Controllable Drug Release Behavior of Polylactic Acid (PLA) Surgical Suture Coating with Ciprofloxacin (CPFX)—Polycaprolactone (PCL)/Polyglycolide (PGA)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
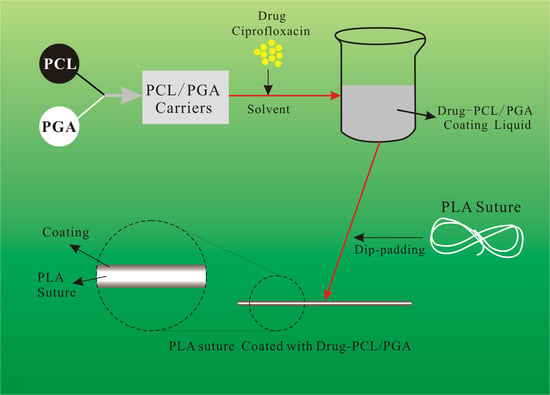
2.2. Preparation of Drug-Loaded Suture
2.3. Characterization
2.4. Drug Release Behavior In Vitro
3. Results and Discussion
3.1. Surface Morphology of Drug-Loaded PLA Suture
3.2. Chemical Structure of Drug-Loaded PLA Suture
3.3. Mechanical Properties of Drug-Loaded PLA Suture
3.4. Drug-Release Behavior of Drug-Loaded PLA Suture
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Valente, T.A.M.; Silva, D.M.; Gomes, P.S.; Fernandes, M.H.; Santos, J.D.; Sencadas, V. Effect of sterilization methods on electrospun poly(lactic acid) (PLA) fiber alignment for biomedical applications. Adv. Drug Deliver. Rev. 2016, 8, 3241–3249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madhavan, N.K.; Nair, N.R.; John, R.P. An overview of the recent developments in polylactide (PLA) research. Bioresource Technol. 2010, 101, 8493–8501. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.M.; Shive, M.S. Biodegradation and biocompatibility of PLA and PLGA microspheres. Adv. Drug Deliver. Rev. 2012, 64, 72–82. [Google Scholar] [CrossRef]
- Schrumpf, M.A.; Lee, A.T.; Weiland, A.J. Foreign-body reaction and osteolysis induced by an intraosseous poly-L-lactic acid suture anchor in the wrist: Case report. J. Hand Surg. 2011, 36, 1769–1773. [Google Scholar] [CrossRef] [PubMed]
- Nakano, Y.; Hori, Y.; Sato, A.; Watanabe, T.; Takada, S.; Goto, H.; Inagaki, A.; Ikada, Y.; Satomi, S. Evaluation of a poly(L-lactic acid) stent for sutureless vascular anastomosis. Ann. Vasc. Surg. 2009, 23, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Moy, R.L.; Kaufman, A.J. Clinical comparison of polyglactic acid (vicryl) and polytrimethylene carbonate (maxon) suture material. J. Dermatol. Surg. Oncol. 2013, 17, 667–669. [Google Scholar] [CrossRef]
- Gaynes, R.P.; Culver, D.H.; Horan, T.C.; Edwards, J.R.; Richards, C.; Tolson, J.S. Surgical site infection (SSI) rates in the united states, 1992-1998: The national nosocomial infections surveillance system basic SSI risk index. Clin. Infect. Dis. 2001, 33, S69–S77. [Google Scholar] [CrossRef]
- He, C.L.; Huang, Z.M.; Han, X.J. Fabrication of drug-loaded electrospun aligned fibrous threads for suture applications. J. Biomed. Mater. Res. A 2009, 89, 80–95. [Google Scholar] [CrossRef]
- Asri, L.A.T.W.; Crismaru, M.; Roest, S.; Chen, Y.; Ivashenko, O.; Rudolf, P.; Tiller, J.C.; van der Mei, H.C.; Loontjens, T.J.A.; Busscher, H.J. A shape-adaptive, antibacterial-coating of immobilized quaternary-ammonium compounds tethered on hyperbranched polyurea and its mechanism of action. Adv. Funct. Mater. 2014, 24, 346–355. [Google Scholar] [CrossRef]
- Varghese, N.M.; Venkatachalam, S.; Saxena, S.K. Nanocarriers for brain specific delivery of anti-retro viral drugs: Challenges and achievements. J. Drug Target. 2018, 26, 195–207. [Google Scholar] [CrossRef]
- Lee, E.J.; Huh, B.K.; Kim, S.N.; Lee, J.Y.; Park, C.G.; Mikos, A.G.; Bin Choy, Y. Application of materials as medical devices with localized drug delivery capabilities for enhanced wound repair. Prog. Mater. Sci. 2017, 89, 392–410. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, Z.; Stride, E.; Edirisinghe, M. Novel preparation of transdermal drug-delivery patches and functional wound healing materials. J. Drug Target. 2009, 17, 724–729. [Google Scholar] [CrossRef] [PubMed]
- Champeau, M.; Thomassin, J.M.; Tassaing, T.; Jerome, C. Drug loading of sutures by supercritical CO2 impregnation: Effect of polymer/ drug interactions and thermal transitions. Macromol. Mater. Eng. 2015, 300, 596–610. [Google Scholar] [CrossRef]
- Lee, D.H.; Kwon, T.Y.; Kim, K.H.; Kwon, S.T.; Cho, D.H.; Jang, S.H.; Son, J.S.; Lee, K.B. Anti-inflammatory drug releasing absorbable surgical sutures using poly(lactic-co-glycolic acid) particle carriers. Polym. Bull. 2014, 71, 1933–1946. [Google Scholar] [CrossRef]
- Weldon, C.B.; Tsui, J.H.; Shankarappa, S.A.; Nguyen, V.T.; Ma, M.L.; Anderson, D.G.; Kohane, D.S. Electrospun drug-eluting sutures for local anesthesia. J. Control. Release 2012, 161, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Toosi, S.; Naderi-Meshkin, H.; Kalalinia, F.; Peivandi, M.T.; HosseinKhani, H.; Bahrami, A.R.; Heirani-Tabasi, A.; Mirahmadi, M.; Behravan, J. PGA-incorporated collagen: Toward a biodegradable composite scaffold for bone-tissue engineering. J. Biomed. Mater. Res. A 2016, 104, 2020–2028. [Google Scholar] [CrossRef] [PubMed]
- Surucu, S.; Sasmazel, H.T. Development of core-shell coaxially electrospun composite PCL/chitosan scaffolds. Int. J. Biol. Macromol. 2016, 92, 321–328. [Google Scholar] [CrossRef]
- Liu, S.Q.; Wu, G.H.; Chen, X.G.; Zhang, X.F.; Yu, J.J.; Liu, M.F.; Zhang, Y.; Wang, P. Degradation behavior in vitro of carbon nanotubes (CNTs) /poly(lactic acid) (PLA) composite suture. Polymers 2019, 11, 01015. [Google Scholar] [CrossRef] [Green Version]
- Alonso, J.J.S.; El Kori, N.; Melian-Martel, N.; Del Rio-Gamero, B. Removal of ciprofloxacin from seawater by reverse osmosis. J. Environ. Manag. 2018, 217, 337–345. [Google Scholar] [CrossRef]
- Sun, B.; Li, D.; Linghu, W.S.; Guan, X.H. Degradation of ciprofloxacin by manganese(III) intermediate: Insight into the potential application of permanganate/ bisulfite process. Chem. Eng. J. 2018, 339, 144–152. [Google Scholar] [CrossRef]
- Gonzalez, J.A.; Bafico, J.G.; Villanueva, M.E.; Giorgieri, S.A.; Copello, G.J. Continuous flow adsorption of ciprofloxacin by using a nanostructured chitin/graphene oxide hybrid material. Carbohyd. Polym. 2018, 188, 213–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamboli, V.; Mishra, G.P.; Mitra, A.K. Novel pentablock copolymer (PLA-PCL-PEG-PCL-PLA)-based nanoparticles for controlled drug delivery: Effect of copolymer compositions on the crystallinity of copolymers and in vitro drug release profile from nanoparticles. Colloid Polym. Sci. 2013, 291, 1235–1245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, X.Y.; Li, H.L.; He, Y.; Yuan, M.W.; Shen, M.L.; Yang, R.Y.; Jiang, N.F.; Yuan, M.L.; Yang, C. Preparation and in vitro release of total alkaloids from alstonia scholaris leaves loaded mPEG-PLA microspheres. Materials 2019, 12, 1457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Souza, A.J.M.; Schowen, R.L.; Topp, E.M. Polyvinylpyrrolidone-drug conjugate: Synthesis and release mechanism. J. Control. Release 2004, 94, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Fassihi, R. Application of a binary polymer system in drug release rate modulation. 1. characterization of release mechanism. J. Pharm. Sci. 1997, 86, 316–322. [Google Scholar] [CrossRef]
- Park, E.S.; Maniar, M.; Shah, J.C. Biodegradable polyanhydride devices of cefazolin sodium, bupivacaine, and taxol for local drug delivery: Preparation, and kinetics and mechanism of in vitro release. J. Control. Release 1998, 52, 179–189. [Google Scholar] [CrossRef]
- Chessa, S.; Huatan, H.; Levina, M.; Mehta, R.Y.; Ferrizzi, D.; Rajabi-Siahboomi, A.R. Application of the dynamic gastric model to evaluate the effect of food on the drug release characteristics of a hydrophilic matrix formulation. Int. J. Pharm. 2014, 466, 359–367. [Google Scholar] [CrossRef]
- Donbrow, M.; Friedman, M. Timed release from polymeric films containing drugs and kinetics of drug release. J. Pharm. Sci. 2010, 64, 76–80. [Google Scholar] [CrossRef]
- Lindstrom, F.T.; Ayres, J.W. Diffusion model for drug release from suspensions II: Release to a perfect sink. J. Pharm. Sci. 2010, 66, 662–668. [Google Scholar] [CrossRef]
- Vachon, M.G.; Nairn, J.G. Physico-chemical evaluation of acetylsalicylic acid-eudragit RS100 microspheres prepared using a solvent-partition method. J. Microencapsul. 1995, 12, 287–305. [Google Scholar] [CrossRef]
- Wei, W.; Shi, S.J.; Liu, J.; Sun, X.; Ren, K.; Zhao, D.; Zhang, X.N.; Zhang, Z.R.; Gong, T. Lipid nanoparticles loaded with 10- hydroxycamptothecin -phospholipid complex developed for the treatment of hepatoma in clinical application. J. Drug Target. 2010, 18, 557–566. [Google Scholar] [CrossRef] [PubMed]










| PCL/PGA | Original PLA Suture | 0/100 | 10/90 | 30/70 | 50/50 | 70/30 | 90/10 | 100/0 |
|---|---|---|---|---|---|---|---|---|
| Effective strength-time /weeks | 11.3 | 12.6 | 14.5 | 15.8 | 16.6 | 18.4 | 20.1 | 24.2 |
| PCL/ PGA | 100/0 | 90/10 | 30/70 | 50/50 | 30/70 | 10/90 | 0/100 | |
|---|---|---|---|---|---|---|---|---|
| Ritger−Peppas Equation: | K | 2.7829 | 3.3780 | 3.4313 | 4.1898 | 3.4539 | 3.1845 | 4.0301 |
| n | 0.4644 | 0.4587 | 0.4665 | 0.4765 | 0.4797 | 0.4718 | 0.4703 | |
| R2 | 0.9992 | 0.9993 | 0.9994 | 0.9994 | 0.9993 | 0.9996 | 0.9994 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, S.; Yu, J.; Li, H.; Wang, K.; Wu, G.; Wang, B.; Liu, M.; Zhang, Y.; Wang, P.; Zhang, J.; et al. Controllable Drug Release Behavior of Polylactic Acid (PLA) Surgical Suture Coating with Ciprofloxacin (CPFX)—Polycaprolactone (PCL)/Polyglycolide (PGA). Polymers 2020, 12, 288. https://doi.org/10.3390/polym12020288
Liu S, Yu J, Li H, Wang K, Wu G, Wang B, Liu M, Zhang Y, Wang P, Zhang J, et al. Controllable Drug Release Behavior of Polylactic Acid (PLA) Surgical Suture Coating with Ciprofloxacin (CPFX)—Polycaprolactone (PCL)/Polyglycolide (PGA). Polymers. 2020; 12(2):288. https://doi.org/10.3390/polym12020288
Chicago/Turabian StyleLiu, Shuqiang, Juanjuan Yu, Huimin Li, Kaiwen Wang, Gaihong Wu, Bowen Wang, Mingfang Liu, Yao Zhang, Peng Wang, Jie Zhang, and et al. 2020. "Controllable Drug Release Behavior of Polylactic Acid (PLA) Surgical Suture Coating with Ciprofloxacin (CPFX)—Polycaprolactone (PCL)/Polyglycolide (PGA)" Polymers 12, no. 2: 288. https://doi.org/10.3390/polym12020288