Ghrelin Restores the Disruption of the Circadian Clock in Steatotic Liver
Abstract
:1. Introduction
2. Results
2.1. Synchronization of the Circadian Rhythm of Primary Hepatocytes by Dexamethasone
2.2. Attenuation of the Rhythm of Core Clock Genes in Steatotic Liver
2.3. Restoration of the Rhythm of Core Clock Genes in Steatotic Liver by Ghrelin
2.4. Effects of GHSR1a Deletion on the Circadian Clock
2.5. Regulation of Hepatic mTOR Activity Rhythm by Ghrelin
3. Discussion
4. Materials and Methods
4.1. Materials
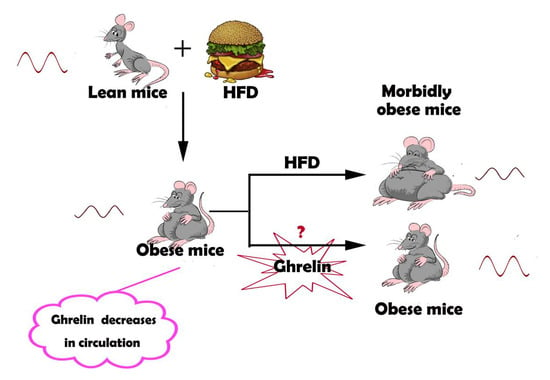
4.2. Animals and Treatment
4.3. Isolation and Synchronization of Hepatocytes
4.4. Western Blotting
4.5. Analysis of Gene Expression
4.6. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| SCN | Suprachiasmatic nucleus |
| ZT | Zeitgeber time |
| CT | Circadian time |
| CLOCK | Circadian Locomotor Output Cycles Kaput ear dichroism |
| BMAL1 | Brain and muscle ARNT-like protein 1 |
| PER | Period |
| CRY | Cryptochromes |
| REV-ERBα | Nuclear receptor subfamily 1, group D, member 1 |
| GHS-R1α | Growth hormone secretagogue receptor 1 |
| mTOR | Mechanistic target of rapamycin |
| NCD | Normal chaw diet |
| HFD | High-fat diet |
| S6 | S6 ribosomal protein |
References
- Takahashi, J.S.; Hong, H.K.; Ko, C.H.; McDearmon, E.L. The Genetics of Mammalian Circadian Order and Disorder: Implications for Physiology and Disease. Nat. Rev. Genet. 2008, 9, 764–775. [Google Scholar] [CrossRef] [PubMed]
- Berson, D.M.; Dunn, F.A.; Takao, M. Phototransduction by Retinal Ganglion Cells That Set the Circadian Clock. Science 2002, 295, 1070–1073. [Google Scholar] [CrossRef] [PubMed]
- Reinke, H.; Asher, G. Circadian Clock Control of Liver Metabolic Functions. Gastroenterology 2016, 150, 574–580. [Google Scholar] [CrossRef] [PubMed]
- Stow, L.R.; Gumz, M.L. The Circadian Clock in the Kidney. J. Am. Soc. Nephrol. 2011, 22, 598–604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zvonic, S.; Ptitsyn, A.A.; Conrad, S.A.; Scott, L.K.; Floyd, Z.E.; Kilroy, G.; Wu, X.; Goh, B.C.; Mynatt, R.L.; Gimble, J.M. Characterization of peripheral circadian clocks in adipose tissues. Diabetes 2006, 55, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Dibner, C.; Schibler, U.; Albrecht, U. The mammalian circadian timing system: Organization and coordination of central and peripheral clocks. Annu. Rev. Physiol. 2010, 72, 517–549. [Google Scholar] [CrossRef] [PubMed]
- Damiola, F.; Le Minh, N.; Preitner, N.; Kornmann, B.; Fleury-Olela, F.; Schibler, U. Restricted feeding uncouplescircadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus. Genes Dev. 2000, 14, 2950–2961. [Google Scholar] [CrossRef] [PubMed]
- Stokkan, K.A.; Yamazaki, S.; Tei, H.; Sakaki, Y.; Menaker, M. Entrainment of the Circadian Clock in the Liver by Feeding. Science 2001, 291, 490–493. [Google Scholar] [CrossRef] [PubMed]
- Song, B.J.; Rogulja, D. SnapShot: Circadian Clock. Cell 2017, 171, 1468. [Google Scholar] [CrossRef] [PubMed]
- Feng, D.; Lazar, M.A. Clocks, metabolism, and the epigenome. Mol. Cell 2012, 47, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Kohsaka, A.; Laposky, A.D.; Ramsey, K.M.; Estrada, C.; Joshu, C.; Kobayashi, Y.; Turek, F.W.; Bass, J. High-fat diet disrupts behavioral and molecular circadian rhythms in mice. Cell Metab. 2007, 6, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Giebultowicz, J.; Kapahi, P. Circadian clocks and metabolism: The nutrient-sensing AKT and TOR pathways make the link. Curr. Biol. 2010, 20, 608–609. [Google Scholar] [CrossRef] [PubMed]
- Mukherji, A.; Kobiita, A.; Damara, M.; Misra, N.; Meziane, H.; Champy, M.-F.; Chambon, P. Shifting eating to the circadian rest phase misaligns the peripheral clocks with the master SCN clock and leads to a metabolic syndrome. Proc. Natl. Acad. Sci. USA 2015, 112, 6691–6698. [Google Scholar] [CrossRef] [PubMed]
- Asher, G.; Sassonecorsi, P. Time for Food: The Intimate Interplay between Nutrition, Metabolism, and the Circadian Clock. Cell 2015, 161, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Inui, A.; Asakawa, A.; Bowers, C.Y.; Mantovani, G.; Laviano, A.; Meguid, M.M.; Fujimiya, M. Ghrelin, appetite, and gastric motility: The emerging role of the stomach as an endocrine organ. FASEB J. 2004, 18, 439–456. [Google Scholar] [CrossRef] [PubMed]
- Kojima, M.; Hosoda, H.; Date, Y.; Nakazato, M.; Matsuo, H.; Kangawa, K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 1999, 402, 656. [Google Scholar] [CrossRef] [PubMed]
- Lesauter, J.; Hoque, N.; Weintraub, M.; Pfaff, D.W.; Silver, R. Stomach ghrelin-secreting cells as food-entrainable circadian clocks. Proc. Natl. Acad. Sci. USA 2009, 106, 13582–13587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yannielli, P.C.; Molyneux, P.C.; Harrington, M.E.; Golombek, D.A. Ghrelin effects on the circadian system of mice. J. Neurosci. Off. J. Soc. Neurosci. 2007, 27, 2890–2895. [Google Scholar] [CrossRef] [PubMed]
- Silver, R.; Hoque, N.; LeSauter, J. Discovery of a putative food anticipatory circadian clock. Soc. Neurosci. Abstr. 2005, 31, 10–60. [Google Scholar]
- Buijs, R.M.; Kalsbeek, A. Hypothalamic integration of central and peripheral clocks. Nat. Rev. Neurosci. 2001, 2, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Hatori, M.; Vollmers, C.; Zarrinpar, A.; DiTacchio, L.; Bushong, E.A.; Gill, S.; Leblanc, M.; Chaix, A.; Joens, M.; Fitzpatrick, J.A.J.; et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012, 15, 848–860. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Xu, G.; Qin, Y.; Zhang, C.; Tang, H.; Yin, Y.; Xiang, X.; Li, Y.; Zhao, J.; Mulholland, M.; et al. Ghrelin promotes hepatic lipogenesis by activation of mTOR-PPARγ signaling pathway. Proc. Natl. Acad. Sci. USA 2014, 111, 13163–13168. [Google Scholar] [CrossRef] [PubMed]
- Blum, I.D.; Patterson, Z.; Khazall, R.; Lamont, E.W.; Sleeman, M.W.; Horvath, T.L.; Abizaid, A. Reduced anticipatory locomotor responses to scheduled meals in ghrelin receptor deficient mice. Neuroscience 2009, 164, 351–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tschop, M.; Weyer, C.; Tataranni, P.A.; Devanarayan, V.; Ravussin, E.; Heiman, M.L. Circulating ghrelin levels are decreased in human obesity. Diabetes 2001, 50, 707–709. [Google Scholar] [CrossRef] [PubMed]
- Haissaguerre, M.; Saucisse, N.; Cota, D. Influence of mTOR in energy and metabolic homeostasis. Mol. Cell. Endocrinol. 2014, 397, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Roderburg, C.; Urban, G.W.; Bettermann, K.; Vucur, M.; Zimmermann, H.; Schmidt, S.; Janssen, J.; Koppe, C.; Knolle, P.; Castoldi, M.; et al. Micro-RNA profiling reveals a role for miR-29 in human and murine liver fibrosis. Hepatology 2011, 53, 209–218. [Google Scholar] [CrossRef] [PubMed]









| Gene | Forward (5′-3′) | Reverse (5′-3′) |
|---|---|---|
| β-actin | ATCTGGCACCACACCTTC | AGCCAGGTCCAGACGCA |
| Bmal1 | TCAAGACGACATAGGACACCT | GGACATTGGCTAAAACAACAGTG |
| Clock | CAC TCT CAC AGC CCC ACT GTA | CCC CAC AAG CTA CAG GAG CAG |
| Cry1 | CACTGGTTCCGAAAGGGACTC | CTGAAGCAAAAATCGCCACCT |
| Per1 | CCAGCGTGTCATGATGACATAC | CTCTCCCGGTCTTGCTTCAG |
| Per2 | TGTGCGATGATGATTCGTGA | GGTGAAGGTACGTTTGGTTTGC |
| Rev-erbα | TCTCTCCGTTGGCATGTCTAGA | GCAAGCATCCGTTGCTTCTC |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Q.; Yin, Y.; Zhang, W. Ghrelin Restores the Disruption of the Circadian Clock in Steatotic Liver. Int. J. Mol. Sci. 2018, 19, 3134. https://doi.org/10.3390/ijms19103134
Wang Q, Yin Y, Zhang W. Ghrelin Restores the Disruption of the Circadian Clock in Steatotic Liver. International Journal of Molecular Sciences. 2018; 19(10):3134. https://doi.org/10.3390/ijms19103134
Chicago/Turabian StyleWang, Qin, Yue Yin, and Weizhen Zhang. 2018. "Ghrelin Restores the Disruption of the Circadian Clock in Steatotic Liver" International Journal of Molecular Sciences 19, no. 10: 3134. https://doi.org/10.3390/ijms19103134