Abstract
Synopsis
Eutectic lidocaine/prilocaine cream 5% is a eutectic mixture of the local anaesthetics lidocaine (lignocaine) 25 mg/g and prilocaine 25 mg/g that provides dermal anaesthesia/analgesia following topical application.
The principal indication in which eutectic lidocaine/prilocaine cream has been studied is the management of pain associated with venipuncture or intravenous cannulation, where significantly greater pain relief than placebo, with equivalent efficacy to ethyl chloride spray and lidocaine infiltration, has been demonstrated. In dermatological surgery, eutectic lidocaine/prilocaine cream offers effective pain relief in children undergoing curettage of molluscum contagiosum lesions, and in adults undergoing split-skin graft harvesting. Particular benefit has also been shown with use of eutectic lidocaine/prilocaine cream in association with treatment of condylomata acuminata in both men and women, and it appears to provide a useful alternative to lidocaine infiltration in this context. Further research in such indications as paediatric lumbar puncture, minor otological surgery, and minor gynaecological, urological and andrological procedures is likely to further broaden the profile of clinical use for eutectic lidocaine/prilocaine cream.
Eutectic lidocaine/prilocaine cream has a very favourable tolerability profile, transient and mild skin blanching and erythema being the most frequent adverse events to occur in association with its application to skin. The potential for inducing methaemoglobinaemia, attributed to a metabolite of the prilocaine component of the formulation, prohibits its use in infants younger than 6 months.
In summary, eutectic lidocaine/prilocaine cream is a novel formulation of local anaesthetics that has proven to be effective and well-tolerated in the relief of pain associated with various minor interventions in adults and children.
Pharmacodynamic Properties
Studies in healthy volunteers have indicated that application of eutectic lidocaine/prilocaine cream for at least 60 minutes before venous cannulation affords significantly greater pain relief than placebo. The maximal depth of analgesia to needle insertion after application of eutectic lidocaine/prilocaine cream was identified as 5mm, obtained 30 minutes after application for 90 minutes, or during the 60 minutes after application for 120 minutes. Local blood flow, as well as epidermal and dermal thickness appear to be important factors affecting the efficacy of eutectic lidocaine/prilocaine cream. Efficacy, as determined by the response to argon laser stimulation, increased with increasing application time for sites including the back, cheek, cubital fossa and dorsum of the hand, while an inverse relationship held for application to the forehead. Onset of analgesia was rapid when eutectic lidocaine/prilocaine cream was applied to the back, but declined rapidly after discontinuation. In contrast, after application to the cubital fossa and the hand, onset of analgesia was slower but increased for up to 60 minutes after removal, followed by a slow decline.
In children aged approximately 2 to 13 years undergoing venipuncture, a ‘thick layer’ of eutectic lidocaine/prilocaine cream, defined as 2ml (approximately 2g) applied to an area measuring 30 by 32mm on the dorsum of the hand, was significantly more effective than a ‘thin layer’, defined as 0.5ml of the cream applied over the same area, in providing pain relief. 91% of patients in the ‘thick layer’ group experienced ‘no pain’ vs 69% in the ‘thin layer’ group.
Volunteer studies have also indicated analgesic efficacy of eutectic lidocaine/prilocaine cream greater than that of placebo in individuals undergoing subcutaneous injection or tourniquet inflation. Eutectic lidocaine/prilocaine cream also provided greater local anaesthesia of the tympanic membrane than lidocaine spray in 1 study. Findings from a study in volunteers undergoing fibreoptic airway endoscopy, however, suggested that eutectic lidocaine/prilocaine cream 1ml provided less effective topical anaesthesia of the nasal mucosa than lidocaine 4% solution, 2% gel or five 10mg doses of a spray. Eutectic lidocaine/prilocaine cream appeared to provide a similar degree of local analgesia to a 10% lidocaine spray applied to the gingival membrane in 1 volunteer study.
Preliminary findings suggest that the analgesia obtained with eutectic lidocaine/prilocaine cream may be later in onset and/or reduced in magnitude in Black compared with White subjects.
Vascular effects of eutectic lidocaine/prilocaine cream, such as skin blanching (reflecting vasoconstriction) and erythema (indicating vasodilatation), have occurred after application times of 30 to 60 minutes, and 2 hours, respectively. While the vasoconstriction may be partly associated with the technique of applying eutectic lidocaine/prilocaine cream under occlusion, the vasodilatation appears to be a specific effect of eutectic lidocaine/prilocaine cream. Notwithstanding the possible occurrence of vasoconstriction, eutectic lidocaine/prilocaine cream does not appear to compromise the efficacy of pulsed dye laser treatment of port wine stains. Vascular responses may be greater when eutectic lidocaine/prilocaine cream is applied to diseased skin.
Eutectic lidocaine/prilocaine cream appears to inhibit the flare, but not the wheal, response to histamine, indicating that it alleviates the neurogenic component of inflammation.
Pharmacokinetic Properties
The rates of percutaneous absorption of lidocaine and prilocaine vary according to the location and condition of the skin. Moreover, plasma prilocaine concentrations tend to be lower than those of lidocaine. Maximum plasma concentrations of the anaesthetics were attained within 2 to 2.5 hours of applying eutectic lidocaine/prilocaine cream to normal facial skin. In contrast, the maximum plasma lidocaine concentration was lower (18 vs 150 μg/L) and not reached until 5 hours after the same dosage (10 g/100cm2 for 2 hours) was first applied to normal forearm skin. Studies in children and infants have revealed that widely varying maximum plasma lidocaine and prilocaine concentrations can be expected within 2 to 4 hours of applying the cream to normal skin.
The rate of percutaneous absorption of lidocaine and prilocaine from skin affected by psoriasis or dermatitis appears to be increased compared with normal skin. Reported plasma concentrations of lidocaine were in the range 16 to 450 μg/L 1 hour after applying eutectic lidocaine/prilocaine cream (4 to 6 g/25cm2) to the skin of patients with these conditions. A study in children about to undergo surgical treatment of molluscum contagiosum reported that maximum plasma anaesthetic concentrations were reached within 2 to 3 hours of applying a total dose of 10 to 16g eutectic lidocaine/prilocaine cream to a total of 100 to 160cm2 of affected skin.
Maximum plasma anaesthetic concentrations following application of eutectic lidocaine/prilocaine cream were 10- to 100-fold less than those considered toxic.
Clinical Efficacy
Almost all of the clinical studies on the use of eutectic lidocaine/prilocaine cream as a local anaesthetic have been in patients undergoing minor medical and surgical procedures.
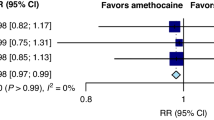
Controlled trials have demonstrated analgesic efficacy of eutectic lidocaine/prilocaine cream significantly greater than that of placebo in children aged between 3 months and 17 years undergoing venipuncture or venous cannulation, and it was reported to facilitate the procedure in some, but not all, studies. In addition, the analgesic efficacy of eutectic lidocaine/prilocaine cream was equivalent to that of lidocaine infiltration or ethyl chloride spray in children undergoing venous cannulation. Initial reports have shown that the patch formulation offers a suitable alternative to the cream in children undergoing venipuncture. Two double-blind trials in paediatric patients undergoing lumbar puncture found that the analgesic efficacy of eutectic lidocaine/prilocaine cream was significantly greater than that of placebo.
In adults undergoing arterial cannulation prior to surgery, eutectic lidocaine/prilocaine cream treatment was associated with lower pain scores than placebo, and compared with lidocaine infiltration in 1 double-blind study. In patients undergoing cannulation for haemodialysis, use of eutectic lidocaine/prilocaine cream was not only associated with significantly greater pain relief than placebo, but also significantly facilitated cannulation in comparison with both placebo and lidocaine infiltration. Controlled trials of the use of eutectic lidocaine/prilocaine cream prior to venipuncture in adults have also shown significant benefit over placebo.
In patients undergoing split-skin graft harvesting, eutectic lidocaine/prilocaine cream (30 g/100cm2) provided satisfactory analgesia in approximately 90% of patients. In children undergoing curettage of molluscum contagiosum lesions, pain after eutectic lidocaine/prilocaine cream treatment was rated as ‘none’ or ‘slight’ in over 90% of patients, vs 54% with placebo. Eutectic lidocaine/prilocaine cream has also been effective in relieving pain in patients undergoing laser treatment of facial port wine stains, was superior to placebo in patients undergoing surgical debridement of leg ulcers and equivalent to prilocaine infiltration in patients undergoing punch or excision skin biopsy.
Eutectic lidocaine/prilocaine cream (at least 1g/lesion) has provided effective analgesia for removal of condylomata acuminata in both men and women in several controlled trials, with eutectic lidocaine/prilocaine cream providing a satisfactory, and more comfortable, alternative to lidocaine infiltration in 2 studies. In female patients with lesions on vulval mucosal membranes, application times of 5 to 15 minutes appear to provide optimal analgesia.
In urology, eutectic lidocaine/prilocaine cream may be of benefit as an adjunct to extracorporeal shock wave lithotripsy for the removal of urinary calculi, with greater efficacy in males than females reported in 1 study. Efficacy equivalent to that of lidocaine infiltration has also been shown in a controlled study. Pilot studies and other preliminary trials of eutectic lidocaine/prilocaine cream in obstetrics, gynaecology and andrology have indicated benefit in a variety of procedures, including laser treatment of cervical intraepithelial neoplasia, vulval biopsy, lumbar epidural catheterisation in labour, drainage of non-lactational breast abscesses, and separation of preputial adhesions in boys.
There have been a number of studies indicating efficacy of eutectic lidocaine/prilocaine cream for local anaesthesia of the tympanic membrane during myringotomy and ventilation tube insertion, in patients without tympanic perforation. Analgesic efficacy with eutectic lidocaine/prilocaine cream appears to be similar to that of lidocaine iontophoresis, prilocaine injection, or cocaine. While eutectic lidocaine/prilocaine cream was more convenient to use than the other agents, it should not be used in patients in whom penetration of the cream to the middle ear is possible.
Other potentially painful procedures in which eutectic lidocaine/prilocaine cream has been studied include retrobulbar injection in cataract surgery, removal of arch bars in mandibular fracture, dermal puncture in electromyography, and paediatric percutaneous renal biopsy.
Tolerability
Local skin reactions (mainly blanching and erythema) have occurred in 56% of patients treated with eutectic lidocaine/prilocaine cream. These effects are mild and transient, and resolve spontaneously within 1 to 2 hours after removing the cream.
Methaemoglobinaemia, attributed to a metabolite of prilocaine, has been reported in an infant aged 3 months treated with eutectic lidocaine/prilocaine cream and receiving concomitant cotrimoxazole (trimethoprim/sulfamethoxazole) administration, which may also be associated with this adverse event. A subsequent study in infants less than 3 months of age, while noting statistically significant small increases in methaemoglobin levels, did not observe clinically significant methaemoglobinaemia in any infant; similar findings were reported from studies in children aged between 3 months and 6 years. Use of eutectic lidocaine/prilocaine cream is, however, contraindicated in infants less than 3 months of age.
Dosage and Administration
A thick layer of eutectic lidocaine/prilocaine cream 5% is applied to intact skin under an occlusive dressing for at least 1 hour before the procedure. For needle insertion or surgical treatment of localised lesions, approximately 2.5g of the cream should be applied to 20 to 25cm2 of skin. For more painful procedures that involve larger areas of skin, approximately 1.5 to 2g/10cm2 should be applied for at least 2 hours.
In infants aged less than 12 months, eutectic lidocaine/prilocaine cream should not be applied for more than 4 hours. Its use is contraindicated in all infants aged less than 3 months and in those aged up to 12 months who are also receiving methaemoglobin-inducing agents.
Eutectic lidocaine/prilocaine cream should not be used in any clinical situation in which its penetration beyond the tympanic membrane is possible.
Similar content being viewed by others
References
Amdisen A, Glud V. No influence from topical application of EMLA® cream before blood sampling on routine clinical chemistry and haematology measurements. European Journal of Clinical Pharmacology 41: 619–620, 1991
Andersen C, Danielson K, Ladefoged J. EMLA cream for pain prevention in hemodialysis patients. Dialysis and Transplantation 18: 684–685, 1989
Anniko M, Hellström S, Schmidt S-H, Spandow O. Toxic effects on inner ear of noxious agents passing through the round window membrane. Acta Oto-Laryngologica Suppl. 457: 49–56, 1988
Anniko M, Schmidt S-H. The ototoxic potential for EMLA. A new local anesthetic for the tympanic membrane. Acta Oto-Laryngologica 105: 255–265, 1988
Anon. Eutectic lidocaine/prilocaine cream prescribing information, USA, 1992
Arendt-Nielsen L, Bjerring P. Laser-induced pain for evaluation of local analgesia: A comparison of topical application (EMLA) and local injection (lidocaine). Anesthesia and Analgesia 67: 115–123, 1988
Arendt-Nielsen L, Bjerring P. The effect of topically applied anaesthetics (EMLA® cream) on thresholds to thermode and argon laser stimulation. Acta Anaesthesiologica Scandinavica 33: 469–473, 1989
Arendt-Nielsen L, Bjerring P, Nielsen J. Regional variations in analgesic efficacy of EMLA® cream. Quantitatively evaluated by argon laser stimulation. Acta Dermato-Venereologica 70: 314–318, 1990
Ashinoff R, Geronemus RG. Effect of the topical anesthetic EMLA on the efficacy of pulsed dye laser treatment of port-wine stains. Journal of Dermatologic Surgery and Oncology 16: 1008–1011, 1990
Bierkens AF, Maes RM, Hendrikx AJM, Erdos AF, de Vries JDM, et al. The use of local anesthesia in second generation extra-corporeal shock wave lithotripsy: eutectic mixture of local anesthetics. Journal of Urology 146: 287–289, 1991
Bingham B, Hawthorne M. The use of anaesthetic EMLA cream in minor otological surgery. Journal of Laryngology and Otology 102: 517, 1988
Bjerring P, Andersen PH, Arendt-Nielsen L. Vascular response of human skin after analgesia with EMLA cream. British Journal of Anaesthesia 63: 655–660, 1989
Bjerring P, Arendt-Nielsen L. Depth and duration of skin analgesia to needle insertion after topical application of EMLA cream. British Journal of Anaesthesia 64: 173–177, 1990a
Bjerring P, Arendt-Nielsen L. A quantitative comparison of the effect of local analgesics on argon laser induced cutaneous pain and on histamine induced wheal, flare and itch. Acta Dermato-Venereologica 70: 126–131, 1990b
Brodin A, Nyqvist-Mayer A, Wadsten T, Forslund B, Broberg F. Phase diagram and aqueous solubility of the lidocaine-prilocaine binary system. Journal of Pharmaceutical Sciences 73: 481–484, 1984
Byrne M, Taylor-Robinson D, Harris JRW. Topical anaesthesia with lidocaine-prilocaine cream for vulval biopsy. British Journal of Obstetrics and Gynaecology 96: 497–499, 1989
Clarke S, Radford M. Topical anaesthesia for venepuncture. Archives of Disease in Childhood. Journal of the British Paedi-atric Association 61: 1132–1134, 1986
Collins D. EMLA cream and herpetic neuralgia. Correspondence. Medical Journal of Australia 155: 206–207, 1991
Cooper CM, Gerrish SP, Hardwick M, Kay R. EMLA cream reduces the pain of venepuncture in children. European Journal of Anaesthesiology 4: 441–448, 1987
de Jong PC, Verburg MP, Lillieborg S. EMLA® cream versus ethyl-chloride spray: a comparison of the analgesic efficacy in children. European Journal of Anaesthesiology 7: 473–481, 1990
de Waard-van der Spek FB, Oranje AP, Lillieborg S, Hop WCJ, Stolz E. Treatment of molluscum contagiosum using a lidocaine/prilocaine cream (EMLA) for analgesia. Journal of the American Academy of Dermatology 23: 685–688, 1990
Dixon JM. Outpatient treatment of non-lactational breast abscesses. British Journal of Surgery 79: 56–57, 1992
Dohlwitz A, Uppfeldt A. Schmerzlinderung bei Venenpunkion. Applikation und Wirksamkeit einer Lidocain-Prilocain-Creme. Anaesthesist 34: 355–358, 1985
Dybvik T, Kolflaath J. EMLA-krem — lokalbedøvelse ved innlegging av perifert venest kateter (Venflon) hos barn. Tidsskrift For Den Norske Laegeforening 106: 2829–2830, 1986
Ehrenström Reiz GME, Reiz SLA. EMLA — a eutectic mixture of local anaesthetics for topical anaesthesia. Acta Anaesthesiologica Scandinavica 26: 596–598, 1982
Ehrenströom-Reiz G, Reiz S, Stockman O. Topical anaesthesia with EMLA, a new lidocaine-prilocaine cream and the cusum technique for detection of minimal application time. Acta Anaesthesiologica Scandinavica 27: 510–512, 1983
El-Kholy A. Manipulation of the fractured nose using topical local anaesthesia. Journal of Laryngology and Otology 103: 580–581, 1989
Enander Malmros I, Nilsen T, Lillieborg S. Plasma concentrations and analgesic effect of EMLA® (lidocaine/prilocaine) cream for the cleansing of leg ulcers. Acta Dermato-Venereologica 70: 227–230, 1990
Engberg G, Danielson K, Henneberg S, Nilsson A. Plasma concentrations of prilocaine and lidocaine and methaemoglobin formation in infants after epicutaneous application of a 5% lidocaine-prilocaine cream (EMLA). Acta Anaesthesiologica Scandinavica 31: 624–628, 1987
Evers H, von Dardel O, Juhlin L, Ohlsén L, Vinnars E. Dermal effects of compositions based on the eutectic mixture of lignocaine and prilocaine (EMLA). Studies in volunteers. British Journal of Anaesthesia 57: 997–1005, 1985
Fitzgerald M, Millard C, McIntosh N. Cutaneous hyersensitivity following peripheral tissue damage in newborn infants and its reversal with topical anaesthesia. Pain 39: 31–36, 1989
Frayling IM, Addison GM, Chattergee K, Meakin G. Methaemoglobinaemia in children treated with prilocaine-lignocaine cream. British Medical Journal 301: 153–154, 1990
Goodacre TEE, Sanders R, Watts DA, Stoker M. Split skin grafting using topicl local anaesthesia (EMLA): a comparison with infiltrated anaesthesia. British Journal of Plastic Surgery 41: 533–538, 1988
Gunawardene RD, Davenport HT. Local application of EMLA and glyceryl trinitrate ointment before venepuncture. Anaesthesia 45: 52–54, 1990
Haasio J, Jokinen T, Numminen M, Rosenberg PH. Topical anaesthesia of gingival mucosa by 5% eutectic mixture of lignocaine and prilocaine or by 10% lignocaine spray. British Journal of Oral and Maxillofacial Surgery 28: 99–101, 1990
Hallén B, Carlsson P, Uppfeldt A. Clinical study of a lignocaineprilocaine cream to relieve the pain of venepuncture. British Journal of Anaesthesia 57: 326–328, 1985
Hallén A, Ljunghall K, Wallin J. Topical anaesthesia with local anaesthetic (lidocaine and prilocaine, EMLA) cream for cautery of genital warts. Genitourinary Medicine 63: 316–319, 1987
Hallén B, Olsson GL, Uppfeldt A. Pain-free venepuncture. Effect of timing of application of local anaesthetic cream. Anaesthesia 39: 969–972, 1984
Hallén B, Uppfeldt A. Does lidocaine-prilocaine cream permit painfree insertion of IV catheters in children? Anesthesiology 57: 340–342, 1982
Halperin DL, Koren G, Attias D, Pellegrini E, Greenberg ML, et al. Topical skin anesthesia for venous, subcutaneous drug reservoir and lumbar punctures in children. Pediatrics 84: 281–284, 1989
Haugstvedt S, Friman A-M, Danielson K. Plasma concentrations of lidocaine and prilocaine and analgesic effect after dermal application of EMLA® cream 5% for surgical removal of mollusca in children. Zeitschrift für Kinderchirurgie 45: 148–150, 1990
Harper EI, Swanson Beck J, Spence VA. Effect of topically applied local anaesthesia on histamine flare in man measured by laser Doppler velocimetry. Agents and Actions 28: 192–197, 1989
Hellgren U, Kihamia CM, Premji Z, Danielson K. Local anaesthetic cream for the alleviation of pain during venepuncture in Tanzanian schoolchildren. British Journal of Clinical Pharmacology 28: 205–206, 1989
Holm J, Andrén B, Grafford K. Pain control in the surgical debridement of leg ulcers by the use of a topical lidocaine-prilocaine cream, EMLA®. Acta Dermato-Venereologica 70: 132–136, 1990
Hoist A, Evers H. Experimental studies of new topical anaesthetics on the oral mucosa. Swedish Dental Journal 9: 185–191, 1985
Honnens de Lichtenberg M, Krogh J, Rye B, Miskowiak J. Topical anesthesia with eutetic mixture of local anesthetics cream in vasectomy: 2 randomized trials. Journal of Urology 147: 98–99, 1992b
Honnens de Lichtenberg M, Miskowiak J, Mogensen P, Andersen JT. Local anesthesia for extracorporeal shock wave lithotripsy. A study comparing eutetic mixture of local anesthetics cream and lidocaine infiltration. Journal of Urology 147: 96–97, 1992a
Hopkins CS, Buckley CJ, Bush GH. Pain-free injection in infants. Use of a lignocaine-prilocaine cream to prevent pain at intravenous induction of general anaesthesia in 1–5-year-old children. Anaesthesia 43: 198–201, 1988
Hymes JA, Spraker MK. Racial differences in the effectiveness of a topically applied mixture of local anesthetics. Regional Anesthesia 11: 11–13, 1986
Jakobson B, Nilsson A. Methemoglobinemia associated with a prilocaine-lidocaine cream and trimetoprim-sulphamethoxazole. A case report. Acta Anaesthesiologica Scandinavica 29: 453–455, 1985
Jones SK, Handfield-Jones S, Kennedy CTC. Does EMLA reduce the discomfort associated with local-anaesthetic infiltration? Clinical and Experimental Dermatology 15: 177–179, 1990
Joyce TH, Skjonsby BS, Taylor BD, Morrow DH, Hess KR. Dermal anesthesia using a eutectic mixture of lidocaine and prilocaine (EMLA) for venipuncture in children. Pain Digest 2: 137–141, 1992
Juhlin TH, Evers H. EMLA: a new topical anesthetic. Advances in Dermatology 5: 75–92, 1990
Juhlin L, Hägglund G, Evers H. Absorption of lidocaine and prilocaine after application of a eutectic mixture of local anesthetics (EMLA®) on normal and diseased skin. Acta Dermato-Venereologica 69: 18–22, 1989
Juhlin L, Rollman O. Vascular effects of a local anesthetic mixture in atopic dermatitis. Acta Dermato-Venereologica 64: 439, 1984
Kapelushnik J, Koren G, Solh H, Greenberg M, DeVeber L. Evaluating the efficacy of EMLA in alleviating pain associated with lumbar puncture; comparison of open and double-blinded protocols in children. Pain 42: 31–34, 1990
Kurien L, Kollberg H, Uppfeldt A. Venepuncture pain can be reduced. Journal of Tropical Medicine and Hygiene 88: 397–399, 1985
Lähteenmäki T, Lillieborg S, Ohlsén L, Olenius M, Strömbeck JO. Topical analgesia for the cutting of slit-skin grafts: a multicenter comparison of two doses of a lidocaine/prilocaine cream. Journal of the American Society of Plastic and Reconstructive Surgeons 82: 458–462, 1988
Lamarche Y, Lebel M, Martin R. EMLA partially relieves the pain of EMG needling. Canadian Journal of Anaesthesia 39: 805–808, 1992
Lanigan SW, Cotterill JA. Use of a lignocaine-prilocaine cream as an analgesic in dye laser treatment of port-wine stains. Lasers in Medical Science 2: 87–89, 1987
Lassus A, Kartamaa M, Happonen H-P. A comparative study of topical analgesia with a lidocaine/prilocaine cream (EMLA®) and infiltration anesthesia for laser surgery of genital warts in men. Sexually Transmitted Diseases 17: 130–132, 1990
Ljunghall K, Lillieborg S. Local anaesthesia with a lidocaine/prilocaine cream (EMLA®) for cautery of condylomata acuminata on the vulval mucosa. The effect of timing of application of the cream. Acta Dermato-Venereologica 69: 362–365, 1989
Lowrie A, Jones MJ, Eastley RJ. Effect of a eutectic mixture of local anaesthetic agents (EMLA) on tourniquet pain in volunteers. British Journal of Anaesthesia 63: 751–753, 1989
Luotonen J, Laitakari K, Karjalainen H, Jokinen K. EMLA® in local anaesthesia of the tympanic membrane. Acta Oto-Laryngologica Suppl. 492: 63–67, 1992
MacKinlay GA. Save the prepuce. Painless separation of preputial adhesions in the outpatient clinic. British Medical Journal 297: 590–591, 1988
Maddi R, Horrow JC, Mark JB, Concepcion M, Murray E. Evaluation of a new cutaneous topical anesthesia preparation. Regional Anesthesia 15: 109–112, 1990
Manner T, Kanto J, Iisalo E, Lindberg R, Viinamäki O, Scheinin M. Reduction of pain at venous cannulation in children with a eutectic mixture of lidocaine and prilocaine (EMLA® cream): comparison with placebo cream and no local premedication. Acta Anaesthesiologica Scandinavica 31: 735–739, 1987
Maunuksela E-L, Korpela R. Double-blind evaluation ol a lignocaine-prilocaine cream (EMLA) in children. Effect on the pain associated with venous cannulation. British Journal of Anaesthesia 58: 1242–1245, 1986
McDonald PF, Berry AM. Topical anaesthesia for extracorporeal shock wave lithotripsy. British Journal of Anaesthesia 69: 399–400, 1992
Milligan K, Atkinson RE, Schofield PA. Lignocaine-prilocaine cream in postherpetic neuralgia. Correspondence. British Medical Journal 298: 253, 1989
Möller C. A lignocaine-prilocaine cream reduces venipuncture pain. Upsala Journal of Medical Sciences 90: 293–398, 1985
Monk TG, Ding Y, White PF. Analgesic efficacy of EMLA during outpatient shock-wave lithotripsy. Abstract. Anesthesia and Analgesia 74: S213, 1992
Nielsen JC, Arendt-Nielsen L, Bjerring P, Svensson P. The analgesic effect of EMLA cream on facial skin. Quantitative evaluation using argon laser stimulation. Acta Dermato-Venereologica 72: 281–284, 1992
Nilsson A, Danielson K, Engberg G, Henneberg S. Emla for pain relief during arterial cannulation. A double-blind, placebo-controlled study of a lidocaine-prilocaine cream. Upsala Journal of Medical Sciences 95: 87–94, 1990
Nilsson A, Engberg G, Henneberg S, Danielson K, de Verdier C-H. Inverse relationship between age-dependent erythrocyte activity of methaemoglobin reductase and prilocaine-induced methaemoglobinaemia during infancy. British Journal of Anaesthesia 64: 72–76, 1990
Nott MR, Peacock JL. Relief of injection pain in adults. EMLA cream for 5 minutes before venepuncture. Anaesthesia 45: 772–774, 1990
Nyqvist-Mayer AA, Brodin AF, Frank SG. Drug release studies on an oil-water emulsion based on a eutectic mixture of lidocaine and prilocaine as the dispersed phase. Journal of Pharmaceutical Sciences 75: 365, 1986
Nyqvist-Mayer AA, Brodin AF, Frank SG. Phase distribution studies on an oil-water emulsion based on a eutectic mixture of lidocaine and prilocaine as the dispersed phase. Journal of Pharmaceutical Sciences 74: 1192–1195, 1985
Ogborn MR. The use of a eutectic mixture of local anesthetic in pediatric renal biopsy. Pediatric Nephrology 6: 276–277, 1992
Ohlsén L, Englesson S, Evers H. An anaesthetic lidocaine/prilocaine cream (EMLA) for epicutaneous application tested for cutting split skin grafts. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery 19: 201–209, 1985
Pepall LM, Cosgrove MP, Cunliffe WJ. Ablation of whiteheads by cautery under topical anaesthesia. British Journal of Dermatology 125: 256–259, 1991
Pere P, Iizuka T, Rosenberg PH, Lindqvist C. Topical application of 5% eutectic mixture of lignocaine and prolocaine (EMLA®) before removal of arch bars. British Journal of Oral and Maxillofacial Surgery 30: 153–156, 1992
Piazolo P, Brech W, Bissinger KR, Hailer D, Hardt D. Emla-Creme (eutektische Mixtur von Lokalanästhetika) verhindert den Shunt-Punktionsschmerz bei Hämodialysepatienten im Doppelblind-Vergleich mit Plazebo. Nieren-Und Hochdruckkrankheiten 17: 236–240, 1988
Pipkorn U, Andersson M. Topical dermal anaesthesia inhibits the flare but not the weal response to allergen and histamine in the skin-prick test. Clinical Allergy 17: 307–311, 1987
Premachandra DJ. Use of EMLA cream as an analgesic in the management of painful otitis externa. Journal of Laryngology and Otology 104: 887–888, 1990
Radford M, Pinder A-M. Methaemoglobinaemia in children treated with prilocaine-lignocaine cream. Correspondence. British Medical Journal 301: 495, 1990
Ralston SJ, Head-Rapson AG. Use of EMLA cream for skin anaesthesia prior to epidural insertion in labour. Anaesthesia 48: 65–67, 1993
Randell T, Yli-Hankala A, Valli H, Lindgren L. Topical anaesthesia of the nasal mucosa for fibreoptic airway endoscopy. British Journal of Anaesthesia 68: 164–167, 1992
Roberts C, Carlin WV. A comparison of topical EMLA cream and prilocaine injection for anaesthesia of the tympanic membrane in adults. Acta Oto-Laryngologica 108: 431–433, 1989
Robieux I, Eliopoulos C, Hwang P, Greenberg M, Blanchette V, et al. Pain perception and effectiveness of the eutectic mixture of local anesthetics in children undergoing venipuncture. Pediatric Research 32: 520–523, 1992
Robieux I, Kumar R, Radhakrishnan S, Koren G. Assessing pain and analgesia with a lidocaine-prilocaine emulsion in infants and toddlers during venipuncture. Journal of Pediatrics 118: 971–973, 1991
Rosdahl I, Edmar B, Gisslén H, Nordin P, Lillieborg S. Curettage of molluscum contagiosum in children: analgesia by topical application of a lidocaine/prilocaine cream (EMLA®). Acta Dermato-Venereologica 68: 149–153, 1988
Russell GN, Desmond MJ, Fox MA. Local anesthesia for radial artery cannulation: a comparison of a lidocaine-prilocaine emulsion and lidocaine infiltration. Journal of Cardiothoracic Anesthesia 2: 309–312, 1988
Rylander E, Sjöberg I, Lillieborg S, Stockman O. Local anesthesia of the genital mucosa with a lidocaine/prilocaine cream (EMLA) for laser treatment of condylomata acuminata. A placebo-controlled study. Obstetrics and Gynecology 75: 302–306, 1990
Sarkar PK. Topical anaesthesia with lignocaine-prilocaine cream (EMLA) for carbon dioxide treatment to the cervix. A pilot study. British Journal of Clinical Pharmacology 44: 352–353, 1990
Shuttleworth D, Hill S, Marks R, Connelly DM. Relief of experimentally induced pruritus with a novel eutectic mixture of local anaesthetic agents. British Journal of Dermatology 119: 535–540, 1988
Simons FER, Gillespie CA, Simons KJ. Local anaesthetic creams and intradermal skin tests. Correspondence. Lancet 339: 1351–1352, 1992
Sims C. Thickly and thinly applied lignocaine-prilocaine cream prior to venepuncture in children. Anaesthesia and Intensive Care 19: 343–345, 1991
Sirimanna KS, Madden GJ, Miles S. Anaesthesia of the tympanic membrane: comparison of EMLA cream and iontophoresis. Journal of Laryngology and Otology 104: 195–196, 1990
Smith M, Gray BM, Ingram S, Jewkes DA. Double-blind comparison of topical lignocaine-prilocaine cream (EMLA) and lignocaine infiltration for arterial cannulation in adults. British Journal of Anaesthesia 65: 240–242, 1990
Soliman IE, Broadman LM, Hannallah RS, McGill WA. Comparison of the analgesic effects of EMLA (eutectic mixture of local anesthetics) to intradermal lidocaine infiltration prior to venous cannulation in unpremedicated children. Anesthesiology 68: 804–806, 1988
Steward D, Goresky G, O’Connor G, Pyesmany DA, Rogers PCJ, et al. A single unit dose EMLA patch compared to 5% EMLA cream used to reduce pain from venepuncture in children: a multicenter randomised study. Abstract. 10th World Congress of Anaesthesiologists, The Hague, June 12–19, 1992
Stow PJ, Glynn CJ, Minor B. EMLA cream in the treatment of post-herpetic neuralgia. Efficacy and pharmacokinetic profile. Pain 39: 301–305, 1989
Strömbeck JO, Uggla M, Lillieborg S. Percutaneous anaesthesia with a lidocaine-prilocaine cream (EMLA®) for cutting split-skin grafts. European Journal of Plastic Surgery 11: 49–52, 1988
Sunderraj P, Kirby J, Joyce PW, Watson A. A double-masked evaluation of lignocaine-prilocaine cream (EMLA) used to alleviate the pain of retrobulbar injection. British Journal of Ophthalmology 75: 130–132, 1991
Taddio A, Robieux I, Koren G. Effect of lidocaine-prilocaine cream on pain from subcutaneous injection. Clinical Pharmacy 11: 347–349, 1992
Tan OT, Stafford TJ. EMLA for laser treatment of portwine stains in children. Lasers in Surgery and Medicine 12: 543–548, 1992
Thune P, Faerden F, Minor BG. The analgesic effect of EMLA cream for skin biopsies. Journal of Dermatological Treatment 1: 239–241, 1990
Tiselius H-G. Cutaneous anesthesia with lidocaine-prilocaine cream: a useful adjunct during shock wave lithotripsy with analgesic sedation. Journal of Urology 149: 8–11, 1993
van den Berg GM, Lillieborg S, Stolz E. Lidocaine/prilocaine cream (EMLA(R)) versus infiltration anaesthesia: a comparison of the analgesic efficacy for punch biopsy and electrocoagulation of genital warts in men. Genitourinary Medicine 68: 162–165, 1992
Villada G, Zetlaoui J, Revuz J. Local blanching after epicutaneous application of EMLA cream. A double-blind randomized study among 50 healthy volunteers. Dermatologica 181: 38–40, 1990
Watson AR, Szymkiw P, Morgan AG. Topical anaesthesia for fistula cannulation in haemodialysis patients. Nephrology Dialysis Transplantation 3: 800–802, 1988
Wehle B, Björnström M, Cedgard M, Danielsson K, Ekernãs A, et al. Repeated application of EMLA cream 5% for the alleviation of cannulation pain in haemodialysis. Scandinavian Journal of Urology and Nephrology 23: 299–302, 1989
Wheeler JG. Emla cream and herpetic neuralgia. Correspondence. Medical Journal of Australia 155: 781, 1991
Whittet HB, Williams HO, Wright A. An evaluation of topical anaesthesia for myringotomy. Clinical Otolaryngology 13: 481–484, 1988
Wig J, Johl KS. Our experience with EMLA cream (for painless venous cannulation in children). Indian Journal of Physiology Pharmac. 34: 130–132, 1990
Williams AR. Phonophoresis: an in vivo evaluation using three topical anaesthetic preparations. Ultrasonics 28: 137–141, 1990
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: T.E.C. Bushell, Royal West Sussex Hospital, Chichester, England; F.B. de Waard-van der Spek, Subdivision of Paediatric Dermatology, Sophia Children’s Hospital, Rotterdam, The Netherlands; S.K. Jones, Department of Dermatology, Bristol Royal Infirmary, Bristol, England; L. Juhlin, Department of Dermatology, University Hospital, Uppsala, Sweden; G. Koren, Division of Clinical Pharmacology, The Hospital for Sick Children, Toronto, Ontario, Canada; H.I. Maibach, Department of Dermatology, University of California at San Francisco, School of Medicine, San Francisco, California, USA; B. Mets, Department of Anesthesiology, College of Physicians and Surgeons of Columbia University, New York, New York, USA; A.P. Oranje, Subdivision of Paediatric Dermatology, Sophia Children’s Hospital, Rotterdam, The Netherlands; B. Page Keller, Department of Anesthesiology, University of Missouri, Columbia, Missouri, USA; P.H. Rosenberg, Department of Anaesthesiology, Helsinki University Central Hospital, Helsinki, Finland; F. Wood, Princess Margaret Hospital for Children, Perth, Australia.
Eutectic lidocaine/prilocaine cream is frequently referred to in the literature by the acronym EMLA. ‘EMLA’ is also the registered brandname.
Rights and permissions
About this article
Cite this article
Buckley, M.M., Benfield, P. Eutectic Lidocaine/Prilocaine Cream. Drugs 46, 126–151 (1993). https://doi.org/10.2165/00003495-199346010-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199346010-00008