Abstract
A dissolution method for benzoyl metronidazole (BMZ) oral suspensions was developed and validated using a high-performance liquid chromatography (HPLC) method. After determination of sink conditions, dissolution profiles were evaluated using different dissolution media and agitation speeds. The sample insertion mode in dissolution media was also evaluated. The best conditions were obtained using a paddle, 50 rpm stirring speed, simulated gastric fluid (without pepsin) as the dissolution medium, and sample insertion by a syringe. These conditions were suitable for providing sink conditions and discriminatory power between different formulations. Through the tested conditions, the results can be considered specific, linear, precise, accurate, and robust. The dissolution profiles of five samples were compared using the similarity factor (f 2) and dissolution efficiency. The dissolution kinetics were evaluated and described by the Weibull model. Whereas there is no monograph for this pharmaceutical formulation, the dissolution method proposed can be considered suitable for quality control and dissolution profile comparison of different commercial formulations.
Similar content being viewed by others
INTRODUCTION
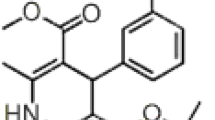
Benzoyl metronidazole (BMZ) is a 5-nitroimidazole bioactive compound used as an antiparasitic and antibacterial therapeutic agent. This drug shows biological effects against Gram-negative and Gram-positive bacteria strains, especially against microaerophilic and anaerobic cocci (1–3). BMZ is an ester derivative of metronidazole which presents a bland taste compared to the bitter taste of metronidazole free base, which allows greater patient acceptance (4). Therefore, formulations of oral suspensions have been developed for this purpose. BMZ presents poor solubility in water (3) and partition coefficient (octanol/water) greater than 2.10, which indicates high hydrophobicity. This drug has a bioavailability of approximately 80% (5). Based on BMZ solubility and absorption characteristics, it may be indicated as a drug class IV in the Biopharmaceutics Classification System (BCS), which is considered poorly soluble and poorly permeable (6). In the case of BCS class IV drugs, the dissolution is dependent on the acidic or basic nature of the drug, solubility, and formulation factors (7). Therefore, drugs in this class may have problems with dissolution which can restrict in vivo absorption (8). Poorly soluble pediatric drugs, such as BMZ oral suspension, still have additional biopharmaceutical risks for pediatric patients considering the taste-masking technology. The taste-masking technology may cause dissolution rate-limiting effects and increase the risk of differences in bioavailability (9). This way, dissolution in vitro studies are important and can be applied in the pharmaceutical development stage, as an important tool to evaluate the quality control of pharmaceutical formulations and biopharmaceutical characteristics. Also, this may be relevant to the prediction of in vivo performance (10,11). In addition to the factors mentioned above, several others can interfere with the dissolution of drugs from pharmaceutical suspensions, such as crystal form, particle size, viscosity, excipients, and the sample insertion method (12–14). The studies of these conditions are important for developing discriminative dissolution methods.
As there are few studies concerning BMZ oral suspension and there is no dissolution method for this formulation reported in official monographs, this paper proposes a discriminative dissolution method for BMZ oral suspensions with different physicochemical characteristics. Different oral suspension formulations were compared by applying the independent model method, similarity factor (f 2), and dissolution efficiency (%DE). The dissolution kinetics was determined using model-dependent approaches.
MATERIALS AND METHODS
Chemicals and Reagents
BMZ reference substance was provided by Prati-Donaduzzi Pharmaceutical Industry (Brazil). Five commercial oral suspensions of BMZ were obtained from different manufacturers and identified by letters. The reference product Flagyl® 4% (Sanofi-Aventis Pharmaceutical) was identified as A and generic products were denoted B, C, D, and E. Placebo was composed with the same excipients as described by the reference product. All excipients contained in dosage forms (monobasic sodium phosphate anhydrous, methylparaben, propylparaben, aluminum magnesium silicate, ethyl alcohol 96°C, sodium saccharin dihydrate, lemon essence, orange essence, liquid sucrose, and purified water) were of pharmaceutical grade and acquired from different distributors. Water was purified by Milli-Q® Plus system (Millipore, Billerica, USA). Methanol, acetonitrile, and triethylamine were of high-performance liquid chromatography (HPLC) grade. All the other reagents and solvents were of analytical grade. Nylon filters (0.45 μm) from Millipore Millex® and quantitative filters (25 μm) from Framex® were used in the filtration procedures. All dissolution media were prepared using the recommended procedures in the United States Pharmacopoeia (USP) (15).
Particle Size Analysis
BMZ particle size distribution was performed by laser diffraction using Malvern Mastersizer® 2000 - Hydro MS module (Worcestershire, UK). Distilled water was used as a dispersing media at 1500 rpm.
Viscosity Measurements
BMZ viscosity measurements were recorded using a Brookfield DV-II + PRO model rotational viscometer with spindle SC4-21. Data were handled using Rheocalc 3.2 software. Rheograms were obtained using data from stress and shear rate at 15–175 rpm. Samples were evaluated using power laws, Bingham, Casson, and Herschel-Bulkley models (16).
HPLC Analysis
Chromatographic analysis was performed using Prominence Liquid Chromatography Shimadzu (Kyoto, Japan) equipped with SPD-20AT PDA detector, LC-20AT pump, automatic injector SIL-20, and LC Solution V. 1.24 SP1 software. Separation was carried out at ambient temperature using C18 Nucleodur 100 column (150 × 4.0 mm, 5 μm). Mobile phase was a mixture of 0.1% phosphoric acid pH 3.0 (adjusted with triethylamine)/methanol (50:50 v/v). The mobile phase deaeration was carried out in Unique® model USC 2850 ultrasonic bath (São Paulo, Brazil). The flow rate was 1.0 mL/min and the injection volume was 10 μL. The detector was set at 235 nm and peak areas were integrated automatically by a computer using a Chemstation® software program (Agilent Technologies Inc., CA, USA).
BMZ Solubility Study
The BMZ solubility was evaluated in different dissolution media in order to ensure sink conditions during the dissolution test. The solubility studies were performed in an orbital shaking platform for 24 h with controlled stirring at 100 rpm and a temperature of 37 ± 1°C. After filtration, the solutions were diluted and analyzed by HPLC. The solubility in media was determined in triplicate. The media tested were 0.1 mol L−1 hydrochloric acid (HCl); 0.1 mol L−1 HCl with 0.1%, 0.5%, and 1.0% sodium lauryl sulfate (SLS) (w/v); 0.1 mol L−1 HCl with 0.1%, 0.5%, and 1.0% polysorbate 80 (POL80) (w/v); simulated gastric fluid (SGF) pH 1.2 (with pepsin); SGF pH 1.2 (without pepsin); 0.01 mol L−1 HCl; 0.01 mol L−1 HCl with 1.0% SLS (w/v); acetate buffer (AB) pH 4.5; AB pH 4.5 with 1.0% SLS (w/v); phosphate buffer (PB) pH 5.8; PB pH 5.8 with 1.0% SLS (w/v); PB pH 6.8; PB pH 6.8 with 1.0% SLS (w/v); simulated intestinal fluid (SIF) pH 7.5 (without pancreatin); and SIF pH 7.5 (without pancreatin) with 1.0% SLS (w/v).
Sink condition was calculated as C s/C d, where C s is the saturation solubility of BMZ in 900 mL of dissolution media and C d is the dose of BMZ in an oral formulation suspension (200 mg/5 mL) (17). Dissolution media with C s/C d ≅ 3 were considered suitable and tested during the method development.
Dissolution Method Development
The dissolution test was performed using Dissolutor Varian® (Palo Alto, USA) model VK 7000 equipped with eight vessels. Dissolution study was performed in 900 mL dissolution media at 37 ± 0.5°C, using paddles (USP apparatus 2). The agitation speed of 50 rpm was tested using the reference product (A). The dissolution media tested were 0.1 mol L−1 HCl; 0.1 mol L−1 HCl with 0.1%, 0.5%, and 1.0% SLS (w/v); 0.1 mol L−1 HCl with 0.1%, 0.5%, and 1.0% POL80 (w/v); SGF pH 1.2 (with pepsin); SGF pH 1.2 (without pepsin); 0.01 mol L−1 HCl with 1.0% SLS (w/v); and AB pH 4.5 with 1% SLS (w/v). Agitation speed of 25 rpm was tested using product A in 0.1 mol L−1 HCl and SGF pH 1.2 (without pepsin). Dissolution media without surfactant were previously deaerated in an ultrasonic bath for 20 min.
Samples were introduced into the vessel via syringes in weight equivalent to dose (200 mg/5 mL). Aliquots of 10 mL were collected manually at 5, 10, 15, 30, 45, 60, and 90 min with the subsequent replacement of the medium. For analytical determinations, the samples were filtered and diluted with methanol/water (50:50 v/v) to obtain the final concentration of 35.56 μg mL−1. After this procedure, samples were analyzed by HPLC (n = 6).
Sample Insertion Mode
The BMZ oral suspension insertion method in selected dissolution medium was evaluated using product A and an agitation speed of 50 rpm using media with deaeration. Dissolution profiles were performed under conditions that were previously selected using two sample insertions: (a) with syringes and (b) apparatus PTFE suspension cups (unofficial) marketed by Agilent Technologies (n = 6). Comparative statistical analysis of two insertion modes was performed using Student’s t test (p < 0.05).
Solution Stability
BMZ oral suspension stability in the dissolution medium tested was evaluated. Sample aliquots were withdrawn at the end of the dissolution test and analyzed immediately (zero time) and after 24 h by HPLC. The solutions were kept at room temperature (25 ± 1°C) and protected from light (n = 3).
Dissolution Method Validation
The dissolution method was validated with the following parameters evaluated: specificity, linearity, accuracy, precision, and robustness (15,18). BMZ adsorbed in filters was also verified using standard solutions (19). The HPLC method was used to analyze BMZ release in dissolution medium.
Specificity was determined by preparing a placebo solution (consisted of all excipients of the reference product without drug). An amount equivalent to a dose (5 mL) of the reference product and the placebo solution were transferred to separate vessels with 900 mL of the dissolution media at 37 ± 0.5°C and stirred for 60 min at 50 rpm, using paddles. Solution aliquots were collected and diluted in methanol/water (50:50 v/v), followed by filtration and analysis by HPLC.
Linearity was evaluated in the range 3.56–44.45 μg mL−1 using BMZ standard stock solution in dissolution media. Linearity was estimated using linear regression analysis, calculated by the least square regression method and analysis of variance (ANOVA). All analyses were performed in triplicate.
Precision was evaluated by the analysis of six samples of BMZ oral suspension samples subjected to the dissolution test. The samples were introduced in a vessel containing dissolution media using syringes (n = 6). The repeatability and intermediate precision were evaluated by relative standard deviation (RSD) obtained from the percentage of drug dissolved on different days and by different analysts.
Accuracy was evaluated by recovery of known amounts of BMZ added to the placebo solution and subjected to the dissolution test. The final concentrations were 3.56, 17.78, and 42.67 μg mL−1, which corresponded to 10.0%, 50.0%, and 120.0% of the nominal assay concentrations, respectively. Samples were added to vessels containing dissolution media and were collected after 1 h and analyzed using HPLC.
Robustness was evaluated by deliberate changes in media deaeration. Samples were subjected to the dissolution test with insertion by syringes using media with and without deaeration. Comparative statistical analysis of two media was performed using Student’s t test (p < 0.05).
Drug adsorption on the filter surface used was also evaluated by preparing standard solutions at 3.56 and 35.56 μg mL−1 concentrations (10% and 100% of BMZ theoretical concentration, respectively) in dissolution media. The filtration procedure was the same as that employed in the dissolution test, with 25 μm filter paper and a nylon membrane with a filter pore size of 0.45 μm (n = 3).
Comparison of Dissolution Profiles
Dissolution profiles of the five formulations from different manufacturers were compared by f 2 and %DE. Dissolution profiles were considered similar when the f 2 value was greater than 50 (6,20).
Dissolution efficiency was calculated using the area under the curve (AUC) of dissolution profile at time t (90 min), applying the trapezoidal method (20). %DE values were compared by ANOVA and post hoc Tukey’s test.
Kinetic Release
The mathematical models zero order, first order, Higuchi, Hixson-Crowell, and Weibull were applied to analyze BMZ release kinetics (20,21). Curves were constructed applying the models described. The kinetic model suitable for demonstrating the BMZ dissolution profile was selected based on determination coefficient (R 2).
RESULTS AND DISCUSSION
Particle Size and Viscosity
Particle size and viscosity are parameters that can influence the dissolution rate in oral suspensions (13,22) and can be used to evaluate discriminative power during the dissolution method development. In this way, these parameters were analyzed for commercial samples, the results of which are shown in Table I.
The BMZ suspensions are commercially available in anhydrous form. According to Hoelgaard and Moller, an increase in BMZ particle size in aqueous suspension occurs due to the conversion of the anhydrous form to monohydrate. The conversion to monohydrate form only has been registered in oral suspensions stored at 4°C for about 3 months, and the suspension stored at 22°C did not show any modification (23).
In particle size analysis, the samples showed different sizes (32.85–112.05 μm) which may be assigned to the intrinsic characteristic of each formulation, since they were obtained from different manufacturers. Moreover, all samples were kept at room temperature (15–30°C).
In rheological analysis, all five samples evaluated were characterized as pseudoplastic fluid (n < 1). It was found that the Hershel-Bulkley model was suitable to predict the flow behavior of the suspension samples. The Herschel-Bulkley model is a three parameter model described by τ = τ o + Kγ n, where τ o = yield stress, τ = shear stress, n = index of flow, K = index of consistency, and γ = shear rate (16). Consistency index (K) is an indicator of viscosity and describes the rheological behavior of complex fluids. It was observed that there is an increase of K values when the particle size increased, independent of the excipients present in the formulations. The hysteresis loop of B, C, and E revealed that these samples exhibited a thixotropic behavior. The loop area designates the energy needed to break down the structure that is not restored during the experimentation period and depends on the nature of the sample (24).
The presence of excipients in the formulations can also influence the dissolution rate. Table I describes the main excipients that comprise the formulation of the five products analyzed. In contrast to the reference product (A), all the other samples present POL80, which is a surfactant used for wetting solid particles and which may facilitate the dissolution process.
BMZ Solubility Study
The solubility of a drug is a key step for dissolution media selection and the determination of sink conditions. Sink conditions can be achieved when media volume reaches at least three times the volume required to form a saturated drug solution (15). Aqueous solutions containing surfactant can be used as dissolution media to achieve sink conditions for poorly soluble drugs. Surfactant amount should be evaluated to identify the minimum concentration necessary to obtain sink conditions (15). BMZ solubility and sink conditions in different media were determined, the results of which are shown in Table II.
BMZ is a weak base that shows pH-dependent solubility. It can be seen that solubility decreases in media with pH ≥ 4.5, without considering the addition of surfactant. On the other hand, the addition of SLS surfactant caused a solubility increase for the media with pH ≥ 4.5. However, up to pH ≥ 5.8, the addition of surfactant was not sufficient to achieve sink conditions (C s ≅ 3.0).
Dissolution Method Development
During method development, parameters such as apparatus, agitation speed, and dissolution media should be evaluated. For pharmaceutical form suspensions, agitation speed and sample introduction into the vessel must be selected based on viscosity (12,25). The U.S. Pharmacopoeia recommends a paddle and an agitation speed of 25 rpm (low-viscosity samples) or 50 rpm (high-viscosity samples). In the selection of the dissolution medium, the solubility of the drug and sink conditions need to be considered. Furthermore, it is important that the dissolution medium also presents a good discriminating power and biorelevant composition.
For the choice of the dissolution medium, the media that demonstrated adequate solubility and sink conditions were tested (Table II). The media 0.01 mol L−1 HCl with 1.0% SLS (w/v) and AB pH 4.5 with 1.0% SLS (w/v) resulted in a profile which initially showed a rapid dissolution rate. However, these were discarded prior to further studies as they did not result in the complete dissolution of the drug at the end point (data not shown).
In Fig. 1, the dissolution profiles obtained with product A using the following media are presented: 0.1 mol L−1 HCl surfactant-free, 0.1 mol L−1 HCl with SLS (Fig. 1a) and 0.1 mol L−1 HCl with POL80 (Fig. 1b). These media do not present differences in solubility associated with increasing concentrations of the surfactant (Table II); however, they were tested to see whether there were differences in the percentages of dissolved drug. Dissolution profiles in 0.1 mol L−1 HCl were slower than those containing SLS. However, the final percentage dissolved was similar for all (Fig. 1a).
In Fig. 1b, it is possible to observe the similarity between the profiles obtained with the dissolution media 0.1 mol L−1 HCl surfactant-free and 0.1 mol L−1 HCl + 1.0% POL80. Regarding the dissolution profiles using the media 0.1 mol L−1 HCl surfactant-free and in the presence of surfactants POL80 and SLS, it was found that the addition of surfactants to media produced small changes compared to surfactant-free media. Thus, the addition of surfactants to 0.1 mol L−1 HCl medium was demonstrated not to be necessary, considering that whenever possible, the addition of surfactants should be avoided.
Figure 2 shows the dissolution profiles obtained with product A using SGF pH 1.2 (with pepsin), SGF pH 1.2 (without pepsin), and 0.1 mol L−1 HCl media at a stirring speed of 50 rpm. The dissolution medium SGF pH 1.2 (without pepsin) produced a gradual and complete dissolution, similar to 0.1 mol L−1 HCl medium (f 2 = 61.25). However, the SGF pH 1.2 (with pepsin) medium did not produce a suitable profile since BMZ showed incomplete dissolution.
Dissolution media 0.1 mol L−1 HCl and SGF pH 1.2 (without pepsin) have been shown to be the most appropriate for the dissolution of product A. In this way, agitation speed and discriminative power were tested using both media in order to evaluate the influence of these parameters on dissolution profiles. Agitation speeds of 25 and 50 rpm were tested using product A, as shown in Fig. 3.
The decrease in agitation speed from 50 to 25 rpm provided lower hydrodynamic forces, which generated a slow dissolution rate, with a dissolved percentage of approximately 60% within 30 min of the test, observed with both media. Therefore, the agitation speed 50 rpm was chosen.
In order to evaluate the discriminative power of the method, dissolution profiles of products A and B in 0.1 mol L−1 HCl and SGF pH 1.2 (without pepsin) were compared (f 2) (Fig. 4). Product B was chosen due to the different particle sizes and viscosity characteristics in relation to product A. Both media using product B showed slower and incomplete BMZ dissolution rates compared to the dissolution profile obtained with product A. This result can be attributed to differences in particle size and viscosity between products A and B (Table I) and indicates that the media chosen are able to discriminate products with different physicochemical properties (f 2 SGF medium = 24.74; f 2 HCl medium = 26.57).
Although the dissolution profiles obtained with product A using 0.1 mol L−1 HCl and SGF pH 1.2 (without pepsin) are similar (Fig. 2), the media SGF pH 1.2 (without pepsin) was chosen as the most suitable because it presents a more biorelevant composition.
In routine tests, time dissolution and Q value are parameters that should be established and can be inferred from dissolution profile analysis. For immediate release drugs, the dissolution time should be 30 to 60 min, and the Q value should correspond to the minimum percentage dissolution at a specified time (15). Since oral suspensions are immediate release dosage forms, a BMZ Q value ≥80 and time dissolution ≥60 min are suggested.
Sample Insertion Mode
In order to evaluate the sample insertion mode on the selected dissolution medium, dissolution profiles were performed using syringes and suspension cups. The results are shown in Table III.
Sample insertion using a syringe generated a gradual and complete dissolution with RSD in each time analysis that was lower than 10%. Sample insertion using the suspension cup apparatus resulted in incomplete dissolution (% dissolved = 54; 90 min), and the RSD for the first time analysis was higher than 10%. This method would allow a sample-controlled surface area with lower dispersion in dissolution media. However, this format (suspension cup geometry) avoided sample contact with the dissolution medium, resulting in inaccurate and incomplete dissolution (demonstrated by higher RSD values between vessels). In statistical comparative analysis, there is a significant difference between the two sample introduction methods, indicating that they are not equivalent (p < 0.05).
Solution Stability
BMZ was stable in dissolution test conditions. The results showed that the sample remained stable for 24 h (recovery = 99.35%), according to the acceptable range 98–102% (15).
Dissolution Method Validation
Dissolution method specificity shows that excipients do not interfere with the BMZ peak, since there was no other peak at the same retention time. Representative chromatograms of BMZ were used to demonstrate the specificity of the method (Fig. 5). Peak purity analysis for BMZ showed a purity of >0.9999.
Linearity was tested by analysis of BMZ standard solutions in the concentration range 3.56–44.45 μg mL−1. The method showed linear correlation (r 2 = 0.9999) and statistical analysis by ANOVA revealed a significant linear regression and no significant deviation from linearity (p > 0.05).
The precision of the dissolution method was evaluated through repeatability (intraday) and intermediate precision (interday). The low RSD (≤2%) values obtained demonstrate the good precision of the method (Table IV).
Accuracy was evaluated based on the recovery test and calculated by the ratio between the determined concentration and the theoretical concentration. Recovery from 95% to 105% is recommended for this test (15). The recovery obtained (range 99.34 ± 1.82–99.65 ± 1.62%) is lower than the recommended limit and indicates the accuracy of the method.
Robustness of the dissolution method was evaluated by the deaerating influence on dissolution media, considering that air bubbles can act as a barrier to the dissolution process (15). The results submitted to ANOVA (Table III) showed no significant difference between dissolved BMZ obtained with and without deaerated dissolution media. These data suggest that deaeration of the dissolution media does not influence the dissolution of BMZ oral suspension.
Adsorption of BMZ in filters utilized in dissolution testing was also evaluated. The results obtained showed recoveries between 100 and 102%, in accordance with the criterion for acceptable adsorption (>95%) (19). Results indicated that filters did not cause a loss of BMZ during the dissolution test.
Comparison of Dissolution Profiles
The dissolution profiles of five brands of BMZ oral suspension subjected to the same test conditions are shown in Fig. 6. Dissolution profiles were appropriate since the RSD was below the recommended limit (≥20% for the first points and ≤10% for the other ones) (6,20). The comparison of dissolution profiles for different products cited in Fig. 6 was realized. The results of f 2 are shown in Table V. Product D was excluded from comparison because it showed rapid dissolution. The complete dissolution of product D was observed in 5 min of the test, which may be attributed to the value found in particle size and viscosity and also the presence of POL80 in the formulation (Table I).
As seen in Table V, the comparison of the dissolution profiles for test products B, C, and E versus the reference (product A) using f 2 showed that only product C presented a profile similar to the reference product (f 2 > 50).
Product B presented values of particle size and viscosity higher than all the products analyzed. This fact may have contributed to the slow dissolution of BMZ even with the presence of surfactant in the formulation. As the analysis using f 2 is a qualitative determination of similarity between pairs of dissolution profiles (21), a statistical analysis of the %DE values was carried out.
In Table V, it is also possible to observe the %DE value of the reference product and of products B, C, D, and E. Product D showed a higher DE value (93.96%), in accordance with the rapid dissolution rate observed. The statistical analysis showed a significant difference (p < 0.05) in the dissolution profile of the reference product in relation to the dissolution profiles of the other products. Differences between the results using f 2 and %DE may occur because different calculation methods were used for analyzing the dissolution profiles. The FDA recommended f 2; however, ANOVA-based methods have narrower limits and are more discriminative than f 2. The similarity factor and %DE are two different methods of analyzing dissolution profiles which can be applied and are useful (21,26).
Evaluation of Release Kinetics
The zero-order, first-order, Higuchi, Hixson-Crowell, and Weibull models were applied to describe the drug release kinetics. The Weibull model showed a higher determination coefficient (Table VI) and was considered appropriate for describing drug release kinetics. For this model, the logarithm of the amount of drug dissolved versus the logarithm of time is linear and demonstrates the cumulative fraction of a drug in a given time (20).
The β parameter characterizes the shape of the curve and was determined from the Weibull equation obtained for each product. Values for β = 1 indicate curve exponential, β > 1 shows a sigmoid curve, and β < 1 is characterized as a parabolic curve (20,27,28). The β parameter calculated for BMZ oral suspensions was lower than 1 (Table VI), which indicates parabolic curves with initial inflection. The parabolic curves are common in suspensions that release the drug quickly in early times of dissolution and then remain at a constant dissolution (28).
CONCLUSIONS
Pharmaceutical suspensions are dispersed systems which can have problems with their dissolution which may compromise drug bioavailability. In this study, a dissolution method was developed and applied to investigate the release profiles of BMZ from suspensions. Pharmaceutical factors such as particle size, system viscosity, and excipients are interdependent and contribute to differences obtained in dissolution profiles. The method proposed showed discriminatory power and can be used in the quality control for BMZ oral suspensions since there is no monograph for the pharmaceutical form in any official compendia. Moreover, this method can be used in studies concerning the pharmaceutical equivalence to BMZ in this dosage form.
REFERENCES
Turgut EH, Özyazici M. Bioavailability file: metronidazole. FABAD J Pharm Sci. 2004;29(1):39–49.
Harris JC, Plummer S, Lloyd D. Antigiardial drugs. Appl Microbiol Biotechnol. 2001;57(5-6):614–9.
Bempong DK, Manning RG, Mirza T, Bhattacharyya L. A stability-indicating HPLC assay for metronidazole benzoate. J Pharm Biomed Anal. 2005;38(4):776–80.
Vu NT, Aloumanis V, Ben MJ, Kupiec TC, Patterson EK, Radke J. Stability of metronidazole benzoate in SyrSpend SF one-step suspension system. Int J Pharm Compd. 2008;12(6):558–64.
Houghton GW. A comparison of the pharmacokinetics of metronidazole in man after oral administration of single doses of benzoylmetronidazole and metronidazole. Br J Clin Pharmacol. 1982;14(2):201–6.
FDA. Guidance for industry: waiver of in vivo bioavailability and bioequivalence studies for immediate-release solid oral dosage forms based on a Biopharmaceutics Classification System. U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER); May 2015. http://www.fda.gov/downloads/Drugs/Guidances/ucm070246.pdf
Tsume Y, Mudie DM, Langguth P, Amidon GE, Amidon GL. The Biopharmaceutics Classification System: subclasses for in vivo predictive dissolution (IPD) methodology and IVIVC. Eur J Pharm Sci. 2014;57:152–63.
Bredael GM, Bowers N, Boulineau F, Hahn D. In vitro–in vivo correlation strategy applied to an immediate-release solid oral dosage form with a biopharmaceutical classification system iv compound case study. J Pharm Sci. 2014;103(7):2125–30.
Purohit VS. Biopharmaceutic planning in pediatric drug development. AAPS J. 2012;14(3):519–22.
Bajerski L, Rossi RC, Dias CL, Bergold AM, Fröehlich PE. Development and validation of a discriminating in vitro dissolution method for a poorly soluble drug, olmesartan medoxomil: comparison between commercial tablets. AAPS PharmSciTech. 2010;11(2):637–44.
Dressman JB, Amidon GL, Reppas C, Shah VP. Dissolution testing as a prognostic tool for oral drug absorption: immediate release dosage forms. Pharm Res. 1998;15:11–22.
Brown CK, Friedel HD, Barker AR, Buhse LF, Keitel S, Cecil TL, et al. FIP/AAPS joint workshop report: dissolution/in vitro release testing of novel/special dosage forms. AAPS PharmSciTech. 2011;12(2):782–94.
Fonseca LB, Labastie M, Sousa VP, Volpato NM. Development and validation of a discriminative dissolution test for nimesulide suspensions. AAPS PharmSciTech. 2009;10(4):1145–52.
Bisrat M, Nyström C. Physicochemical aspects of drug release. VIII. The relation between particle size and surface specific dissolution rate in agitated suspensions. Int J Pharm. 1988;47:223–31.
The United States Pharmacopeia, 36th ed., and The National Formulary, 31st ed. 36 ed. Rockville, MD: United States Pharmacopeial Convention, Inc.; 2013.
Alves MP, Pohlmann AR, Guterres SS. Semisolid topical formulations containing nimesulide-loaded nanocapsules, nanospheres or nanoemulsion: development and rheological characterization. Pharmazie. 2005;60(12):900–4.
Priya MBV, Murthy TEGK. Development of discriminative dissolution media for marketed gliclazide modified-release tablets. Dissolut Technol. 2012;19(2):38–42.
ICH, validation of analytical procedures: text and methodology (Q2R1), in International Conference on Harmonization; November 2005.
Lindenberg M, Wiegand C, Dressman JB. Comparison of the adsorption of several drugs to typical filter materials. Dissolut Technol. 2005;12(1):22–5.
Costa P, Lobo JMS. Modeling and comparison of dissolution profiles. Eur J Pharm Sci. 2001;13(2):123–33.
Yuksel N, Kanık AE, Baykara T. Comparison of in vitro dissolution profiles by ANOVA-based, model-dependent and -independent methods. Int J Pharm. 2000;209(1-2):57–67.
Bernal NP, Calpenal AC, Mallandrich M, Ruiz A, Clares B. Development, physical-chemical stability, and release studies of four alcohol-free spironolactone suspensions for use in pediatrics. Dissolut Technol. 2014;21(1):19–30.
Hoelgaard A, Moller N. Hydrate formation of metronidazole benzoate in aqueous suspensions. Int J Pharm. 1983;15(2):213–21.
Roopa BS, Bhattacharya S. Characterization and modeling of time-independent and time-dependent flow behavior of sodium alginate dispersions. Int J Food Sci Technol. 2009;44(12):2583–9.
Vaghela B, Kayastha R, Bhatt N, Pathak N, Rathod D. Development and validation of dissolution procedures. J Appl Pharm Sci. 2011;1(3):50–6.
Anderson NH, Bauer M, Boussac N, Khan-Malek R, Munden P, Sardaro M. An evaluation of fit factors and dissolution efficiency for the comparison of in vitro dissolution profiles. J Pharm Biomed Anal. 1998;17:811–22.
Adams E, Coomans D, Smeyers-Verbeke J, Massart DL. Non-linear mixed effects models for the evaluation of dissolution profiles. Int J Pharm. 2002;240(1-2):37–53.
Papadopouloi V, Kosmidis K, Vlachou M, Macheras P. On the use of the Weibull function for the discernment of drug release mechanisms. Int J Pharm. 2006;309(1-2):44–50.
ACKNOWLEDGMENTS
We acknowledge the Prati-Donaduzzi Pharmaceutical Industry (Brazil) for the kind donation of the BMZ reference substance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
da Silva, A.S., da Rosa Silva, C.E., Paula, F.R. et al. Discriminative Dissolution Method for Benzoyl Metronidazole Oral Suspension. AAPS PharmSciTech 17, 778–786 (2016). https://doi.org/10.1208/s12249-015-0407-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-015-0407-9