Is clinical evaluation alone sufficient for the diagnosis of a Bankart lesion without the use of magnetic resonance imaging?
Introduction
Recurrent shoulder instability is a common condition affecting many young athletes. The stability of the shoulder joint is maintained by a deepened glenoid labrum. A torn glenoid labrum results in shoulder instability. A Bankart lesion is an injury of the glenoid labrum due to an antero-inferior shoulder dislocation, often located in the 3–6 o’clock position (1). This lesion is reported to be as high as 90% after a traumatic shoulder dislocation. Matsen described a Bankart lesion as a significant finding in a patient with anterior shoulder instability who suffered a traumatic dislocation requiring surgical correction (2).
Diagnosis of a Bankart lesion requires a detailed assessment of a patient presenting with shoulder pain, which is often accompanied by shoulder instability (3). The patient often suffers his first shoulder dislocation following a traumatic event. The proposed mechanism of injury resulting in a Bankart lesion is an impaction force in a hyperabducted and externally rotated position. With an underlying Bankart lesion, the patient will often experience recurrent dislocations, with subsequent dislocations occurring with more ease. On physical examination, anterior shoulder instability is indicated by a positive Anterior Apprehension test and Load and Shift test.
Clinical evaluation and imaging modalities can strongly suggest the presence of such lesions and aid in the preoperative planning. A diagnosis of Bankart lesion is usually confirmed intra-operatively during shoulder arthroscopy. A prospective study by Walsworth et al. found that a history of “popping” or “catching” in combination with positive findings on physical examination were highly suggestive of a labral tear (4). However, the role of imaging in the diagnosis of Bankart lesions has been met with high intra and inter-observer variability. Plain radiographs have not been helpful in the diagnosis of Bankart lesions, unless associated with a bony lesion, for example a Hill-Sachs lesion. Ultrasound has been shown to only be effective in detecting rotator cuff tears (5). The current accepted gold standard is the use of magnetic resonance imaging (MRI) for preoperative diagnosis of Bankart lesions. MRI may also be augmented with the use of contrast, as in magnetic resonance arthrogram (MRA). Studies have reported good sensitivities and specificities with these two modalities (6-8). Some studies have gone further to show the superiority of MRA over MRI in the diagnosis of labral tears (5,8,9).
Although imaging modalities such as MRA offer great utility in diagnosing Bankart lesions, they can place a huge financial burden on the patients and the healthcare system. The high degree of intra and interobserver variability between the available modalities has called into question the effectiveness of these modalities in detecting labral lesions (10). This study aims to evaluate the diagnostic accuracy of clinical evaluation and imaging modalities in Bankart lesions such as MRI and MRA of the shoulder. The authors of this study believe that the use of clinical evaluation can offer sensitivities comparable to imaging modalities.
Methods
Between February 2004 and January 2015, we retrospectively reviewed the surgical records of a tertiary hospital and identified a total of 250 patients who underwent arthroscopic Bankart repair. Centralized Institutional Review Board approval (CIRB 2015/2478) and written patient consent was obtained for this study. The inclusion criteria were patients with the diagnosis of recurrent shoulder subluxation or dislocation and a diagnosis of labra-ligamentous injury. All the patients subsequently underwent arthroscopic surgery with documented intra-operative findings. All patients were thoroughly investigated preoperatively by the senior surgeon in which a detailed history were obtained, relevant physical examinations were performed (Load and Shift/Anterior Apprehension test) with pre-operative radiographs including anterior-posterior, lateral, axillary and scapular-Y views. Some patients subsequently underwent either an MRI or an MRA scan if the initial clinical evaluation was equivocal. Postoperatively, patients were followed up regularly and any recurrence of symptoms were noted. Those patients with incomplete data were excluded from this study. There were a total of 227 patients included in the study group.
The mean age was 26±8 (range, 15–54) years, with 217 male and 10 female patients in the group. All 227 (100%) patients suffered a traumatic shoulder dislocation and the mode of injury varied among these patients. One hundred and thirty-nine (61%) patients suffered a fall onto out stretched hand (FOOSH), 83 (37%) patients suffered sports related injuries which included excessive overhead activities and 5 (2%) patients suffered a direct traumatic injury to the shoulder. All patients reported shoulder pain and 214 (94%) patients reported signs and symptoms of chronic instability. Chronic instability was defined by recurrent episodes of dislocations, sensation of shoulder subluxation or “looseness” of the shoulder joint as reported by the patient.
Anterior shoulder instability was assessed through the Anterior Apprehension test and the Load and Shift test. The Anterior Apprehension test was chosen because it demonstrated high sensitivity and specificity (11,12). The test was first performed with the patient seated upright in a clinic setting. The patient’s shoulder was first abducted to 90 degrees and the elbow flexed to 90 degrees. One hand was used to stabilize the patient’s shoulder, the other used to externally rotate the arm while observing the patient’s face for apprehension. Stabilization of the shoulder was performed by placing the thumb posteriorly and the fingers anteriorly. A positive test was indicated by a sense of apprehension.
The Load and Shift test was also chosen because it demonstrated high sensitivity and specificity (13,14). It was first performed with the patient seated upright in a clinic setting. The patient’s shoulder was first abducted to 90 degrees and the elbow flexed to 90 degrees. One hand was used to stabilize the patient’s shoulder, while the other was used to provide a compressive force onto the glenoid. The glenoid was then moved anteriorly and posteriorly and the amount of translation was documented. This test was used to assess for the degree of anterior and posterior instability.
Twenty-six of 227 patients underwent an MRI scan for the shoulder. Eighty-nine of the 227 patients underwent an MRA scan. MR imaging was performed within 45 mins after injection of the contrast material into the shoulder joint. All MRI/MRA readings were performed by an experienced musculoskeletal radiologist with more than 10 years experience in the field.
Operative arthroscopy was performed by a single senior surgeon with the use of a standardised technique. The patient was placed in a beach chair position with the shoulder draped in a sterile manner. A standard posterior viewing portal was established approximately 2 cm inferior and 1 cm medial to the acromial angle. Two anterior portals were established using the outside-in technique with a spinal needle to determine the most appropriate placement of the cannulas. The anterosuperior portal was inserted just inferior to the acromion edge while the anterior midglenoid portal was inserted over the superior border of the subscapularis tendon. Through these portals, an assessment of the glenoid labrum, rotator cuff integrity, and humeral head for Hill-Sachs lesions was performed. All Bankart lesions were repaired using three suture anchors. The reference standard for this study was the intraoperative diagnosis from the arthroscopic surgery.
Postoperatively, patients were placed in a sling for 6 weeks and taught to do basic isometric exercises. These patients were allowed full shoulder mobilization after 6 weeks and were able to return to sports after 4 months.
Statistical analysis
Statistical analysis was performed in consultation with the in-house biostatistician, using SPSS® 19.0 (IBM, Armonk, New York, United States). Sensitivities, positive predictive values (PPVs) and their respective 95% confidence interval (CI) were calculated for each of the tests.
Results
All 227 patients underwent anterior shoulder stabilisation for a Bankart lesion. Arthroscopic findings confirmed that all patients had Bankart lesion, of which there were 7 patients (3.1%) who had an osseous defect (bony Bankart), 12 patients (5.3%) who had a superior labrum anterior-posterior (SLAP) and 33 patients (15%) who had Hill-Sachs lesions (Table 1).
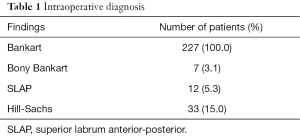
Full table
All 227 patients experienced a shoulder dislocation following a traumatic event, with 89% of these patients being under 35 years of age. On examination, the Anterior Shoulder Apprehension test and the Load and Shift test identified 214 of 227 Bankart tears, with a sensitivity of 94% (95% CI, 90–97%). For all the patients with a concurrent SLAP and Bankart lesions, physical examination was negative. Similarly, a positive history indicating chronic instability mirrored the physical examination results and trend for SLAP lesions. Thus, for all patients with concurrent SLAP and Bankart lesions, they did not experience any chronic shoulder instability and any physical examination testing for instability was also found to be negative.
In our study, MRI correctly identified 23 of 26 patients with Bankart tears, with a sensitivity of 89% (95% CI, 70–98%). There were five patients who have SLAP tears seen on MRI, however only three patients had SLAP tears seen during their arthroscopic surgery. MRA correctly identified 84 of 89 patients with Bankart tears, with a sensitivity of 94% (95% CI, 87–98%). There were 13 patients who have SLAP tear seen on MRA, but only 7 patients had SLAP tears seen during their arthroscopic surgery.
Eight patients suffered a recurrence of shoulder dislocation after their index anterior shoulder stabilisation surgery. All of the eight patients experienced symptoms of chronic instability. Subsequently, four out of eight patients underwent computed tomography (CT) scan of their shoulder and identified bone loss of at least 20% in all these patients. Only two patients required revision surgery while the remaining six were treated conservatively.
Discussion
In our study, all the patients suffered a shoulder dislocation following a traumatic event, with the commonest mode of injury a fall on the out stretched hand (61%). Another salient feature in the history is the age of the patient. Liu et al. identified that 66% of their patients with labral tears were younger than 35 years (13). This is consistent with our study, with 89% of our patients with Bankart lesions under 35 years old.
Chronic shoulder instability was assessed by determining the number of episodes, mechanism of shoulder dislocation or a sensation of “looseness” or shoulder subluxation. This study identified a sensitivity of 94% when a history of chronic instability was positive. Similarly, the results for the Anterior Apprehension and Load and Shift tests were identical to the history of chronic instability with a sensitivity of 94%. Patients presenting with recurrent shoulder dislocations from traumatic events with a positive clinical findings of Anterior Apprehension and Load and Shift tests are very likely to have a Bankart lesion.
The use of imaging modalities such as MRI and MRA of the shoulder has been useful to aid clinical evaluation of anterior shoulder instability due to Bankart lesions. Several studies reported that the variability in sensitivities reported for MRA in detecting labral lesions was in part due to the experience level of the radiologist (5,6). There is high intra- and interobserver variability with differing sensitivity levels of more than 10% when two different radiologists were asked to interpret the MR images (10). Even with use of MRA, it has been reported to have low levels of sensitivity and specificities in diagnosing labral tears, with a study showing sensitivity for MRA in detecting Bankart lesions at a dismal 58.1% (6). Liu et al. also found that clinical examination yielded a higher sensitivity, (90% vs. 59%) in detecting glenoid labral tears when compared to MRA (13).
In our study, we report high sensitivities (>90%) and PPVs (100%) for both clinical evaluation and imaging in the diagnosis of Bankart lesions (Table 2). In our patients, MRA demonstrated the highest sensitivity at 94.4% among the groups in detecting Bankart lesions, which is similar to the results of studies (15-17), which advocate MRA as the gold standard for diagnosing anterior-inferior labral lesions. The advantages of MRA over other forms of imaging are the ability to detect subtle lesions of the intra-articular structures such as the labrum and ligaments (18).
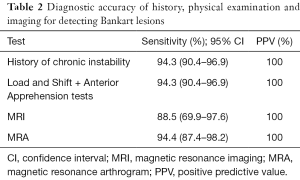
Full table
Despite being the gold standard for imaging of Bankart lesions, the use of MRA has its disadvantages such as increasing financial burden on the patient and healthcare, longer waiting times and procedure-related complications such as, contrast media side effects, allergic reactions or even extravasations, though these are rare adverse events (19). The waiting time for MRA pre-operatively can also delay the surgical management. Clinical examination with Anterior Apprehension and Load and Shift tests have been reported to have a high sensitivity and specificity for diagnosing labral lesions in multiple studies (11-13,20-22). Thus in our study, we support the use of clinical evaluation for the diagnosis of shoulder instability and we propose the use of MRA scans as an adjunct pre-operatively when the clinical evaluations are equivocal.
In the event of glenoid bone loss in Bankart lesions, additional imaging modalities such as CT scan should be used to evaluate the amount of bone loss pre-operatively. The bone loss should then be addressed during the anterior shoulder stabilisation operation as up to 89% of patients that failed soft-tissue stabilization procedures have underlying glenoid bone deficiencies (23). In our study, eight of the patients in our study had a recurrence of symptoms after arthroscopic anterior shoulder stabilisation, and four of these patients have a bony Bankart lesion identified on the CT scan.
The strengths of this study include the large number of patients available for analysis, representing the largest series (227 patients) in the existing literature to the authors’ knowledge. The study also focused only on Bankart lesions in comparison to other studies which categorized labral lesions as a whole as this could confound the results as mentioned earlier. There are some limitations in our study. Firstly, this study is a retrospective study and also selection biases as only patients who underwent arthroscopic surgery for Bankart lesion were included in the study. In addition, we were unable to obtain specificity of the clinical examination or imaging modalities as the study group only involved patients who underwent arthroscopic repair of Bankart lesion. Future prospective studies targeted at patients with a preoperative diagnosis of anterior shoulder instability can be performed to reduce these biases.
Conclusions
In our study, we report that clinical evaluation with focused history-taking and anterior apprehension, load and shift clinical examination can diagnose anterior shoulder instability as reliably as MR imaging. This saves the waiting time and financial cost from MR imaging for the patients. For patients with equivocal clinical findings, the use of MR imaging can then be used as an adjunct to aid with the diagnosis. For patients with a recurrence of symptoms necessitating a revision Bankart repair, additional imaging modalities such as CT scan can be used to evaluate underlying glenoid bone deficiencies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Centralized Institutional Review Board approval (CIRB 2015/2478) and written patient consent was obtained for this study.
References
- Owens BD, Nelson BJ, Duffey ML, et al. Pathoanatomy of first-time, traumatic, anterior glenohumeral subluxation events. J Bone Joint Surg Am 2010;92:1605-11. [Crossref] [PubMed]
- Matsen FA 3rd, Harryman DT 2nd, Sidles JA. Mechanics of glenohumeral instability. Clin Sports Med 1991;10:783-8. [PubMed]
- Hurley JA, Anderson TE. Shoulder arthroscopy: its role in evaluating shoulder disorders in the athlete. Am J Sports Med 1990;18:480-3. [Crossref] [PubMed]
- Walsworth MK, Doukas WC, Murphy KP, et al. Reliability and diagnostic accuracy of history and physical examination for diagnosing glenoid labral tears. Am J Sports Med 2008;36:162-8. [Crossref] [PubMed]
- Pavic R, Margetic P, Bensic M, et al. Diagnostic value of US, MR and MR arthrography in shoulder instability. Injury 2013;44 Suppl 3:S26-32. [Crossref] [PubMed]
- Jonas SC, Walton MJ, Sarangi PP. Is MRA an unnecessary expense in the management of a clinically unstable shoulder? A comparison of MRA and arthroscopic findings in 90 patients. Acta Orthop 2012;83:267-70. [Crossref] [PubMed]
- Li HF, Liu YJ, Cheng LQ, et al. Diagnostic value of MRI and MR arthrography in the detection of injuries of anterior labrum in shoulder. Zhongguo Gu Shang 2012;25:413-7. [PubMed]
- Palmer WE, Brown JH, Rosenthal DI. Labral-ligamentous complex of the shoulder: evaluation with MR arthrography. Radiology 1994;190:645-51. [Crossref] [PubMed]
- Chandnani VP, Yeager TD, DeBerardino T, et al. Glenoid labral tears: prospective evaluation with MRI imaging, MR arthrography, and CT arthrography. AJR Am J Roentgenol 1993;161:1229-35. [Crossref] [PubMed]
- Garneau RA, Renfrew DL, Moore TE, et al. Glenoid labrum: evaluation with MR imaging. Radiology 1991;179:519-22. [Crossref] [PubMed]
- Lo IK, Nonweiler B, Woolfrey M, et al. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. Am J Sports Med 2004;32:301-7. [Crossref] [PubMed]
- Farber AJ, Castillo R, Clough M, et al. Clinical assessment of three common tests for traumatic anterior shoulder instability. J Bone Joint Surg Am 2006;88:1467-74. [PubMed]
- Liu SH, Henry MH, Nuccion S, et al. Diagnosis of glenoid labral tears. A comparison between magnetic resonance imaging and clinical examinations. Am J Sports Med 1996;24:149-54. [Crossref] [PubMed]
- van Kampen DA, van den Berg T, van der Woude HJ, et al. Diagnostic value of patient characteristics, history, and six clinical tests for traumatic anterior shoulder instability. J Shoulder Elbow Surg 2013;22:1310-9. [Crossref] [PubMed]
- Waldt S, Burkart A, Imhoff AB, et al. Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology 2005;237:578-83. [Crossref] [PubMed]
- Flannigan B, Kursunoglu-Brahme S, Snyder S, et al. MR arthrography of the shoulder: comparison with conventional MR imaging. AJR Am J Roentgenol 1990;155:829-32. [Crossref] [PubMed]
- Green MR, Christensen KP. Magnetic resonance imaging of the glenoid labrum in anterior shoulder instability. Am J Sports Med 1994;22:493-8. [Crossref] [PubMed]
- Peh WC. Magnetic resonance arthrography of the labral-ligamentous complex of the shoulder: an update. Ann Acad Med Singapore 2002;31:614-20. [PubMed]
- Newberg AH, Munn CS, Robbins AH. Complications of arthrography. Radiology 1985;155:605-6. [Crossref] [PubMed]
- Tzannes A, Paxinos A, Callanan M, et al. An assessment of the interexaminer reliability of tests for shoulder instability. J Shoulder Elbow Surg 2004;13:18-23. [Crossref] [PubMed]
- Malhi AM, Khan R. Correlation between clinical diagnosis and arthroscopic findings of the shoulder. Postgrad Med J 2005;81:657-9. [Crossref] [PubMed]
- Mahaffey BL, Smith PA. Shoulder instability in young athletes. Am Fam Physician 1999;59:2773-82, 2787. [PubMed]
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [Crossref] [PubMed]


