
References
Kenny JR, Liu MM, Chow AT, Earp JC, Evers R, Slatter JG, et al. Therapeutic protein drug-drug interactions: navigating the knowledge gaps-highlights from the 2012 AAPS NBC roundtable and IQ consortium/FDA workshop. AAPS J. 2013;15(4):933–40.
Maini RN, Breedveld FC, Kalden JR, Smolen JS, Davis D, Macfarlane JD, et al. Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum. 1998;41(9):1552–63.
Kovarik JM, Pescovitz MD, Sollinger HW, Kaplan B, Legendre C, Salmela K, et al. Differential influence of azathioprine and mycophenolate mofetil on the disposition of basiliximab in renal transplant patients. Clin Transpl. 2001;15(2):123–30.
Pescovitz MD, Bumgardner G, Gaston RS, Kirkman RL, Light S, Patel IH, et al. Pharmacokinetics of daclizumab and mycophenolate mofetil with cyclosporine and steroids in renal transplantation. Clin Transpl. 2003;17(6):511–7.
Su CG, Lichtenstein GR. Influence of immunogenicity on the long-term efficacy of infliximab in Crohn’s disease. N Engl J Med. 2003;125(5):1544–6.
Zhou H, Mascelli MA. Mechanisms of monoclonal antibody-drug interactions. Annu Rev Pharmacol Toxicol. 2011;51:359–72.
Schmitt C, Kuhn B, Zhang X, Kivitz AJ, Grange S. Disease-drug-drug interaction involving tocilizumab and simvastatin in patients with rheumatoid arthritis. Clin Pharmacol Ther. 2011;89(5):735–40.
Actemra® (tocilizumab) [package insert] San Francisco, CA: Genentech Inc; [cited 2016 Jan 6]; Available from: http://www.gene.com/download/pdf/actemra_prescribing.pdf.
Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 2004;351(4):337–45.
Erbitux® (cetuximb) [package insert] Indianapolis, IN : Eli Lilly and Company; [cited 2016 Jan 6]; Available from: http://pi.lilly.com/us/erbitux-uspi.pdf
US Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and ResearchGuidance for Industry Drug Interaction Studies -Study Design, Data Analysis,Implications for Dosing, and labeling Recommendations Rockville, MD February 2012 [cited 2016 Jan 6]; Available from: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM292362.pdf.
Hansen RJ, Balthasar JP. Effects of intravenous immunoglobulin on platelet count and antiplatelet antibody disposition in a rat model of immune thrombocytopenia. Blood. 2002;100(6):2087–93.
Jin F, Tayab ZR, Balthasar JP. Pharmacokinetic and pharmacodynamic effects of high-dose monoclonal antibody therapy in a rat model of immune thrombocytopenia. AAPS J. 2005;7(4):E895–902.
Getman KE, Balthasar JP. Pharmacokinetic effects of 4C9, an anti-FcRn antibody, in rats: implications for the use of FcRn inhibitors for the treatment of humoral autoimmune and alloimmune conditions. J Pharm Sci. 2005;94(4):718–29.
Abuqayyas L, Balthasar JP. Pharmacokinetic mAb-mAb interaction: anti-VEGF mAb decreases the distribution of anti-CEA mAb into colorectal tumor xenografts. AAPS J. 2012;14(3):445–55.
Wilhelm S, Chien DS. BAY 43–9006: preclinical data. Curr Pharm Des. 2002;8(25):2255–7.
Kim S, Yazici YD, Calzada G, Wang ZY, Younes MN, Jasser SA, et al. Sorafenib inhibits the angiogenesis and growth of orthotopic anaplastic thyroid carcinoma xenografts in nude mice. Mol Cancer Ther. 2007;6(6):1785–92.
Wilhelm SM, Carter C, Tang L, Wilkie D, McNabola A, Rong H, et al. BAY 43–9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004;64(19):7099–109.
Larkin JM, Ferguson TR, Pickering LM, Edmonds K, James MG, Thomas K, et al. A phase I/II trial of sorafenib and infliximab in advanced renal cell carcinoma. Br J Cancer. 2010;103(8):1149–53.
Galal KM, Khaled Z, Mourad AM. Role of cetuximab and sorafenib in treatment of metastatic colorectal cancer. Indian J Cancer. 2011;48(1):47–54.
Marsh AM, Lo L, Cohen RA, Feusner JH. Sorafenib and bevacizumab for recurrent metastatic hepatoblastoma: stable radiographic disease with decreased AFP. Pediatr Blood Cancer. 2012;59(5):939–40.
Castellano D, Capdevila J, Sastre J, Alonso V, Llanos M, Garcia-Carbonero R, et al. Sorafenib and bevacizumab combination targeted therapy in advanced neuroendocrine tumour: a phase II study of Spanish Neuroendocrine Tumour Group (GETNE0801). Eur J Cancer. 2013;49(18):3780–7.
Cheng AL, Kang YK, He AR, Lim HY, Ryoo BY, Hung CH, et al. Safety and efficacy of tigatuzumab plus sorafenib as first-line therapy in subjects with advanced hepatocellular carcinoma: a phase 2 randomized study. J Hepatol. 2015;63(4):896–904.
Zhu AX, Park JO, Ryoo BY, Yen CJ, Poon R, Pastorelli D, et al. Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2015;16(7):859–70.
Galanis E, Anderson SK, Lafky JM, Uhm JH, Giannini C, Kumar SK, et al. Phase II study of bevacizumab in combination with sorafenib in recurrent glioblastoma (N0776): a north central cancer treatment group trial. Clin Cancer Res. 2013;19(17):4816–23.
Hefta LJ, Neumaier M, Shively JE. Kinetic and affinity constants of epitope specific anti-carcinoembryonic antigen (CEA) monoclonal antibodies for CEA and engineered CEA domain constructs. Immunotechnology. 1998;4(1):49–57.
Sorafenib Tosylate; Product Datasheet; Santa Cruz Biotechnology: Dallas, TX, [cited 2016 Jan 6]; Available from: http://www.scbt.com/datasheet-357801.html.
Sharma A, Trivedi NR, Zimmerman MA, Tuveson DA, Smith CD, Robertson GP. Mutant V599EB-Raf regulates growth and vascular development of malignant melanoma tumors. Cancer Res. 2005;65(6):2412–21.
Jensenius JC, Williams AF. The binding of anti-immunoglobulin antibodies to rat thymocytes and thoracic duct lymphocytes. Eur J Immunol. 1974;4(2):91–7.
Urva SR, Yang VC, Balthasar JP. Physiologically based pharmacokinetic model for T84.66: a monoclonal anti-CEA antibody. J Pharm Sci. 2010;99(3):1582–600.
Shah DK, Shin BS, Veith J, Toth K, Bernacki RJ, Balthasar JP. Use of an anti-vascular endothelial growth factor antibody in a pharmacokinetic strategy to increase the efficacy of intraperitoneal chemotherapy. J Pharmacol Exp Ther. 2009;329(2):580–91.
Reichman HR, Farrell CL, Del Maestro RF. Effects of steroids and nonsteroid anti-inflammatory agents on vascular permeability in a rat glioma model. J Neurosurg. 1986;65(2):233–7.
Abuqayyas L, Balthasar JP. Investigation of the role of FcgammaR and FcRn in mAb distribution to the brain. Mol Pharm. 2013;10(5):1505–13.
Garg A, Balthasar JP. Investigation of the influence of FcRn on the distribution of IgG to the brain. AAPS J. 2009;11(3):553–7.
Nedelman JR, Gibiansky E, Lau DT. Applying Bailer’s method for AUC confidence intervals to sparse sampling. Pharm Res. 1995;12(1):124–8.
Motulsky H. Intuitive biostatistics. 1st ed. New York: Oxford University Press; 1995;17(23):2804–5.
Abuqayyas L. Evaluation of the mechanistic determinants of antibody exposure in tissues [Ph.D. Thesis]: State University of New York at Buffalo; 2012.
Ma J, Waxman DJ. Combination of anti-angiogenesis with chemotherapy for more effective cancer treatment. Mol Cancer Ther. 2008;7(12):3670–84.
Goel S, Duda DG, Xu L, Munn LL, Boucher Y, Fukumura D, et al. Normalization of the vasculature for treatment of cancer and other diseases. Physiol Rev. 2011;91(3):1071–121.
Jain RK. Normalizing tumor vasculature with anti-angiogenic therapy: a new paradigm for combination therapy. Nat Med. 2001;7(9):987–9.
Shah DK, Veith J, Bernacki RJ, Balthasar JP. Evaluation of combined bevacizumab and intraperitoneal carboplatin or paclitaxel therapy in a mouse model of ovarian cancer. Cancer Chemother Pharmacol. 2011;68(4):951–8.
Jain RK. Delivery of molecular and cellular medicine to solid tumors. Adv Drug Deliv Rev. 2012;64:353–65.
Thurber GM, Schmidt MM, Wittrup KD. Antibody tumor penetration: transport opposed by systemic and antigen-mediated clearance. Adv Drug Deliv Rev. 2008;60(12):1421.
Thurber GM, Schmidt MM, Wittrup KD. Factors determining antibody distribution in tumors. Trends Pharmacol Sci. 2008;29(2):57.
Pastuskovas CV, Mundo EE, Williams SP, Nayak TK, Ho J, Ulufatu S, et al. Effects of anti-VEGF on pharmacokinetics, biodistribution, and tumor penetration of trastuzumab in a preclinical breast cancer model. Mol Cancer Ther. 2012;11(3):752–62.
Jain RK. Physiological barriers to delivery of monoclonal antibodies and other macromolecules in tumors. Cancer Res. 1990;50(3 Suppl):814s-9s.
Acknowledgments
The authors thank Pathology Resource Network of Roswell Park Cancer Institute for the technical assistance with the IHC analysis. We also thank Maureen Adolf for her help in the iodination of T84.66. This work was supported by funding from the UB Center for Protein Therapeutics.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplemental Fig. 1
(JPG 165 kb)
Supplemental Table I
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Thomas, V.A., Balthasar, J.P. Sorafenib Decreases Tumor Exposure to an Anti-carcinoembryonic Antigen Monoclonal Antibody in a Mouse Model of Colorectal Cancer. AAPS J 18, 923–932 (2016). https://doi.org/10.1208/s12248-016-9909-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-016-9909-y