Abstract
Background
The relationship between extent of cervical lymphadenectomy along with the number of involved lymph nodes (LNs) removed and overall survival has not been well documented in patients with medullary thyroid carcinoma (MTC). This study investigates whether the overall number of LNs removed and the number of metastatic LNs are independent prognostic factors for overall survival.
Methods
Data from patients with MTC in the Surveillance, Epidemiology, and End Results (SEER) registry database were examined. After categorizing the study population based on the number of overall LNs examined and the number of metastatic LNs, survival estimates were compared. The total number of examined LNs and their histopathological status were analyzed for their prognostic value in estimating overall survival.
Results
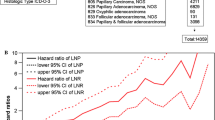
593 patients were included in this study. Those with all negative LNs had the best overall survival; those with LNs examined and at least one positive LN had worst overall survival (p < 0.0001). The total number of examined LNs for both groups with negative and positive LNs was not associated with improved survival outcome (p = 0.41). In node-positive patients, each additional positive LN was significantly associated with an increase in overall mortality [hazard ratio (HR) = 1.05, 95% confidence interval (CI) = 1.02–1.08].
Conclusions
Cervical LN metastases conferred an independent risk for worse survival rate in MTC. Cervical lymphadenectomy is important for staging and regional disease control, however the extent of lymph node dissection, the overall number of lymph nodes removed along with removal of an increased number of involved lymph nodes do not confer a survival advantage. Future prospective studies are needed.


Similar content being viewed by others
References
Harris PE. The management of thyroid cancer in adults: a review of new guidelines. Clin Med. 2002;2(2):144–6.
Kendall-Taylor P, Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf). 2003;58(4):400–2.
American Thyroid Association Guidelines Task Force, Kloos RT, et al. Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid. 2009;19(6):565–612.
National Comprehensive Cancer Network. Practice guidelines in oncology/thyroid carcinoma. Available at http://www.nccn.org/professionals/physician_gls/PDF/thyroid.pdf. Accessed 26 October 2010.
Franc S, et al. Complete surgical lymph node resection does not prevent authentic recurrences of medullary thyroid carcinoma. Clin Endocrinol (Oxf). 2001;55(3):403–9.
Chen H, et al. Effective long-term palliation of symptomatic, incurable metastatic medullary thyroid cancer by operative resection. Ann Surg. 1998;227(6):887–95.
Kebebew E, et al. Extent of disease and practice patterns for medullary thyroid cancer. J Am Coll Surg. 2005;200(6):890–6.
National Cancer Institute D, SRP, Cancer Statistics Branch. Available at http://seer.cancer.gov/about/. Accessed 26 October 2010.
Ball DW. Medullary thyroid cancer, monitoring and therapy. Endocrinol Metab Clin North Am. 2007;36(3):823–37.
Saad MF, et al. Medullary carcinoma of the thyroid. A study of the clinical features and prognostic factors in 161 patients. Medicine (Baltimore). 1984;63(6):319–42.
Gharib H, et al. American Association of Clinical Endocrinologists and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocr Pract. 2006;12(1):63–102.
Roman S, Lin R, Sosa JA. Prognosis of medullary thyroid carcinoma: demographic, clinical, and pathologic predictors of survival in 1252 cases. Cancer. 2006;107(9):2134–42.
Kebebew E, et al. Medullary thyroid carcinoma: clinical characteristics, treatment, prognostic factors, and a comparison of staging systems. Cancer. 2000;88(5):1139–48.
Pelizzo MR, et al. Natural history, diagnosis, treatment and outcome of medullary thyroid cancer: 37 years experience on 157 patients. Eur J Surg Oncol. 2007;33(4):493–7.
Fialkowski E, DeBenedetti M, Moley J. Long-term outcome of reoperations for medullary thyroid carcinoma. World J Surg. 2008;32(5):754–65.
Quayle FJ, Moley JF. Medullary thyroid carcinoma: management of lymph node metastases. Curr Treat Options Oncol. 2005;6(4):347–54.
Moley JF, et al. Reoperation for recurrent or persistent medullary thyroid cancer. Surgery. 1993;114(6):1090–5 (discussion 1095–6).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kandil, E., Gilson, M.M., Alabbas, H.H. et al. Survival Implications of Cervical Lymphadenectomy in Patients with Medullary Thyroid Cancer. Ann Surg Oncol 18, 1028–1034 (2011). https://doi.org/10.1245/s10434-010-1363-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-010-1363-y