Abstract
Background and objective
An economic analysis of telemedicine support to improve glycemic control in patients with type 2 diabetes mellitus, illustrating the use of an analytic framework that efficiently combines telemedicine program findings with published estimates of treatment cost effectiveness.
Method
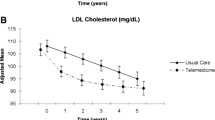
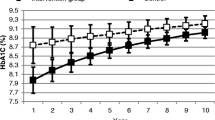
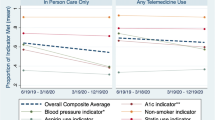
The Pro-Active Call Centre Treatment Support (PACCTS) trial compared tailored, protocol-driven call-center support with usual care as methods to manage glycemic control in 591 patients with diabetes in Salford, UK. Economic analysis of the trial describes the cost of delivering telemedicine support and level of improved glycemic control achieved in patients. These findings are linked to current best evidence for the long-term cost effectiveness of treatment to help inform whether the provision of call-center support to improve glycemic control should become routine health policy.
Results
Under trial conditions, the cost effectiveness of the PACCTS intervention was estimated to be £43 400/ quality-adjusted life-year (QALY) [2003 costings]. Under routine-use call-center conditions (a full caseload of patients with moderate to poor glycemic control) cost effectiveness was estimated to be lower at £33 700/QALY. Set against a threshold of £30 000/QALY, Monte Carlo simulation suggests the probability of PACCTS being cost-effective in routine use is 29%.
Discussion
Despite being received well by patients and healthcare professionals alike, telemedicine support solely to achieve improved glycemic control in patients with type 2 diabetes was found to be borderline cost effective. Major uncertainties that could change this result include the underlying cost effectiveness of improved glycemic control, which is currently imprecisely known. Research is ongoing in patients with type 2 diabetes to extend call-center support to improve blood pressure and lipid management, where if similar improvements are obtained, the call center should prove highly cost effective. The novel analytic approach illustrated provides a clear framework for thinking about the design and analysis of behavioral change policies for healthcare.






Similar content being viewed by others
References
Currell R, Urquhart C, Wainwright P, et al. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes (Cochrane Review). In: The Cochrane Library, Issue 3, 2003. Oxford: Update Software
Edworthy SM. Telemedicine in developing countries. BMJ 2001; 323: 524–5
Finch T, May C, Mair F, et al. Integrating service development with evaluation in telehealthcare: an ethnographic study. BMJ 2003; 327(7425): 1205–9
Foy R, Eccles M, Grimshaw J. Why does primary care need more implementation research? Fam Pract 2001; 4: 353–5
Whitten P, Mair F, Haycox A, et al. Systematic review of cost effectiveness studies of telehealthcare interventions: economic benefits of new technology are assumed, rather than known. BMJ 2002; 324: 1434–7
Mason J, Freemantle N, Nazareth I, et al. When is it cost-effective to change the behaviour of health professionals? JAMA 2001; 286: 2988–92
United Kingdom Prospective Diabetes Study Group (UKPDS 33). Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet 1998; 352: 837–53
United Kingdom Prospective Diabetes Study Group (UKPDS 34). Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes. Lancet 1998; 352: 854–65
Clarke PM, Gray AM, Briggs A, et al. UKPDS 72 United Kingdom Prospective Diabetes Study. Cost-utility analyses of intensive blood glucose and tight blood pressure control in type 2 diabetes (UKPDS 72). Diabetologia 2005 May; 48(5): 868–77
Gray A, Railour M, McGuire A, et al., on behalf of the United Kingdom Prospective Diabetes Study Group (UKPDS 41). Cost effectiveness of an intensive blood glucose control policy in patients with type 2 diabetes: economic analysis alongside randomised controlled trial. BMJ 2000; 320: 1372–8
Clarke P, Gray A, Adler A, et al., on behalf of the United Kingdom Prospective Diabetes Study Group (UKPDS 51). Cost-effectiveness analysis of intensive blood-glucose control with metformin in overweight patients with type II diabetes. Diabetologia 2001; 44: 298–304
CDC Diabetes Cost-Effectiveness Group. Cost-effectiveness of intensive glycaemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. JAMA 2002; 287: 2542–51
Owens DK. Interpretation of cost-effectiveness analysis. J Gen Intern Med 1998; 13: 716–7
World Health Organization. Purchasing power parities 1995–2000 [online]. Available from URL: http://www.who.int//choice/costs/ppp/en/ [Accessed 2006 Dec 19]
Burls A, Sandercock J. How to make a compelling submission to NICE: tips for sponsoring organisations. BMJ 2003; 327: 1446–8
Young RJ, Taylor J, Friede T, et al. Pro-Active Call Centre Treatment Support (PACCTS) to improve glucose control in type 2 diabetes: a randomised controlled trial. Diabetes Care 2005; 28: 278–82
Data Professional, Release 10. Copyright 1988–2003 [online]. TreeAge Software, Inc. Available from URL: http://www.treeage.com/ [Accessed 2006 Dec 20]
Hulscher MEJL, Wensing M, van der Weijden T, Grol R. Interventions to implement prevention in primary care (Cochrane Review). In: The Cochrane Library, Issue 3, 2003. Oxford: Update Software
Long AF, Gambling T, Young RJ, et al. Acceptability and satisfaction with a telecarer approach to the management of type 2 diabetes. Diabetes Care 2005; 28: 283–9
Department of Health. Standard General Medical Services Contract (27.02.04). Annex A: quality indicators - summary of points. 2004 [online]. Available from URL: http://www.dh.gov.uk/assetRoot/04/07/86/59/04078659.pdf [Accessed 2006 Dec 19]
Acknowledgments
This work was funded as part of an unrestricted academic (sub-contract) grant from Salford Hospital NHS Trust to provide research support, with funds originating from the study sponsors Glaxo Smith Kline and British Telecom. British Telecom acted as technology partners funding call center equipment and development and maintenance costs of the PACCTS trial. British Telecom is planning to market the PACCTS software. The authors have no other conflicts of interests that are directly relevant to the contents of this study. Ethical Approval: Salford & Trafford Research Ethics Committee (project 00199). This analysis was conceived and conducted by James M. Mason, assisted by Robert J. Young and John P. New. All authors contributed to interpreting findings and writing the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mason, J.M., Young, R.J., New, J.P. et al. Economic Analysis of a Telemedicine Intervention to Improve Glycemic Control in Patients with Diabetes Mellitus. Dis-Manage-Health-Outcomes 14, 377–385 (2006). https://doi.org/10.2165/00115677-200614060-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-200614060-00007