Abstract
Synopsis
The microemulsion-basedformulation of cyclosporin (Neoral®; referred to as the microemulsion formulation in this review) is a microemulsion preconcentrate which has been developed to overcome problems associated with the poor and unpredictable absorption of the standard oral formulation of this drug. These include marked intra- and interpatient variability in the extent of absorption, a poor correlation between trough blood concentrations of cyclosporin and total systemic exposure, and the need for regular monitoring of blood cyclosporin concentrations.
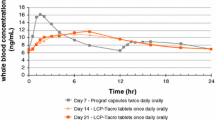
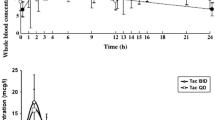
In healthy volunteers and renal or liver transplant recipients, administration of the microemulsion formulation resulted in cyclosporin absorption which was significantly faster, more extensive and more predictable than that seen with the standard oral formulation. Furthermore, measurement of whole-blood trough cyclosporin concentrations provided a better estimate of systemic drug exposure in renal transplant recipients who received the microemulsion formulation than in those who received the standard formulation. Systemic exposure of cyclosporin delivered by the new formulation appears to be relatively unaffected by food intake.
Initial data suggest that drug absorption from the microemulsion formulation is enhanced in comparison with that achieved from the standard formulation in liver transplant recipients undergoing biliary diversion or with cholestasis, although absorption from the new formulation does not appear to be completely independent of bile. Preliminary results from other groups that experience cyclosporin malabsorption from the standard formulation (patients with cystic fibrosis or diabetes, and children) are also encouraging.
Clinical trials specifically designed to investigate the relative immunosuppressive efficacy of the microemulsion formulation have not been reported; further data are required to fully establish the relationship between the more rapid and extensive absorption of cyclosporin from the microemulsion formulation and the probability of graft rejection or adverse events (including nephrotoxicity and hypertension). However, no statistically significant differences have been noted between the 2 formulations in the incidence of these events in studies to date. The incidence of rejection in new renal or liver transplant recipients treated for a minimum of 3 months was ≈31 to 50% in those receiving the microemulsion formulation and ≈24 to 56% in those receiving the standard formulation.
Thus, although confirmation of existing efficacy and tolerability data is required, the characteristic pharmacokinetic properties of the microemulsion formulation make it an attractive option for the oral delivery of cyclosporin in transplant recipients, offering more predictable and more extensive drug absorption than the standard formulation. The microemulsion formulation may be of particular benefit in patients who show poor absorption of cyclosporin from the standard oral formulation, such as liver transplant recipients with biliary diversion or cholestasis.
Overview of Pharmacodynamic Properties
Cyclosporin is an inhibitor of T cell activation and causes suppression of the cell-mediated immune response. In complex with its receptor protein (cyclophilin), cyclosporin is believed to inhibit calcineurin-mediated regulation of cytokine transcription. Thus, cyclosporin may prevent the expression of interleukin-2 and other cytokines by T helper cells, a process which is central to the immune response involved in graft rejection.
Pharmacokinetic Properties
The standard oral formulation of cyclosporin (oil-based solution or soft gelatin capsules) is characterised by poor and unpredictable drug absorption. In an attempt to overcome these limitations, a new formulation of cyclosporin (Neoral®; referred to as the microemulsion formulation in this review) has been developed. This new formulation is a microemulsion preconcentrate which, on contact with gastrointestinal fluids, readily produces a microemulsion that mimics the mixed micellar phase of absorption seen with the standard oral formulation. The microemulsion system is stable, releases cyclosporin quickly, and can be diluted without causing precipitation.
In comparison with the standard formulation, delivery of cyclosporin by the microemulsion formulation results in more extensive and faster drug absorption [increased area under the whole-blood concentration versus time curve (AUC), increased maximum concentration (Cmax) and shorter time to Cmax], a more predictable relationship between trough cyclosporin concentration and systemic exposure, and reduced intra- and interindividual variability for a range of pharmacokinetic parameters. In addition, the overall systemic exposure of cyclosporin as measured by AUC does not appear to be significantly affected by food intake in patients receiving the microemulsion formulation; previous clinical experience indicates that the effects of food intake on cyclosporin absorption from the standard formulation are unpredictable.
In small numbers of liver transplant recipients with biliary diversion via an open T tube, the systemic exposure of cyclosporin from the microemulsion formulation was significantly greater than that seen with the standard formulation. However, limited data also suggest that cyclosporin absorption from the microemulsion formulation is not completely independent of bile flow.
Improvements in the rate and extent of cyclosporin absorption have also been seen with the microemulsion formulation compared with the standard formulation in other transplant groups (heart transplant recipients, patients with diabetes who have undergone kidney or simultaneous kidney and pancreas transplantation, and patients with cystic fibrosis who are candidates for heart-lung transplantation) and in patients with rheumatoid arthritis or other autoimmune disease.
Clinical Efficacy and Pharmacoeconomic Considerations
Statistically significant differences in the incidence of rejection episodes have not been observed between patients receiving the microemulsion or standard formulations in studies available to date. However, most of the relevant data come from pharmacokinetic and tolerability studies which were of short duration and/or involved relatively small numbers of patients; large, well-controlled clinical trials specifically designed to investigate immunosuppressive efficacy are still needed. The incidence of rejection in new renal or liver transplant recipients treated for a minimum of 3 months was ≈31 to 50% in those receiving the microemulsion formulation and ≈24 to 56% in those receiving the standard formulation.
Retrospective pharmacoeconomic analyses of clinical studies involving new or stable renal transplant recipients suggest that direct healthcare costs are up to 28% lower in patients receiving the microemulsion formulation than in those receiving the standard formulation over a 12-week period, although statistical analysis of these differences was not provided. Cyclosporin acquisition costs were not included in these analyses; however, the cost of the microemulsion formulation is the same as that of the standard formulation.
Tolerability
Information on the tolerability of the microemulsion formulation in transplant recipients has been derived primarily from studies which were of short duration and/or involved small numbers of patients. The microemulsion and standard formulations of cyclosporin appeared to be similar in terms of the type, incidence and severity of adverse events which were observed in these investigations. Renal function was stable in the majority of patients treated with the microemulsion formulation; where clinically significant nephrotoxicity (as measured by increased serum creatinine levels) was reported, the incidence was not significantly different from that seen in recipients of the standard formulation. Effects on blood pressure have been similar in the few comparative clinical trials of the microemulsion and standard formulations.
The most common adverse events in 33 new renal transplant recipients who received the microemulsion formulation (mean dosage 3.4 mg/kg/day) for 12 months were hypertrichosis (58%), gingival hyperplasia (52%) and tremor (30%). Headache, oedema, tremor, gingival hyperplasia and nausea/vomiting/epigastric pain were the most common adverse events (incidence less than 10% for each event) recorded in 373 stable renal transplant recipients who received the microemulsion formulation for 12 weeks after switching from the standard formulation.
Dosage and Administration
A 1 : 1 dose conversion from the standard formulation of cyclosporin to the microemulsion formulation has been used successfully in pharmacokinetic and clinical studies involving stable renal transplant recipients. However, definitive conversion guidelines have yet to be published and a 1 : 1 conversion may not be appropriate for other types of transplant recipients, particularly those with cyclosporin malabsorption. A 1 : 1 conversion to the microemulsion formulation in stable renal transplant recipients resulted in either similar trough cyclosporin concentrations or the need for downward dose adjustment of up to 20% to maintain clinically appropriate concentrations of cyclosporin. The mean oral dosage of the microemulsion formulation ranged from 3.4 to 15 mg/kg/day in clinical trials in renal or liver transplant recipients.
Similar content being viewed by others
References
Faulds D, Goa KL, Benfield P. Cyclosporin: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in immunoregulatory disorders. Drugs 1993 Jun; 45: 953–1040.
Shaefer MS, Collier DS. Immunosuppression for solid organ transplantation. Dialysis Transplant 1993 Sep; 22: 542–71.
Graham RM. Cyclosporine: mechanisms of action and toxicity. Cleve Clin J Med 1994 Jul–Aug; 61: 308–13.
Fahr A. Cyclosporin clinical pharmacokinetics. Clin Pharmacokinet 1993 Jun; 24: 472–95.
Vonderscher J, Meinzer A. Rationale for the development of Sandimmune Neoral. Transplant Proc 1994 Oct; 26: 2925–7.
Kahan BD. Individualization of cyclopsorine therapy using pharmacokinetic and pharmacodynamic parameters? Transplantation 1985; 40 (5): 457–76.
Kahan BD, Grevel J. Optimization of cyclosporine therapy in renal transplantation by a pharmacokinetic strategy? Transplantation 1988; 46 (5): 631–44.
Kahan BD. The impact of ciclosporin pharmacokinetics on transplant outcome: the potential benefits of Sandimmun Neoral® therapy. In: Neoral: A New Formulation of Ciclosporin. New York: World Medical Press, 1994: 12–9
Kovarik JM, Mueller EA, van Bree JB, et All Cyclosporine pharmacokinetics and variability from a microemulsion formulation — a multicenter investigation in kidney transplant patients. Transplantation 1994 Sep 27; 58: 658–63
Kahan BD, Dunn J, Fitts C, et al. Reduced inter- and intrasubject variability in cyclosporine pharmacokinetics in renal transplant recipients treated with a microemulsion formulation in conjunction with fasting, low-fat meals, or high-fat meals. Transplantation 1995 Feb 27; 59: 505–11.
Nankivell BJ, Hibbins M, Chapman JR. Diagnostic utility of whole blood cyclosporine measurements in renal tranplantation using triple therapy? Transplantation 1994; 58 (9): 989–96.
Lindholm A, Kahan BD. Influence of cyclosporine pharmacokinetics, trough concentrations, and AUC monitoring on outcome after kidney transplantation. Clin Pharmacol Ther 1993; 54: 205–18.
Levy G, Grant D. Potential for CsA-Neoral in organ tranplantation? Transplant Proc 1994; 26 (5): 2932–4.
Mueller EA, Kovarik JM, van Bree JB, et al. Influence of a fat-rich meal on the pharmacokinetics of a new oral formulation of cyclosporine in a crossover comparison with the market formulation. Pharm Res 1994 Jan; 11: 151–5.
Sketris IS, Lawen JG, Beauregard-Zollinger L, et al. Comparison of the pharmacokinetics of cyclosporine Sandimmune with Sandimmune Neoral in stable renal transplant patients. Transplant Proc 1994 Oct; 26: 2961–3.
Kovarik JM, Mueller EA, van Bree JB, et al. Within-day consistency in cyclosporine pharmacokinetics from a microemulsion formulation in renal transplant patients. Ther Drug Monit 1994 Jun; 16: 232–7.
Foradori AC, Martinez L, Vacarezza A, et al. Pharmacokinetics of a new galenical formulation of oral cyclosporine Ain stable kidney transplanted patients. Transplant Proc 1994 Oct; 26: 2969–72.
Kovarik JM, Vernillet L, Mueller EA, et al. Cyclosporine disposition and metabolite profiles in renal transplant patients receiving a microemulsion formulation. Ther Drug Monit 1994 Oct; 16: 519–25.
Freeman D, Grant D, Levy G, et al. Pharmacokinetics of a new oral formulation of cyclosporine in liver transplant recipients. Ther Drug Monit 1995; 17: 213–6.
Kovarik JM, Mueller EA, van Bree JB, et al. Reduced inter- and intraindividual variability in cyclosporine pharmacokinetics from a microemulsion formulation. J Pharm Sci 1994 Mar; 83: 444–6.
Mueller EA, Kovarik JM, van Bree JB, et al. Improved dose linearity of cyclosporine pharmacokinetics from a microemulsion formulation. Pharm Res 1994 Feb; 11: 301–4.
Weiss M, Zantvoort FA, Lison A-E, et al. Clinical study of a new cyclosporin formulation [abstract]. Nephrol Dial Transplant 1994; 2: 1053.
Foradori AC, Martinez L, Elberg A, et al. Preliminary pharmacokinetic evaluation of a new galenical formulation of oral cyclosporine A: Neoral TM. Transplant Proc 1995 Apr; 27: 1813–4.
Lin CY, Lee SE Comparison of pharmacokinetics between CsA capsules and Sandimmun Neoral in pediatric patients. Transplant Proc 1994 Oct; 26: 2973–4
Bökenkamp P, Enke B, Offner G, et al. Conversion from Sandimmun® to a new oral formulation of CsA in paediatric renal transplant recipients [abstract]. Pediatr Nephrol 1994 Oct; 8: C72.
Levy G, Altraif I, Rezieg M, et al. Cyclosporine Neoral in liver transplant recipients. Transplant Proc 1994 Dec; 26: 3184–7.
Superina RA, Strong DK, Acal LA, et al. Relative bioavailability of Sandimmune and Sandimmune Neoral in pediatric liver recipients. Transplant Proc 1994 Oct; 26: 2979–80.
Mueller EA, Kallay Z, Kovarik JM, et al. Bile-independent absorption of cyclosporine from a microemulsion formulation in liver transplant patients. Transplantation. In press
Trull AK, Tan KKC, Tan L, et al. Absorption of cyclosporin from the conventional and new microemulsion oral formulation in liver transplant recipients with extaernal biliary diversion. Br J Clin Pharmacol 1995; 39: 627–31.
Winkler M, Ringe B, Oldhafer K, et al. Influence of bile on cyclosporin absorption from microemulsion formulation in primary liver transplant recipients. Transpl Int 1995; 8: 324–6.
Levy G, Rochon J, Freeman D, et al. Cyclosporine Neoral in liver transplant recipients. Transplant Proc 1994 Oct; 26: 2949–52.
Färber L, Malbücher A, Geissler F, et al. Favourable clinical results of Sandimmun-Neoral in malabsorbing liver and heart transplant recipients? Transplant Proc 1994; 26 (5): 2988–93.
Belli LS, De Carlis L, Rondinara GF. Sandimmun-Neoral in liver transplantation: a remarkable improvement in long-term immunosuppression? Transplant Proc 1994; 26 (5): 2983–4.
Atkison PR, Grant DR, Williams SE, et al. Sandimmune Neoral in paediatric liver transplant recipients with malabsorption of cyclosporin A. Transplant Proc 1994 Oct; 26: 2953–4.
Winkler M, Ringe B, Schneider K, et al. Enhanced bioavailability of cyclosporine using a new oral formulation (Sandimmun optoral) in a liver-grafted patient with severe cholestasis. Transpl Int 1994 Mar; 7: 147–8.
Fiocchi R, Mamprin F, Gamba A, et al. Pharmacokinetic profile of cyclosporine in long-term heart transplanted patients treated with a new oral formulation. Transplant Proc 1994 Oct; 26: 2994–5.
Mikhail G, Eadon H, Leaver N, et al. Use of Neoral in heart transplant recipients. Transplant Proc 1994 Oct; 26: 2985–7.
Johnston A, Reynold L, Wright DL, et al. Pharmacokinetics of cyclosporin in heart transplant patients after administration of Sandimmun® and a new oral formulation — Neoral® [abstract no? 129]. Ther Drug Monit 1995; 17 (4): 415.
Storck M, Mickley V, Gräb C, et al. Cyclosporine levels in diabetic (type 1) patients undergoing kidney and pancreas transplantation: role of a new galenica formulation. Transplant Proc 1994 Oct; 26: 2996–8.
Tan KKC, Trull AK, Uttridge JA, et al. Relative bioavailability of cyclosporin from conventional and microemulsion formulations in heart-lung transplant candidates with cystic fibrosis. Eur J Clin Pharmacol 1995; 48: 285–89.
Van den Borne BEEM, Landewé RBM, Goei The HS, et al. Relative bioavailability of a new oral form of cyclosporin A in patients with rheumatoid arthritis. Br J Clin Pharmacol 1995 Feb; 39: 172–5.
Open, multicentre trial to evaluate the safety and steady-state pharmacokinetic profile of SANDIMMUN NEORAL in patients with rheumatoid arthritis switched from Sandimmun soft gelatin capsules. Study Report, Institute of Clinical Methodology and Medical Pathology I, University of Pisa, Pisa, Italy. Sandoz Pharma Ltd., 1995 (Data on file)
Niese D, on behalf of the International Sandimmun Neoral Study Group. A double-blind randomized study of Sandimmun Neoral versus Sandimmun in new renal transplant recipients: results after 12 months. Transplant Proc 1995 Apr; 27: 1849–56.
Frei U, Taesch S, Niese D. Use of Sandimmun Neoral in renal transplant patients. Transplant Proc 1994 Oct; 26: 2928–31 (Study in 2 parts. Pt A).
Pollak R. The Neoral™ vs Sandimmune® soft-gelatin capsule randomized multicenter three-month double-blind trial (N-103): tolerability and safety profiles. In: Neoral™: The New Microemulsion Formulation of Cyclosporine, Special Report, May 1995. Cedar Knolls, New Jersey, USA: World Medical Press, 1995: 19–27
Keown P, Lawen JG, Landsberg D, et al. Economic analysis of Sandimmune Neoral in Canada in stable renal transplant patients. Transplant Proc 1995 Apr; 27: 1845–8.
Sandoz Neoral to replace Sandimmune as anti-organ rejection gold standard, firm says; cyclosporine microemulsion cost will be same as Sandimmune. FDC Rep Pink Sheet 1995; July 24, 1995: 4–5
Sandoz’ Neoral approved in US. Scrip 1995 July 25; 2045: 17
Rossi SJ, Schroeder TJ, Hariharan S. Prevention and management of the adverse effects associated with immunosuppressive therapy. Drug Saf 1993 Aug; 9: 104–31.
Markell MS, Armenti V, Danovitch G, et al. Hyperlipidemia and glucose intolerance in the post-renal transplant patient. J Am Soc Nephrol 1994 Feb; 4 Suppl. 1: 37–47
Belli LS, Slim OA, De Carlis L, et al. Neoral in liver transplant patients: pharmacokinetic study and clinical implications. Transplant Proc 1994 Oct; 26: 2981–2.
Neumayer H-H, Färber L, Haller P, et al. Clinical experience transferring kidney transplant patients from Sandimmun to Sandimmun Neoral — results after 3 months. Clin Nephrol 1995 Jan; 43 Suppl. 1:27–32
Mueller EA, Kallay Z, Kovarik JM, et al. Assessment of glomerular filtration rate after multiple administration of a new oral formulation of cyclosporine in clinically stable renal transplant patients. Transplant Proc 1995 Feb; 27 (1): 834–6
Mueller EA, Kovarik JM, van Bree JB, et al. Pharmacokinetics and tolerability of a microemulsion formulation of cyclosporine in renal allograft recipients — a concentration-controlled comparison with the commercial formulation. Transplantation 1994 Apr 27; 57: 1178–82.
Neumayer H-H, Färber L, Haller P, et al. Conversion from Sandimmun to Sandimmun Neoral in patients with stable renal allografts: results after 1 month. Transplant Proc 1994 Oct; 26: 2944–8.
Neumayer H-H, Färber L, Haller P, et al. Conversion from Sandimmun to Sandimmun Neoral — experience in 300 patients after renal transplantation: results after one year [abstract]? Nephrol Dial Transplant 1995; 10 (6): 1058.
Whitington PF, Emond JC, Whitington SH, et al. Small-bowel length and the dose of cyclosporine in children after liver transplantation? N Engl J Med 1990; 322 (11): 733–8.
Lindholm A, Welsh M, Alton C, et al. Demographic factors influencing pharmacokinetic parameters in patients with uremia: racial differences in bioavailability. Clin Pharmacol Ther 1992; 52: 359–71.
Kahan BD, Van Buren CT, Lin SN, et al. Immunopharmalogical monitoring of cyclosporin A-treated recipients of cadaveric kidney allografts? Transplantation 1982; 34 (1): 36–45.
Kahan BD, Shaw LM, Holt DH, et al. Consensus document: Hawk’s Cay Meeting on therapeutic drug monitoring of cyclosporine? Clin Chem 1990; 36 (8): 1510–6.
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: C.G. Barnes, Department of Rheumatology, The Royal London Hospital, London, England; L.S. Belli, Divisione Epatologia Crespi, Ospedale Niguarda Ca’ Granda, Milan, Italy; H. Bismuth, Centre Hepato-Biliaire, Hôpital Paul Brousse, Villejuif, France; U. Frei, Department of Nephrology and Intensive Care Medicine, Universitätsklinikum Rudolf Virchow, Berlin, Germany; K. Fukao, Institute of Clinical Medicine, University of Tsukuba, Tsukuba, Japan; R.M. Graham, The Victor Chang Cardiac Research Institute, St Vincent’s Hospital, Sydney, New South Wales, Australia; J.H. Helderman, Vanderbilt Transplant Center, Vanderbilt University Medical Center, Nashville, Tennessee, USA; B.D. Kahan, Division of Immunology and Organ Transplantation, The University of Texas Health Science Center at Houston, Houston, Texas, USA; J. Kay, School of Biological Sciences, University of Sussex, Brighton, England; G. Levy, The Toronto Hospital, University of Toronto, Toronto, Ontario, Canada; T.E. Mandel, Department of Surgery, University of Cambridge Clinical School, Cambridge, England; G. Mikhail, Transplant Office, Harefield Hospital, Harefield, England; H.-H. Neumayer, Universitätsklinikum Charité, Medizinische Klinik und Poliklinik V, Berlin, Germany; A.K. Trull, Department of Clinical Biochemistry, Addenbrooke’s Hospital, Cambridge, England; A.G. Tzakis, Division of Transplantation, University of Miami School of Medicine, Miami, Florida, USA; J.A. Vale, West Midlands Poisons Unit, Birmingham, England; B.E.E.M. van den Borne, Department of Rheumatology, University Hospital, Leiden, The Netherlands.
Rights and permissions
About this article
Cite this article
Noble, S., Markham, A. Cyclosporin. Drugs 50, 924–941 (1995). https://doi.org/10.2165/00003495-199550050-00009
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199550050-00009