
Roles of respirologists in lung transplantation in Japan: narrative review
Introduction
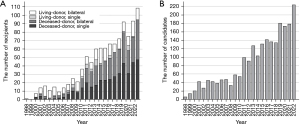
Lung transplantation (LTx) has evolved in a dramatic manner over the last decades and is currently recognized as a life-saving procedure for advanced pulmonary disease (1,2). Despite worldwide transplant success, Japan lagged behind other countries in accepting the social consensus of brain death. Although the 1997 Japanese Organ Transplantation Act legalized the transplantation of lungs from brain-dead donors, few organ donations took place at that time (Figure 1A). The Act required documented consent from donors and did not allow organ donation from children under the age of 15. Thus, the number of deceased-donor LTx surgeries was very small in the first decade, during which time the dominant procedure was living-donor LTx (3,4). However, the number of brain-dead donors increased after the revised Act became law in 2010, which allows organ donation from brain-dead individuals, regardless of their age, with family consent unless the patients refused organ donation during their lifetime (5). Consequently, the frequencies of living- and deceased-donor LTx were completely reversed. Thereafter, the number of deceased-donor LTx cases climbed to between 60 and 80 every year, up to the present day. As of the end of 2022, 1,036 LTx procedures, including 752 deceased-donor and 284 living-donor cases, have been carried out in Japan. Meanwhile, the number of LTx candidates listed with Japan Organ Transplant Network has been increasing, steadily outnumbering that of transplant recipients over time (6) (Figure 1B). At the end of 2022, there were 545 candidates on the waitlist of the Japan Organ Transplant Network.
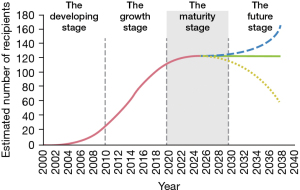
Because of the rarity of LTx and the need for appropriate experience in the developing stage [2000–2009], most of transplant process from candidacy evaluation to peri- and post-operative management including immunosuppressive and anti-microbial therapy, medical consultants (7,8) and bronchoscopic procedures (9) was handled by thoracic surgeons alone (Figure 2). A medical consultation system for maintaining a donor’s lungs in a condition suitable for transplantation is managed by thoracic surgeons from LTx centers. The system is described in the topic “Donor management and extremely high donor-utility ratio in Japan”. This deprived pulmonologists (hereinafter referred to as “respirologists”, this term being more commonly used in Japan) of opportunities to be involved in transplant practice and gave rise to the misunderstanding that transplant recipients were managed by thoracic surgeons in the growth stage [2010–2019]. However, the increasing number of both transplant candidates and recipients after implementation of the revised Act imposed a heavy burden on thoracic surgeons, who could not afford to evaluate patients with advanced pulmonary disease and provide full care of LTx recipients with complex problems. Accordingly, the development of new immunosuppression and biologics and a variety of anti-microbial agents with or without off-label use were adopted by the surgeons. In the maturity stage (2020 to the present), there are growing demands for cooperation with respirologists in LTx to accomplish transplant success in Japan. Yet, the prevailing view that transplant recipients should be managed by thoracic surgeons remains an obstacle for respirologists to actively participate in transplant practice at this stage. In addition, a long-term lack of training in LTx expertise still prevents physicians from taking on the care of LTx recipients. Nowadays, joint efforts and training of outstanding personnel who can take care of recipients are required, as this is crucial for the success of transplantation in Japan at the present stage. We present this article in accordance with the Narrative Review reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1716/rc).
Methods
Authors summarized current transplant circumstance in Japan from the transplant physician’s standpoint. A systematic search through PubMed database and Google Scholar was performed by terms of “respirologists”, “pulmonologist”, “lung transplant” or “Japan” from January 2000 and December 2022 (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | March 7, 2023 |
| Databases and other sources searched | PubMed and Google Scholar |
| Search terms used | Respirologists, pulmonologist, lung transplant or Japan |
| Timeframe | January 2000 to March 2023 |
| Inclusion and exclusion criteria | Inclusion criteria: English language |
| Exclusion criteria: Non-English language | |
| Selection process | TH conducted data selection independently and designed the study concept |
| YO is responsible for data analysis and interpretation |
Ten thoracic surgeons, a practitioner in each transplant center, were asked to complete a questionnaire on physicians’ intervention in non-surgical management of LTx in the pre-, peri- and post-transplant periods at two different time points in 2016 and 2022.
Results
Thoracic surgeons working at lung transplant centers in Japan
There are currently 10 LTx centers in Japan, these being hospitals affiliated with the following universities: Tohoku, Dokkyo-Medical, Tokyo, Chiba, Fujita-Health, Kyoto, Osaka, Okayama, Fukuoka and Nagasaki (Figure 3) (10). As of 2022, there are 1,538 board-certified general thoracic surgeons in Japan, approximately eight staff surgeons being involved in LTx at each center and roughly 80 thoracic surgeons being engaged in transplantation. As of the end of 2022, Kyoto University was the leading center for deceased-donor LTx in Japan (total number 196), followed by Tohoku (n=144) and Okayama (n=120), while living-donor transplantation was mostly carried out in Kyoto (total number 119), followed by Okayama (n=95) and Tokyo (n=26). Thoracic surgeons working at each transplant center were asked to complete a questionnaire on physicians’ intervention to LTx (Table 2). The pre-transplant process, including the review of initial referral and informed consent for candidates and assessment of living-donor eligibility, was mostly done by thoracic surgeons in 2016, some of these tasks being transferred to respirologists in 2022. Furthermore, the responsibility for post-transplant intervention, including the management of underlying disorders and native lung complications or long-term follow-up of LTx recipients, has transitioned from thoracic surgeons to respirologists over the past few years. However, a similar transition of non-surgical management in the perioperative period currently seems difficult.

Table 2
| Non-surgical management in lung transplant | 2016 | 2022 |
|---|---|---|
| Pre-transplant | ||
| Review of initial referral and informed consent for candidates | 88.9% (8/9) | 70.0% (7/10) |
| Candidacy evaluation for LTx recipient | 55.6% (5/9) | 50.0% (5/10) |
| Assessment of living-donor eligibility | 88.9% (8/9) | 80.0% (8/10) |
| Follow-up while on the waiting list | 44.4% (4/9) | 40.0% (4/10) |
| Perioperative | ||
| Evaluation of deceased donor’s lung | 100% (9/9) | 100% (10/10) |
| Systemic management in intensive-care unit (e.g., ventilator, chest drains) | 100% (9/9) | 90.0% (9/10) |
| Histocompatibility test (e.g., crossmatch, donor-specific antibodies) | 100% (9/9) | 90.0% (9/10) |
| Immunosuppressive and antimicrobial therapies | 100% (9/9) | 80.0% (8/10) |
| Post-transplant | ||
| Transplant related complication (e.g., graft infection or acute rejection) | 100% (9/9) | 70.0% (7/10) |
| Management of underlying disorder or native lung complication | 55.6% (5/9) | 30.0% (3/10) |
| Long-term follow-up of recipients (e.g., diabetes, chronic kidney disease) | 55.6% (5/9) | 40.0% (4/10) |
| Annual assessment of LTx recipients | 100% (9/9) | 80.0% (8/10) |
The trend of physicians’ intervention in non-surgical management of LTx in the pre-, intraoperative-, peri-operative, and post-transplant periods in 2016 and 2022. The actual work mainly done by thoracic surgeons or respirologists was ascertained through the questionnaire. LTx, lung transplantation.
Similar trends are also seen in other types of organ transplantation, such as kidney, liver and heart, where transplant surgeons play pivotal roles in the perioperative management of recipients (11-14). However, cooperation with physicians in other types of organ transplantation is better organized than it is in LTx in Japan. For instance, in heart transplantation, cardiologists take on the main care of recipients following surgery, while in kidney transplantation, both nephrologists and urologists support each other to successfully take care of recipients. Also, while not all hepatologists accept the role of being main care providers after liver transplantation, more physicians are involved in such transplantation than in LTx. In this respect, the leadership role of respirologists following LTx still lags behind that in other type of organ transplantation in Japan.
Roles of respirologists in LTx in Japan
The majority of Japanese respirologists and thoracic surgeons understand the need for training that will enable respirologists to manage patients before and after LTx. However, because of the severe donor shortage in Japan, the country still has a way to go to reach the global standard where LTx is a regular clinical practice for patients with advanced respiratory disease (15). Moreover, most respirologists still have few opportunities to see transplant recipients and little confidence in taking responsibility for making decisions concerning the management of immunosuppression and allograft dysfunction of LTx recipients. Therefore, it will take time for Japanese physicians to become involved in the whole LTx process. Perhaps it is still too early to argue that transplant physicians, in view of their highly professional expertise in the field of LTx, are valuable in their being able to provide a broad range of services to the recipients and transplant team value.
Given such unique circumstances surrounding transplantation in Japan, there is no need for all respirologists to have a detailed knowledge of transplant practice. The role of individual respirologists in either a part of or the whole of the LTx process would be stratified on the basis of the size and function of the facility at which they work (Table 3). Respirologists at a non-transplant center do not necessarily concentrate on interpreting histocompatibility tests or on post-operative management of recipients in an intensive-care unit. Instead, their value lies in their understanding of the optimal timing for referral and patient selection for LTx listing as well as their basic knowledge of the long-term management of LTx recipients (16). In contrast, respirologists working at a transplant center have several options: some devote themselves to the management of LTx recipients between pre- and post- transplant periods as a second sub-specialty in pulmonary medicine; others, depending on their sub-specialties, provide consultation for appropriate anti-microbial therapy such as pre-emptive therapy or universal prophylaxis and management of underlying disease or transplant-related complications. Meanwhile, at high- or intermediate-volume transplant centers, transplant physicians are encouraged to participate as members of the transplant teams. However, since the value and importance of transplant physicians have gone unrecognized by society, institutional understanding and assurance of sustainable employment in the field are needed.
Table 3
| Respirologists working at a non-transplant center |
| Optimal timing for referral and patient selection for LTx listing and basic understanding of long-term management of LTx recipients |
| Respirologists working at a lung transplant center |
| In addition to basic understanding of transplant practice working at a non-transplant center, knowledge of candidacy evaluation and post-operative management |
| Transplant physician at a high-volume lung transplant center |
| Management of patients between pre- and post-transplant periods, with responsibilities that include candidacy evaluation, ensuring that patients remain qualified while on the waiting list, intervention of histocompatibility, and short- and long-term management of immunosuppressive therapy and allograft dysfunction |
LTx, lung transplantation.
The following, which relates to Tohoku University Hospital, illustrates how lung transplant physicians play a decisive role in the management of LTx candidates and recipients. Patients with advanced pulmonary disease are referred to Tohoku University Hospital for an extensive evaluation concerning transplant candidacy. The transplant physician explains the risks (such as complications of the transplant surgery, life-long immunosuppression and increased risk of infection) and benefits (greater quality of life, improved functionality and longer survival) of LTx, and informed consent is obtained from the candidates. Close communication between primary care respirologists at a non-transplant center and the transplant physician is essential to transplant success given the long waiting time of over 900 days with an approximately 50% waitlist mortality in Japan (5,15). As most candidates deteriorate in the interim, the transplant physician shares the candidates’ conditions or newly-developed complications with the respirologists and considers using marginal donor lungs or changing the transplant procedure from single to bilateral LTx. Post-transplant management at a non-transplant center requires the support of the transplant physician with respect to transplant-associated complications, such as graft rejection or cytomegalovirus infection, or optimization of immunosuppressive therapy based on the adverse events or graft function (17-20).
Current activities to address the future direction of LTx in Japan
Japan has taken steps toward increasing the number of donors and recipients and is at the stage of maturity, where, for progress to continue, a number of significant changes are needed (Figure 2). There is a clear need for respirologists to become involved either in transplant or non-transplant centers in order to expand the transplant service and provide higher-quality care to patients with advanced pulmonary disease as well as to LTx recipients. At the current stage, educating respirologists who can take care of patients before and after LTx and display their leadership in the transplant practice is an immediate top priority in Japan. Additionally, development of transplant physicians and establishment of their positions at transplant centers is an overriding issue. A significant growth in LTx in Japan cannot be expected in the future unless these issues are addressed. Increasing the number of respirologists taking care of LTx recipients is certain to change the circumstances with respect to transplantation in Japan. The more trained respirologists participate in transplantation, the more widely transplantation will be provided to patients, resulting in the growth of candidates and recipients. This change will help transplant practice become widely accepted by the Japanese public and, consequently, will lead to the public acceptance of brain death as well as an increase in the number of donors. In view of the increasing number of organ donations and transplants in Japan, the management of LTx recipients will get out of control if only thoracic surgeons are involved. Additionally, given respirologists’ high degree of expertise in immunosuppressive therapy, based on the recipients’ graft function, and their ability to provide long-term care of recipients with complicated backgrounds and comorbidities, involvement of respirologists at all centers, as well as authorized transplant physicians at transplant centers, is essential for Japanese transplant sustainability (21). In order to do that, some high-volume transplant centers have started respirologist training programs that accept visiting physicians from non-transplant centers or low-volume centers in order to give them experience in seeing candidates on the waiting list and LTx recipients. In other LTx centers, the two sides meet halfway: respirologists and thoracic surgeons collaboratively register patients with advanced pulmonary disease with the Japan Organ Transplant Network and also follow LTx recipients in respiratory clinics. Alternatively, some LTx centers routinely hold online LTx workshops for respirologists, where optimal timing for a referral or basic management of LTx recipients is shared with transplant physicians. The management of transplant recipients will, in future, be included in a respiratory fellowship program. It is hoped those issues will be brought up for discussion at meetings of The Japanese Society of Internal Medicine (22) or The Japanese Respiratory Society (23).
Conclusions
In view of the LTx situation in Japan and the roles played by thoracic surgeons to date, there is an urgent need for respirologists to become involved in LTx practice. Although LTx centers are currently devoted to educating respirologists to take care of patients before and after LTx, it will take time for these physicians to become involved in the whole process of transplantation and display their leadership in transplant practice. A significant growth in LTx in Japan cannot be expected until such involvement is achieved.
Acknowledgments
Funding: This work was supported in part by,
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Masaaki Sato) for the series “Why is the Outcome Good? Secrets of Lung Transplantation in Japan” published in Journal of Thoracic Disease. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1716/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1716/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1716/coif). The special series “Why is the Outcome Good? Secrets of Lung Transplantation in Japan” was commissioned by the editorial office without any funding or sponsorship. TH reports receiving support from Grant-in-Aid for Scientific Research C from the Japan Society for the Promotion of Science (No. 23K08287), Takeda Science Foundation (The visionary research 2021), Tokyo-Hokenkai Byotai-Seiri Laboratory (Clinical Research Grant 2022) and the Cooperative Research Project Program of Joint Usage/Research Center at the Institute of Development, Aging and Cancer, Tohoku University (2022-11). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Perch M, Hayes D Jr, Cherikh WS, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-ninth adult lung transplantation report-2022; focus on lung transplant recipients with chronic obstructive pulmonary disease. J Heart Lung Transplant 2022;41:1335-47. [Crossref] [PubMed]
- Chambers DC, Perch M, Zuckermann A, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-eighth adult lung transplantation report - 2021; Focus on recipient characteristics. J Heart Lung Transplant 2021;40:1060-72. [Crossref] [PubMed]
- Nakajima D, Date H. Living-donor lobar lung transplantation. J Thorac Dis 2021;13:6594-601. [Crossref] [PubMed]
- Date H. Living-related lung transplantation. J Thorac Dis 2017;9:3362-71. [Crossref] [PubMed]
- Hirama T, Akiba M, Watanabe T, et al. Waitlist Mortality in Lung Transplant Candidates in Japan. Transplantation 2022;106:1507-9. [Crossref] [PubMed]
- Japan Organ Transplant Network. Available online: https://www.jotnw.or.jp/en/, accessed on March 1, 2023
- Fukushima N, Ono M, Saiki Y, et al. Donor evaluation and management system (medical consultant system) in Japan: experience from 200 consecutive brain-dead organ donation. Transplant Proc 2013;45:1327-30. [Crossref] [PubMed]
- Konoeda C, Sato M. Current situation of lung transplantation in Japan. Curr Chall Thorac Surg 2022;4:6. [Crossref]
- Inoue M, Minami M, Wada N, et al. Results of surveillance bronchoscopy after cadaveric lung transplantation: a Japanese single-institution study. Transplant Proc 2014;46:944-7. [Crossref] [PubMed]
- The Japanese Society for Heart and Lung Transplantation. Available online: http://www2.idac.tohoku.ac.jp/dep/surg/shinpai/, accessed on March 1, 2023
- Fukui A, Yokoo T, Nangaku M, et al. New measures against chronic kidney diseases in Japan since 2018. Clin Exp Nephrol 2019;23:1263-71. [Crossref] [PubMed]
- Soyama A, Eguchi S, Egawa H. Liver transplantation in Japan. Liver Transpl 2016;22:1401-7. [Crossref] [PubMed]
- Oda N, Kato TS, Komamura K, et al. Clinical course and outcome of heart transplant recipients: single center experience at the National Cardiovascular Center in Japan. Int Heart J 2010;51:264-71. [Crossref] [PubMed]
- Kato TS, Gomi H, Aizawa Y, et al. Are we ready for building transition programs for heart transplant recipients in Japan? - Knowing the unique background is the first step for discussion. Front Pediatr 2022;10:935167. [Crossref] [PubMed]
- Hirama T, Akiba M, Watanabe T, et al. Waiting time and mortality rate on lung transplant candidates in Japan: a single-center retrospective cohort study. BMC Pulm Med 2021;21:390. [Crossref] [PubMed]
- lversen M. Immunosuppression for the non-transplant physician: what should you know? Breathe 2013;9:202-8. [Crossref]
- Kumata S, Hirama T, Watanabe Y, et al. The fraction of sensitization among lung transplant recipients in a transplant center in Japan. BMC Pulm Med 2020;20:256. [Crossref] [PubMed]
- Katahira M, Hirama T, Eba S, et al. Impact of Postoperative Continuous Renal Replacement Therapy in Lung Transplant Recipients. Transplant Direct 2020;6:e562. [Crossref] [PubMed]
- Nikkuni E, Hirama T, Hayasaka K, et al. Recovery of physical function in lung transplant recipients with sarcopenia. BMC Pulm Med 2021;21:124. [Crossref] [PubMed]
- Hirama T, Tomiyama F, Notsuda H, et al. Outcome and prognostic factors after lung transplantation for bronchiectasis other than cystic fibrosis. BMC Pulm Med 2021;21:261. [Crossref] [PubMed]
- Nelson J, Alvey N, Bowman L, et al. Consensus recommendations for use of maintenance immunosuppression in solid organ transplantation: Endorsed by the American College of Clinical Pharmacy, American Society of Transplantation, and the International Society for Heart and Lung Transplantation. Pharmacotherapy 2022;42:599-633. [Crossref] [PubMed]
- The Japanese Society of Internal Medicine. Available online: https://www.naika.or.jp/english/, accessed on March 1, 2023.
- The Japanese Respiratory Society. Available online: https://www.jrs.or.jp/english/, accessed on March 1, 2023.


