
Incidence and risk factors of wound complications in long segment instrumented thoracolumbar spinal fusions: a retrospective study
Introduction
Surgical site complications following spinal surgery are a source of significant patient morbidity, increased cost, and further medical management (1). A typical treatment regimen of surgical site infections includes wound debridement, long-term antibiotic usage, and wound closure (2-6). More controversially, management may also involve removal of instrumentation (2) while some studies advocate that removal of instrumentation is not necessary in management (3,7). These interventions have been reported to increase financial burden of spinal surgery by an estimated $4,067–$36,000 per case (8,9).
To lessen the associated medical and economic complications, measures are taken to prevent surgical site infection from occurring. This includes aseptic technique, optimization of patient status, pre-operative antibiotics, and close post-operative follow-up (1,10). Of note, Staphylococcus aureus is the microbe most commonly responsible for infections after spinal surgery; however, infections can also arise from multi-microbial origin (1,4-6,11,12).
Since surgical site complications occur despite preventative measures, it is important to identify the associated risk factors. The literature reveals a wide range of patient-related risk factors that includes: diabetes, smoking, obesity, cardiovascular disease, chronic obstructive pulmonary disease, steroids, malignancy, older age, alcohol abuse, perioperative transfusion, revision surgery, American Society of Anesthesiology (ASA) class 3–5, weight loss, and Medicaid status (1,4,9,11-15). Additionally, the following intraoperative risk factors have been identified in the literature: surgical invasiveness, type of fusion, implant usage, traditional (vs. minimally invasive) approach, longer surgery, blood loss, and increased ICU stay (1,4,13,14,16-18). In the pediatric population, risk factors include procedures that extend to the pelvis or include osteotomy (19).
Many of the aforementioned risk factors have been identified in the context of spinal surgery. When broken down by procedure type, fusion with instrumentation has been found to be one of the strongest risk factors associated with wound complications (4,5,13). This association seems to exist because instrumentation can serve as a nidus for microbes (13). The current literature on the complications of medium to long segment spinal fusions is limited to studies conducted at single institutions with less than 150 cases (20-23). This is the first national study to specifically examine long segment (7+ vertebrae) instrumented thoracolumbar fusions. The objective is to identify the incidence rates, preoperative and perioperative risk factors, and associated complications of patients who develop postoperative wound complications.
Methods
This is a retrospective analysis of prospectively collected data from the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP). NSQIP is a national database consisting of preoperative, intraoperative, and 30-day postoperative variables of adult patients undergoing major surgery in the United States. It includes both inpatient and outpatient procedures, and patient data is collected on an 8-day cycle so that cases from all days of the week are included. Data is input by surgical nurses who are trained in the matter and are subject to random audits, which yielded an overall disagreement rate of 2% (24).
This study consists of a comprehensive search of the NSQIP database from January 1, 2005 to July 31, 2014. Inclusion entailed a Current Procedural Terminology (CPT) code corresponding to posterior segmental instrumentation (e.g., pedicle fixation, dual rods with multiple hooks and sublaminar wires) expanding either 7 to 12 vertebral segments, or 13 or more vertebral segments (CPT codes 22843 and 22844). It was not required that this was the primary CPT code. The use of pelvic fusion was identified by the CPT code 22848.
Variable frequencies were conducted at baseline. Due to the large number of ICD9 postoperative diagnosis codes, similar diagnoses were grouped for the purpose of assessing the distribution. Each ICD9 code that represented less than 2% of the cases was excluded from the distribution. In the tabulation of discharge destination, skilled care, not home (e.g., transitional care unit, subacute hospital, ventilator bed, skilled nursing home), unskilled facility, not home (e.g., nursing home or assisted facility-if not patient’s home preoperatively), and separate acute care facility (e.g., transfer to another acute care facility) were grouped together.
For all cases, patients were categorized as having a wound complication if they were specified to have either a surgical site infection or surgical incision wound disruption. Surgical site infection was defined in accordance with the Centers for Disease Control and Prevention’s National Healthcare Safety Network criteria (CDC/NHSN) (25), and thus the following variables were classified as a wound complication: superficial surgical site infection, deep surgical site infection, organ space infection, or occurrence of wound dehiscence. As described by the CDC/NHSN, organ space surgical site infection includes infection of the bone, disc space, spine, meninges, joint or bursa, intracranial, ear, eye, oral cavity, myocardium, pericardium, breast, sinus, upper respiratory tract, arteries or veins, gastrointestinal tract, intraabdominal, lung, urinary tract, reproductive tract, endometrium and vagina (25). Patients with pre-existing wound infections were not excluded from the study, as this study aims to capture the preoperative and perioperative variables that have an independent effect on wound complications.
Univariate analyses of nominal variables were conducted using the Pearson χ2 test, or the Fisher exact test when the observed cell count was lower than the expected cell count. The normality of continuous variables was evaluated using the Shapiro-Wilk Test. None of the continuous variables examined (age, operation time, length of stay) were found to have a normal distribution, thus the Kruskal-Wallis test was conducted.
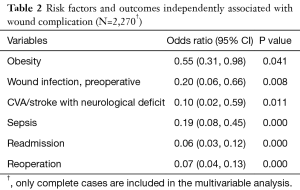
Binomial logistic regression was subsequently conducted using all the variables found to be statistically significant (P<0.05) in the univariate analysis, listed in Table 1. For the regression analysis, cases were excluded if any data points were missing from the variables in question. Of our 2,548 cases, 2,270 remained in the binomial regression. Only the variables found to be statistically significant were reported in Table 2. All statistical analyses were performed using the commercially available software, SPSS Statistics v24.0.0.0 (IBM, Armonk, NY, USA). The level of significance was set at P<0.05.

Full table
Full table
Results
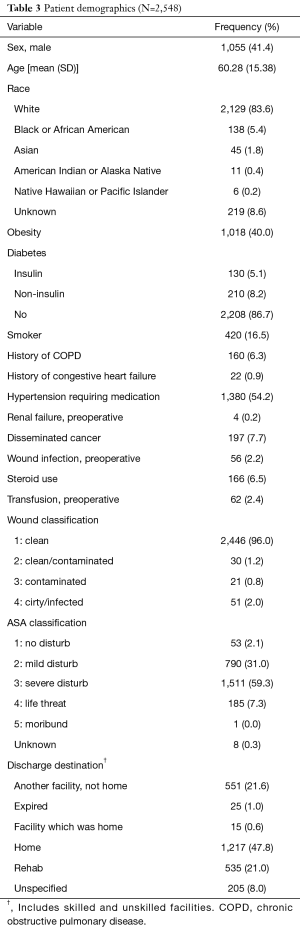
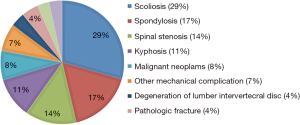
A total of 2,548 cases were identified as having a multilevel (7+ levels) instrumented thoracolumbar fusion from 2005 to 2014. The mean patient age was 60.28 years and 41.4% of the population was male (Table 3). 91.4% of patients with a reported race were classified as white. The mean time spent in the operating room was 5.86 hours (SD 2.54, 95% CI: 5.76–5.96). The average spent from operation until discharge was 7.39 days (SD 6.40, 95% CI: 7.15–7.64). The largest portion of patients undergoing multilevel fusion had a diagnosis of scoliosis (29%), followed by spondylosis (17%) and spinal stenosis (14%) (Figure 1).
Full table
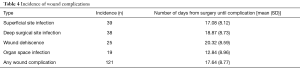
Overall, there were 121 wound complications in 108 patients, thus 4.24% of patients experienced at least one wound complication. Superficial surgical site infection and deep surgical site infection were more common complications than wound dehiscence and organ space infection (Table 4). Organ space infections presented the earliest after operation, while wound dehiscence presented the latest (Table 4).
Full table
In the univariate analysis, the following preoperative variables were found to be statistically significant (P<0.05): obesity status, BMI, preoperative wound infection, preoperative transfusion, and operation time (Table 1). The mean operation time in patients with a wound complication was 44 minutes longer (393.77±158.33 vs. 349.82±151.69 minutes, P=0.004) than those without a wound complication, possibly indicating that these are more complex procedures. The demographics of sex, age, and race were not significantly associated with wound complication (Table 1).
In the univariate analysis, the following perioperative and postoperative outcomes were found to be statistically significant (P<0.05): cerebrovascular accident (CVA)/stroke with neurological deficit, postoperative blood transfusion, deep vein thrombosis (DVT), sepsis, septic shock, readmission, reoperation, and length of hospital stay (Table 1). The mean increase in hospital length of stay in patients with a wound complication was 2.21 days (9.51±8.86 vs. 7.3±6.26 days, P=0.001). A total of 36 deaths within 30 days occurred in the group without wound complications and no deaths within 30 days occurred in the group with wound complications, but this finding was not statistically significant (Table 1). Amongst those who died, the average number of days until death was 15.31 (SD 10.02).
For the binomial logistic regression, cases were excluded if they were missing data points of variables included, leading to the exclusion of 278 cases, 20 of which had wound complications. In the binomial logistic regression analyses, obesity, preoperative infection, CVA/stroke with neurological deficit, postoperative sepsis, readmission, and reoperation were independently associated with wound complication (Table 2).
Discussion
Rate of wound complications
The overall rate of wound complications in patients undergoing long segment instrumented thoracolumbar fusion was 4.24%. Although no previous studies have been performed solely on this type of procedure, our rate is consistent with the literature on rates of wound complications following spinal surgery in general (0.7–4.4%) (4,5,10,12-14,17). Our rate is near the lower end of the range of infection rates in spinal fusions (2.6–10.1%), but these studies are not necessarily long segment and may not involve instrumentation (3,6,7,11,15,16,19,26,27). Of note, three of the aforementioned studies reported infection rates higher than the majority (3,15,27). Both Mirovsky et al., who reported a rate of 7.2%, and Pappou et al., who reported a rate of 10.1%, studied interbody fusions compared to instrumented fusion, which may account for the higher infection rates due to possible longer operative times and exposure (3,15). The third study was performed by Rechtine et al., and their rate of 10% in instrumented fusions may be accounted for by their sample size of 235 patients in a single medical center (27). Furthermore, most studies do not specify the length of spinal fusion performed.
Clinically, surgical site infections present as back pain and wound drainage (1,5,26). Our mean time to wound complication was 17.64 days, which is consistent with previous studies that report a range from 16 to 27.6 days (6,15,26).
Patient related risk factors
Obesity and preoperative transfusions were found to be significant in our study, which is consistent with previous studies (1,11,14,15). Unlike the literature, we did not find age, diabetes, cardiovascular disease, chronic obstructive pulmonary disease, smoking, steroids, malignancy, or ASA class to be risk factors for wound complication (1,4,5,11-15). Of note, some risk factors are not consistent amongst the literature. Older age has been associated with an increased risk of infection in some studies (4,15), while at least one study found that older age decreased risk of infection (17). Our study found no correlation between age and infection.
Surgery-related risk factors
The significant surgery-related risk factors in our study include operative time and length of hospital stay, which is consistent with the literature. The mean operative time of our cases was 5.86 hours, which is within the range reported in the literature (5.7–10.85 hours) (26,28). Unlike Martin et al.’s study of wound infections in a pediatric population, we found that extension to the pelvis was not a risk factor in our sample (19). In 1997, Levi et al. found a more drastic increase in length of hospital stay of 16.6 days for patients with wound complication (6). Our data demonstrates a less drastic, yet still significant, increase in length of hospital stay by 2.21 days (9.51 vs. 7.3 days, P=0.001). In 2009, Veeravagu et al. performed a study utilizing the Veterans Affairs’ NSQIP database for the years 1997–2006, and demonstrated a similar increase of 2.92 days (7.12 vs. 4.2 days) (16). Our results from 2005–2014 demonstrate longer lengths of stay for both those with and without wound complications compared to Veeravagu et al.’s data from 1997–2006, indicating a trend of longer hospitalization over the past decade although these findings may not be directly comparable due to different study populations. This trend may suggest a more intensive approach to managing and monitoring patients with wound complications over time.
Outcome measures
In our patient population, there was an association between wound complications and CVA/stroke with neurological deficit, postoperative blood transfusion, DVT, postoperative sepsis, postoperative septic shock (including organ failure), readmission, and reoperation. In accordance with our results, it has previously been demonstrated that CVA/stroke is independently associated with decreased wound healing, although the reason for this correlation is not understood (29). Reoperation rates were significantly associated with wound complication (68.1% vs. 4.6%, P=0). Veeravagu’s et al.’s study also found higher rates of reoperation in those with infection (37% vs. 2.5%). The higher rates of reoperation in our patient sample may suggest greater integration of procedures in the management of infections over time (16).
Strengths and limitations
Strengths of this study include the sample size of 2,548 long segment instrumented thoracolumbar fusions over a 9-year time span. Another strength is the inclusion of a multitude of factors that may affect surgical outcomes, from patient comorbidities to intraoperative events (e.g., blood transfusion). Limitations of the study include its retrospective study design. Additionally, the NSQIP database can only capture 30 days of post-operative complications, so any complications that occurred thereafter are not included in this analysis.
Conclusions
In our sample of 2,548 long segment (7+ vertebrae) instrumented thoracolumbar fusions, 121 wound complications occurred in 108 patients, with 4.24% cases having at least one wound complication. Binomial regression revealed obesity and preoperative wound infection as independent risk factors. Independently associated complications include CVA/stroke with neurological deficit, sepsis, readmission, and reoperation. An understanding of risk factors and outcomes specific to long segment fusions will aid surgeons in determining a patient’s risk of developing a wound complication. Furthermore, identification of independent risk factors will assist in prevention in an effort to lessen the morbidity and economic burden of wound complications in spinal surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was completed with NSQIP and was IRB exempt.
References
- Chahoud J, Kanafani Z, Kanj SS. Surgical site infections following spine surgery: eliminating the controversies in the diagnosis. Front Med (Lausanne) 2014;1:7. [Crossref] [PubMed]
- Collins I, Wilson-MacDonald J, Chami G, et al. The diagnosis and management of infection following instrumented spinal fusion. Eur Spine J 2008;17:445-50. [Crossref] [PubMed]
- Mirovsky Y, Floman Y, Smorgick Y, et al. Management of deep wound infection after posterior lumbar interbody fusion with cages. J Spinal Disord Tech 2007;20:127-31. [Crossref] [PubMed]
- Fang A, Hu SS, Endres N, et al. Risk factors for infection after spinal surgery. Spine (Phila Pa 1976) 2005;30:1460-5. [Crossref] [PubMed]
- Weinstein MA, McCabe JP, Cammisa FP. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord 2000;13:422-6. [Crossref] [PubMed]
- Levi AD, Dickman CA, Sonntag VK. Management of postoperative infections after spinal instrumentation. J Neurosurg 1997;86:975-80. [Crossref] [PubMed]
- Picada R, Winter RB, Lonstein JE, et al. Postoperative deep wound infection in adults after posterior lumbosacral spine fusion with instrumentation: incidence and management. J Spinal Disord 2000;13:42-5. [Crossref] [PubMed]
- Whitmore RG, Stephen J, Stein SC, et al. Patient comorbidities and complications after spinal surgery: a societal-based cost analysis. Spine (Phila Pa 1976) 2012;37:1065-71. [Crossref] [PubMed]
- Manoso MW, Cizik AM, Bransford RJ, et al. Medicaid status is associated with higher surgical site infection rates after spine surgery. Spine (Phila Pa 1976) 2014;39:1707-13. [Crossref] [PubMed]
- Kanayama M, Hashimoto T, Shigenobu K, et al. Effective prevention of surgical site infection using a Centers for Disease Control and Prevention guideline-based antimicrobial prophylaxis in lumbar spine surgery. J Neurosurg Spine 2007;6:327-9. [Crossref] [PubMed]
- Koutsoumbelis S, Hughes AP, Girardi FP, et al. Risk factors for postoperative infection following posterior lumbar instrumented arthrodesis. J Bone Joint Surg Am 2011;93:1627-33. [Crossref] [PubMed]
- Kanafani ZA, Dakdouki GK, El-Dbouni O, et al. Surgical site infections following spinal surgery at a tertiary care center in Lebanon: incidence, microbiology, and risk factors. Scand J Infect Dis 2006;38:589-92. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Sansur CA, et al. Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 2011;36:556-63. [Crossref] [PubMed]
- Pull ter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976) 2009;34:1422-8. [Crossref] [PubMed]
- Pappou IP, Papadopoulos EC, Sama AA, et al. Postoperative infections in interbody fusion for degenerative spinal disease. Clin Orthop Relat Res 2006.120-8. [Crossref] [PubMed]
- Veeravagu A, Patil CG, Lad SP, et al. Risk factors for postoperative spinal wound infections after spinal decompression and fusion surgeries. Spine (Phila Pa 1976) 2009;34:1869-72. [Crossref] [PubMed]
- Valentini LG, Casali C, Chatenoud L, et al. Surgical site infections after elective neurosurgery: a survey of 1747 patients. Neurosurgery 2008;62:88-95; discussion-6.
- Blam OG, Vaccaro AR, Vanichkachorn JS, et al. Risk factors for surgical site infection in the patient with spinal injury. Spine (Phila Pa 1976) 2003;28:1475-80. [Crossref] [PubMed]
- Martin CT, Pugely AJ, Gao Y, et al. Incidence and risk factors for early wound complications after spinal arthrodesis in children: analysis of 30-day follow-up data from the ACS-NSQIP. Spine (Phila Pa 1976) 2014;39:1463-70. [Crossref] [PubMed]
- Faloon MJ, Essig D, Cho W, et al. Unplanned Reoperations Affect Long-Term Outcomes in Adult Spinal Deformity Patients Undergoing Long Fusions to the Sacrum. Spine Deform 2015;3:367-71. [Crossref] [PubMed]
- Cho KJ, Suk SI, Park SR, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2007;32:2232-7. [Crossref] [PubMed]
- Nishimura Y, Hara M, Nakajima Y, et al. Outcomes and complications following posterior long lumbar fusions exceeding three levels. Neurol Med Chir (Tokyo) 2014;54:707-15. [Crossref] [PubMed]
- Mesfin A, El Dafrawy MH, Jain A, et al. Surgical outcomes of long spinal fusions for scoliosis in adult patients with rheumatoid arthritis. J Neurosurg Spine 2015;22:367-73. [Crossref] [PubMed]
- User Guide for the 2014 ACS NSQIP Participant Use Data File. American College of Surgeons 2015. Available online: https://www.facs.org/~/media/files/quality%20programs/nsqip/nsqip_puf_userguide_2014.ashx
- Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008;36:309-32. [Crossref] [PubMed]
- Glassman SD, Dimar JR, Puno RM, et al. Salvage of instrumental lumbar fusions complicated by surgical wound infection. Spine (Phila Pa 1976) 1996;21:2163-9. [Crossref] [PubMed]
- Rechtine GR, Bono PL, Cahill D, et al. Postoperative wound infection after instrumentation of thoracic and lumbar fractures. J Orthop Trauma 2001;15:566-9. [Crossref] [PubMed]
- Anastasian ZH, Gaudet JG, Levitt LC, et al. Factors that correlate with the decision to delay extubation after multilevel prone spine surgery. J Neurosurg Anesthesiol 2014;26:167-71. [Crossref] [PubMed]
- Khalil H, Cullen M, Chambers H, et al. Elements affecting wound healing time: An evidence based analysis. Wound Repair Regen 2015;23:550-6. [Crossref] [PubMed]


