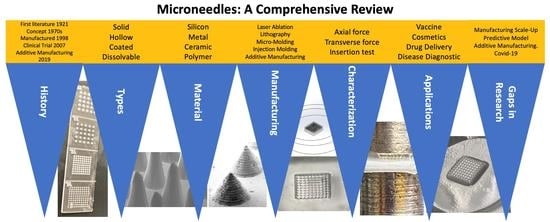
A Comprehensive Review of Microneedles: Types, Materials, Processes, Characterizations and Applications
Abstract
:1. Introduction
1.1. Drug Delivery System
1.2. Transdermal Drug Delivery (TDD)
1.3. Microneedle (MN) for Transdermal Drug Delivery
1.3.1. Economic Value and Statistics
1.3.2. Advantages
1.3.3. Disadvantages
2. Microneedle History
3. Microneedle Types
3.1. Solid Microneedle
3.2. Hollow Microneedle
3.3. Coated Microneedle
| MN Type | Characteristics | Advantages | Disadvantages | Application | Material | References |
|---|---|---|---|---|---|---|
| Solid | Creates channels in the skin to allow drugs reach the lower skin layer. Adequate mechanical strength. Sharper tip. | Allows more drugs to pass into the skin. Easy to manufacture. | Damage to the skin and microincisions need to be closed to avoid infections. | Drug delivery Cosmetic | Silicon Metal Polymer | [41,64,65,66,67] |
| Hollow | Empty shape to be filled with the drug. Ability to control drug release over time. | Handles a large dose/amount of drug solution. | Weak needles. Requires intensive care in terms of needle design and insertion method. Might cause leakage and clogging. | Disease diagnosis | Silicon | [16,59,68,69,70,71,72,73,74] |
| Coated | Carries less amount of the drug due to the design. Ability to deliver the proteins and DNA in a minimally invasive manner. | Deliver the drug quickly to the skin. | Prone to infection | Drug delivery Vaccine delivery | Silicon | [59,75,76,77,78] |
| Dissolving | Facilitates rapid release of macromolecules. | Ease of administration for patients with one step application. | Requires technical expertise to manufacture. Takes time to dissolve. | Drug delivery Cosmetic Vaccine delivery | Polymer | [16,59,69,80,81,82,83] |
3.4. Dissolving MN
4. MN Material
4.1. Silicon
4.2. Metal
4.3. Ceramic
4.4. Polymer
| MN Type | Advantages | Disadvantages | Manufacturing Method | MN Type Fit | References |
|---|---|---|---|---|---|
| Silicon | Flexible enough to manufacture desirable shapes and sizes. | Time-consuming fabrication. High cost. Possibility of skin fracture | Etching | Solid Hollow Coated | [29,53,55,100,110,111,112] |
| Metal | Good biocompatibility and mechanical properties. High fracture toughness Strong and hard to break. | High startup cost. Required post-fabrication process. May cause an allergic Reaction. | Laser ablation Etching Injection mold | Solid Hollow | [14,16,101,102,103,113,114,115] |
| Ceramic | Possesses chemical and compression resistance. | Low tension strength | Micromolding Lithography | Solid Hollow | [16,104,105,116,117] |
| Polymer | Excellent biocompatibility. Low toxicity. Low cost. | Low strength | Lithography injection molding Casting Laser ablation | Solid Hollow Coated Dissolving | [16,53,71,106,107,108,109,114,118,119] |
5. MN Manufacturing Method
5.1. Laser Ablation
5.2. Lithography
5.3. Micro-Molding
5.4. Injection Molding
5.5. Additive Manufacturing
6. MN Mechanical Characterizations
6.1. Axial Force
6.2. Transverse Force
6.3. Insertion Test
| Description | Importance | Limitation | References | |
|---|---|---|---|---|
| Axial Force | Apply force into the tip of the needle in vertical way (x-axis) | Determine the failure force of the tip needle. | Simulation (not accurate) | [80,157,176,177,178,179,180] |
| Transvers Force | Apply force into the MN base in parallel way (y-axis) | Determine the failure force of the needle base. | Simulation (not accurate) | [80,174,176,181] |
| Insertion Test | Apply the needles into a rat, pig, or human skin. | Determine the actual force on skin.Ability to release the drug. | Required a skin resource | [177,179,182,183,184,185,186,187] |
7. MN Applications
7.1. Drug Delivery
7.2. Vaccine Delivery
7.3. Disease Diagnosis
7.4. Cosmetic Application
8. Gaps in Research and Future Outlook
8.1. Manufacturing Process Scale-Up
8.2. Predictive Model for MN Manufacturing
8.3. Next Generation of MN
8.4. MN and Additive Manufacturing
8.5. Covid19 and MN
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ranade, V.V.; Hollinger, M.A.; Cannon, J.B. Drug Delivery Systems; CRC Press: Boca Raton, FL, USA, 2003. [Google Scholar]
- Tiwari, G.; Tiwari, R.; Bannerjee, S.; Bhati, L.; Pandey, S.; Pandey, P.; Sriwastawa, B. Drug delivery systems: An updated review. Int. J. Pharm. Investig. 2012, 2, 2–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassan, B.A.R. Overview on Drug Delivery System. Pharm. Anal. Acta 2012, 3, 4172. [Google Scholar]
- Robbie, G.; Wu, T.; Chiou, W.L. Poor and unusually prolonged oral absorption of amphotericin B in rats. Pharm. Res. 1999, 16, 455–458. [Google Scholar] [CrossRef] [PubMed]
- Date, A.A.; Nagarsenker, M. Parenteral microemulsions: An overview. Int. J. Pharm. 2008, 355, 19–30. [Google Scholar] [CrossRef]
- Rau, J.L. The inhalation of drugs: Advantages and problems. Respir. Care 2005, 50, 367–382. [Google Scholar]
- Zeng, X.M.; Martin, G.P.; Marriott, C. The controlled delivery of drugs to the lung. Int. J. Pharm. 1995, 124, 149–164. [Google Scholar] [CrossRef]
- El-Newehy, M.H.; El-Naggar, M.E.; Alotaiby, S.; El-Hamshary, H.; Moydeen, M.; Al-Deyab, S. Green Electrospining of Hydroxypropyl Cellulose Nanofibres for Drug Delivery Applications. J. Nanosci. Nanotechnol. 2018, 18, 805–814. [Google Scholar] [CrossRef]
- Om, H.; El-Naggar, M.E.; El-Banna, M.; Fouda, M.M.G.; Othman, S.I.; Allam, A.; Morsy, O.M. Combating atherosclerosis with targeted Diosmin nanoparticles-treated experimental diabetes. Investig. New Drugs 2020, 38, 1303–1315. [Google Scholar] [CrossRef]
- El-Naggar, M.E.; El-Rafie, M.; El-Sheikh, M.; El-Feky, G.S.; Hebeish, A. Synthesis, characterization, release kinetics and toxicity profile of drug-loaded starch nanoparticles. Int. J. Biol. Macromol. 2015, 81, 718–729. [Google Scholar] [CrossRef]
- El-Naggar, M.E.; Abdelgawad, A.; Salas, C.; Rojas, O. Curdlan in fibers as carriers of tetracycline hydrochloride: Controlled release and antibacterial activity. Carbohydr. Polym. 2016, 154, 194–203. [Google Scholar] [CrossRef] [PubMed]
- El-Newehy, M.H.; El-Naggar, M.E.; Alotaiby, S.; El-Hamshary, H.; Moydeen, M.; Al-Deyab, S. Preparation of biocompatible system based on electrospun CMC/PVA nanofibers as controlled release carrier of diclofenac sodium. J. Macromol. Sci. Part A 2016, 53, 566–573. [Google Scholar] [CrossRef]
- Alkilani, A.Z.; McCrudden, M.T.C.; Donnelly, R.F. Transdermal drug delivery: Innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics 2015, 7, 438–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donnelly, A.D.W.R.F.; Singh, T.R.R.; Morrow, D.I.J. Microneedle-Mediated Transdermal and Intradermal Drug Delivery; John Wiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar]
- Han, T.; Das, D.B. Potential of combined ultrasound and microneedles for enhanced transdermal drug permeation: A review. Eur. J. Pharm. Biopharm. 2015, 89, 312–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waghule, T.; Singhvi, G.; Dubey, S.K.; Pandey, M.M.; Gupta, G.; Singh, M.; Dua, K. Microneedles: A smart approach and increasing potential for transdermal drug delivery system. Biomed. Pharmacother. 2018, 109, 1249–1258. [Google Scholar] [CrossRef]
- Prausnitz, M.R.; Langer, R. Transdermal drug delivery. Natl. Inst. Health 2009, 26, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Song, C.; Baik, S.; Kim, D.; Hyeon, T.; Kim, D. Device-assisted transdermal drug delivery. Adv. Drug Deliv. Rev. 2017, 127, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, V.; Yadav, P. Transdermal drug delivery system: An overview. Asian J. Pharm. 2012, 6, 161–170. [Google Scholar] [CrossRef]
- Verma, N.K.; Panda, P.; Mishra, J.N.; Vishwakarma, D.K.; Singh, A.P.; Alam, G. Advances and development in transdermal drug delivery system—A Review. Int. J. Adv. Pharm. Int. J. Adv. Pharm. 2017, 6, 49–62. [Google Scholar]
- Goodman, M.P. Are all estrogens created equal? A review of oral vs. transdermal therapy. J. Women’s Health 2012, 21, 161–169. [Google Scholar] [CrossRef]
- Pandya, D.; Shinkar, D.; Saudagar, R. Revolutionized Topico-Systemic Era: Transdermal Drug Delivery System. Res. J. Top. Cosmet. Sci. 2015, 6, 66. [Google Scholar] [CrossRef]
- Mamta, Y.; Satish, N.; Jitendra, B. A Review on Transdermal Patches. Pharma Res. 2010, 3, 139–149. [Google Scholar]
- Erdő, F.; Hashimoto, N.; Karvaly, G.; Nakamichi, N.; Kato, Y. Critical evaluation and methodological positioning of the transdermal microdialysis technique. A review. J. Control. Release 2016, 233, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Gupta, H.; Babu, R. Transdermal Delivery: Product and Patent Update. Recent Pat. Drug Deliv. Formul. 2013, 7, 22. [Google Scholar] [CrossRef]
- Scheuplein, R.J.; Blank, I.H. Permeability of the skin. Physiol. Rev. 1971, 51, 702–747. [Google Scholar] [CrossRef]
- Seok, J.; Hong, J.Y.; Choi, S.Y.; Park, K.Y.; Kim, B.J. A potential relationship between skin hydration and stamp-type microneedle intradermal hyaluronic acid injection in middle-aged male face. J. Cosmet. Dermatol. 2016, 15, 578–582. [Google Scholar] [CrossRef]
- Singh, T.; Mcmillan, H.; Mooney, K.; Alkilani, A.; Donnelly, R. Microneedles for drug delivery and monitoring. Microfluid. Devices Biomed. Appl. 2013, 185–230. [Google Scholar] [CrossRef]
- Donnelly, R.F.; Singh, T.R.R.; Larrañeta, E.; McCrudde, M.T.C. Microneedles for Drug and Vaccine Delivery and Patient Monitoring; John Wiley and Sons, Incorporated: Hoboken, NJ, USA, 2018. [Google Scholar]
- Barry, B.W. Novel mechanisms and devices to enable successful transdermal drug delivery. Eur. J. Pharm. Sci. 2001, 14, 101–114. [Google Scholar] [CrossRef]
- Ghosh, P.; Brogden, N.K.; Stinchcomb, A.L. Effect of Formulation pH on Transport of Naltrexone Species and Pore Closure in Microneedle-Enhanced Transdermal Drug Delivery. Mol. Pharm. 2013, 10, 2331–2339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naik, A.; Kalia, Y.; Guy, R. Transdermal drug delivery: Overcoming the skin’s barrier function. Pharm. Sci. Technol. Today 2000, 3, 318–326. [Google Scholar] [CrossRef]
- Arora, A.; Prausnitz, M.R.; Mitragotri, S. Micro-scale devices for transdermal drug delivery. Int. J. Pharm. 2008, 364, 227–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tröls, A.; Hintermüller, M.; Saeedipour, M.; Pirker, S.; Jakoby, B. Drug dosage for microneedle-based transdermal drug delivery systems utilizing evaporation-induced droplet transport. Microfluid. Nanofluid. 2019, 23, 91. [Google Scholar] [CrossRef] [Green Version]
- Sun, W.; Lee, J.; Zhang, S.; Benyshek, C.; Dokmeci, M.R.; Khademhosseini, A. Engineering Precision Medicine. Adv. Sci. 2018, 6, 1801039. [Google Scholar] [CrossRef] [Green Version]
- Mahato, R. Chapter 13—Microneedles in Drug Delivery. In Micro and Nano Technologies; Elsevier: Boston, MA, USA, 2017; pp. 331–353. [Google Scholar]
- Lee, B.Y.; Bartsch, S.M.; Mvundura, M.; Jarrahian, C.; Zapf, K.M.; Marinan, K.; Wateska, A.R.; Snyder, B.; Swaminathan, S.; Jacoby, E.; et al. An economic model assessing the value of microneedle patch delivery of the seasonal influenza vaccine. Vaccine 2015, 33, 4727–4736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azmana, M.; Mahmood, S.; Hilles, A.R.; Mandal, U.K.; Al-Japairai, K.A.S.; Raman, S. Transdermal drug delivery system through polymeric microneedle: A recent update. J. Drug Deliv. Sci. Technol. 2020, 60, 101877. [Google Scholar] [CrossRef]
- Transdermal Drug Delivery Market Analysis & Trends—Technology, Application—Forecast to 2025; Research and Markets: Dublin, Irland, 2017.
- Microneedle Drug Delivery Systems Market. Available online: https://www.transparencymarketresearch.com/microneedle-drug-delivery-system-market.html (accessed on 1 August 2021).
- Kim, Y.C.; Park, J.H.; Prausnitz, M.R. Microneedles for drug and vaccine delivery. Drug Deliv. Transl. Res. 2015, 5, 311–312. [Google Scholar] [CrossRef] [Green Version]
- Amsden, B.G.; Goosen, M.F.A. Transdermal delivery of peptide and protein drugs: An overview. AIChE J. 1995, 41, 1972–1997. [Google Scholar] [CrossRef]
- Giudice, E.L.; Campbell, J.D. Needle-free vaccine delivery. Adv. Drug Deliv. Rev. 2006, 58, 68–89. [Google Scholar] [CrossRef]
- Museau, M.; Butdee, S.; Vignat, F. Design and Manufacturing of Microneedles Toward Sustainable Products Museau. King Mongkut’s Univ. Technol. North Bangk. Int. J. Appl. Sci. Technol. 2011, 4, 55–62. [Google Scholar]
- Williams, A.C.; Barry, B.W. Penetration enhancers. Adv. Drug Deliv. Rev. 2012, 64, 128–137. [Google Scholar] [CrossRef]
- Jeong, H.R.; Lee, H.S.; Choi, I.J.; Park, J.H. Considerations in the use of microneedles: Pain, convenience, anxiety and safety. J. Drug Target. 2017, 25, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Rzhevskiy, A.S.; Singh, T.R.R.; Donnelly, R.F.; Anissimov, Y.G. Microneedles as the technique of drug delivery enhancement in diverse organs and tissues. J. Control. Release 2018, 270, 184–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bariya, S.H.; Gohel, M.C.; Mehta, T.A.; Sharma, O.P. Microneedles: An emerging transdermal drug delivery system. J. Pharm. Pharmacol. 2011, 64, 11–29. [Google Scholar] [CrossRef] [PubMed]
- Ramadon, D.; McCrudden, M.T.C.; Courtenay, A.J.; Donnelly, R.F. Enhancement strategies for transdermal drug delivery systems: Current trends and applications. Drug Deliv. Transl. Res. 2021, 1–34. [Google Scholar] [CrossRef]
- Kawahara, K.; Tojo, K. Skin Irritation in Transdermal Drug Delivery Systems: A Strategy for its Reduction. Pharm. Res. 2006, 24, 399–408. [Google Scholar] [CrossRef]
- Walsh, L. Microneedling: A versatile and popular treatment option. J. Aesthetic Nurs. 2019, 8, 280–284. [Google Scholar] [CrossRef]
- Chambers, R. Microdissection studies, III. some problems in the maturation and fertilization of the echinoderm egg. Biol. Bull. 1921, 41, 318–350. [Google Scholar] [CrossRef] [Green Version]
- Larraneta, E.; Lutton, R.E.M.; Woolfson, A.D.; Donnelly, R.F. Microneedle Arrays As Transdermal and Intradermal Drug Delivery Systems: Materials Science, Manufacture and Commercial Development; Elsevier: Amsterdam, The Netherlands, 2016; Volume 104, pp. 1–32. [Google Scholar]
- Gerstel, M.S.; Place, V.A. Drug Delivery Device. U.S. Patent US3964482A, 22 June 1976. [Google Scholar]
- Reed, M.; Lye, W.-K. Microsystems for Drug and Gene Delivery. Proc. IEEE 2004, 92, 56–75. [Google Scholar] [CrossRef]
- Orentreich, D.S.; Orentreich, N. Subcutaneous Incisionless (Subcision) Surgery for the Correction of Depressed Scars and Wrinkles. Dermatol. Surg. 1995, 21, 543–549. [Google Scholar] [CrossRef]
- Henry, S.; McAllister, D.V.; Allen, M.G.; Prausnitz, M.R. Microfabricated Microneedles: A Novel Approach to Transdermal Drug Delivery. J. Pharm. Sci. 1998, 87, 922–925. [Google Scholar] [CrossRef]
- Prausnitz, M.R. Microneedles for transdermal drug delivery. Adv. Drug Deliv. Rev. 2004, 56, 581–587. [Google Scholar] [CrossRef]
- Dang, N.; Liu, T.Y.; Prow, T.W. Nano-and Microtechnology in Skin Delivery of Vaccines. In Micro and Nanotechnology in Vaccine Development; William Andrew Publishing: Norwich, NY, USA, 2017. [Google Scholar]
- Johnson, A.R.; Procopio, A.T. Low cost additive manufacturing of microneedle masters. 3D Print. Med. 2019, 5, 2. [Google Scholar] [CrossRef]
- Chen, Z.; Lin, Y.; Lee, W.; Ren, L.; Liu, B.; Liang, L.; Wang, Z.; Jiang, L. Additive Manufacturing of Honeybee-Inspired Microneedle for Easy Skin Insertion and Difficult Removal. ACS Appl. Mater. Interfaces 2018, 10, 29338–29346. [Google Scholar] [CrossRef]
- Caudill, C.L.; Perry, J.L.; Tian, S.; Luft, J.C.; DeSimone, J.M. Spatially controlled coating of continuous liquid interface production microneedles for transdermal protein delivery. J. Control. Release 2018, 284, 122–132. [Google Scholar] [CrossRef]
- Krieger, K.J.; Bertollo, N.; Dangol, M.; Sheridan, J.T.; Lowery, M.M.; O’Cearbhaill, E.D. Simple and customizable method for fabrication of high-aspect ratio microneedle molds using low-cost 3D printing. Microsyst. Nanoeng. 2019, 5, 42. [Google Scholar] [CrossRef] [Green Version]
- Moo-Young, M. Comprehensive Biotechnology; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Gupta, J.; Gill, H.S.; Andrews, S.N.; Prausnitz, M.R. Kinetics of skin resealing after insertion of microneedles in human subjects. J. Control. Release 2011, 154, 148–155. [Google Scholar] [CrossRef] [Green Version]
- Jacoby, E.; Jarrahian, C.; Hull, H.F.; Zehrung, D. Opportunities and Challenges in Deliveringinfluenza Vaccineby Microneedle Patch; Elsevier: Amsterdam, The Netherlands, 2015; p. 20892. [Google Scholar]
- Nair, K.J. Micro-Injection Moulded Microneedles for Drug Delivery; University of Bradford: Bradford, UK, 2014. [Google Scholar]
- Cheung, K.; Das, D.B. Microneedles for drug delivery: Trends and progress. Drug Deliv. 2014, 23, 2338–2354. [Google Scholar] [CrossRef] [Green Version]
- Ita, K. Transdermal Delivery of Drugs with Microneedles—Potential and Challenges. Pharmaceutics 2015, 7, 90–105. [Google Scholar] [CrossRef] [Green Version]
- Sanjay, S.T.; Dou, M.; Fu, G.; Xu, F.; Li, X. Controlled Drug Delivery Using Microdevices Sharma. Curr. Pharm. Biotechnol. 2017, 25, 1032–1057. [Google Scholar]
- Donnelly, R.F.; Morrow, D.I.J.; McCrudden, M.T.C.; Alkilani, A.Z.; Vicente-Pérez, E.M.; O'Mahony, C.; González-Vázquez, P.; McCarron, P.; Woolfson, A.D. Hydrogel-Forming and Dissolving Microneedles for Enhanced Delivery of Photosensitizers and Precursors. Photochem. Photobiol. 2014, 90, 641–647. [Google Scholar] [CrossRef] [Green Version]
- Mishra, R.; Bhattacharyya, T. MEMS-based hollow microneedles for transdermal drug delivery. Drug Deliv. Devices Ther. Syst. 2020, 325–344. [Google Scholar] [CrossRef]
- Zhang, P.; Dalton, C.; Jullien, G.A. Design and fabrication of MEMS-based microneedle arrays for medical applications. Microsyst. Technol. 2009, 15, 1073–1082. [Google Scholar] [CrossRef] [Green Version]
- McAllister, D.V.; Wang, P.M.; Davis, S.P.; Park, J.-H.; Canatella, P.J.; Allen, M.G.; Prausnitz, M.R. Microfabricated needles for transdermal delivery of macromolecules and nanoparticles: Fabrication methods and transport studies. Proc. Natl. Acad. Sci. USA 2003, 100, 13755–13760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; Zeng, M.; Shan, H.; Tong, C. Microneedle Patches as Drug and Vaccine Delivery Platform. Curr. Med. Chem. 2017, 24, 2413–2422. [Google Scholar] [CrossRef] [PubMed]
- Gill, H.S.; Prausnitz, M.R. Coated microneedles for transdermal delivery. J. Control. Release 2007, 117, 227–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duong, H.T.T.; Kim, N.W.; Thambi, T.; Phan, V.G.; Lee, M.S.; Yin, Y.; Jeong, J.H.; Lee, D.S. Microneedle arrays coated with charge reversal pH-sensitive copolymers improve antigen presenting cells-homing DNA vaccine delivery and immune responses. J. Control. Release 2018, 269, 225–234. [Google Scholar] [CrossRef]
- Kwon, K.M.; Lim, S.-M.; Choi, S.; Kim, D.-H.; Jin, H.-E.; Jee, G.; Hong, K.-J.; Kim, J.Y. Microneedles: Quick and easy delivery methods of vaccines. Clin. Exp. Vaccine Res. 2017, 6, 156–159. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Chen, B.Z.; Wang, Q.L.; Jin, X.; Guo, X.D. Fabrication of coated polymer microneedles for transdermal drug delivery. J. Control. Release 2017, 265, 14–21. [Google Scholar] [CrossRef]
- Demir, Y.K.; Akan, Z.; Kerimoglu, O. Characterization of Polymeric Microneedle Arrays for Transdermal Drug Delivery. PLoS ONE 2013, 8, e77289. [Google Scholar] [CrossRef] [Green Version]
- Rodgers, A.M.; Cordeiro, A.S.; Donnelly, R.F. Technology update: Dissolvable microneedle patches for vaccine delivery. Med. Devices 2019, 12, 379–398. [Google Scholar] [CrossRef] [Green Version]
- Guillot, A.J.; Cordeiro, A.S.; Donnelly, R.F.; Montesinos, M.C.; Garrigues, T.M.; Melero, A. Microneedle-Based Delivery: An Overview of Current Applications and Trends. Pharmaceutics 2020, 12, 569. [Google Scholar] [CrossRef]
- González-Vázquez, P.; Larrañeta, E.; McCrudden, M.T.; Jarrahian, C.; Rein-Weston, A.; Quintanar-Solares, M.; Zehrung, D.; McCarthy, H.; Courtenay, A.J.; Donnelly, R.F. Transdermal delivery of gentamicin using dissolving microneedle arrays for potential treatment of neonatal sepsis. J. Control. Release 2017, 265, 30–40. [Google Scholar] [CrossRef] [Green Version]
- Zhao, X.; Li, X.; Zhang, P.; Du, J.; Wang, Y. Tip-loaded fast-dissolving microneedle patches for photodynamic therapy of subcutaneous tumor. J. Control. Release 2018, 286, 201–209. [Google Scholar] [CrossRef]
- Desai, S.; Bidanda, B.; Bártolo, P.J. Emerging Trends in the Applications of Metallic and Ceramic Biomaterials. In Bio-Materials and Prototyping Applications in Medicine; Bártolo, P.J., Bidanda, B., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 1–17. [Google Scholar]
- Desai, S.; Shankar, M.R. Emerging Trends in Polymers, Composites, and Nano Biomaterial Applications. In Bio-Materials and Prototyping Applications in Medicine; Springer International Publishing: Cham, Switzerland, 2021; pp. 19–34. [Google Scholar]
- Li, W.; Ruff, B.; Yin, J.; Venkatasubramanian, R.; Mast, D.; Sowani, A.; Krishnaswamy, A.; Shanov, V.; Alvarez, N.; Malik, R.; et al. Tiny Medicine. In Nanotube Superfiber Materials: Changing Engineering Design; Elsevier Inc.: Amsterdam, The Netherlands, 2013; pp. 713–747. [Google Scholar]
- Desai, S.; Shankar, M.R. Polymers, composites and nano biomaterials: Current and future developments. In Bio-Materials and Prototyping Applications in Medicine; Springer US: New York, NY, USA, 2008; pp. 15–26. [Google Scholar]
- Desai, S.; Bidanda, B.; Bártolo, P. Metallic and ceramic biomaterials: Current and future developments. In Bio-Materials and Prototyping Applications in Medicine; Springer US: New York, NY, USA, 2008; pp. 1–14. [Google Scholar]
- Perkins, J.; Desai, S.; Wagner, W.; Hong, Y. Biomanufacturing: Direct-writing of controlled release coatings for cardiovascular (Stents) applications. In IIE Annual Conference. Proceedings; Institute of Industrial Engineers-Publisher: Norcross, GA, USA, 2011; pp. 1–6. [Google Scholar]
- Marquetti, I.; Desai, S. Orientation effects on the nanoscale adsorption behavior of bone morphogenetic protein-2 on hydrophilic silicon dioxide. RSC Adv. 2019, 9, 906–916. [Google Scholar] [CrossRef] [Green Version]
- Desai, S.; Harrison, B. Direct-Writing of Biomedia for Drug Delivery and Tissue Regeneration. In Printed Biomaterials; Springer: New York, NY, USA, 2010; pp. 71–89. [Google Scholar]
- Perkins, J.; Xu, Z.; Smith, C.; Roy, A.; Kumta, P.N.; Waterman, J.; Conklin, D.; Desai, S. Direct Writing of Polymeric Coatings on Magnesium Alloy for Tracheal Stent Applications. Ann. Biomed. Eng. 2014, 43, 1158–1165. [Google Scholar] [CrossRef]
- Perkins, J.L.; Desai, S.; Harrison, B.; Sankar, J. Understanding Release Kinetics of Calcium Alginate Microcapsules Using Drop on Demand Inkjet Printing. In Proceedings of the ASME 2009 International Mechanical Engineering Congress and Exposition, Lake Buena Vista, FL, USA, 13–19 November 2009; Volume 14. [Google Scholar]
- Desai, S.; Sankar, J.; Moore, A.; Harrison, B. Biomanufacturing of microcapsules for drug delivery and tissue engineering applications. In Proceedings of the 2008 Industrial Engineering Research Conference, Vancouver, BC, Canada, 17–21 May 2008; pp. 507–513. [Google Scholar]
- Desai, S.; Moore, A.; Harrison, B.; Sankar, J. Understanding Microdroplet Formations for Biomedical Applications. In Proceedings of the ASME 2008 International Mechanical Engineering Congress and Exposition, Boston, MA, USA, 31 October–6 November 2008; Volume 15. [Google Scholar]
- Desai, S.; Richardson, A.; Lee, S.J. Bioprinting of FITC conjugated bovine serum albumin towards stem cell differentiation. In Proceedings of the 2010 Industrial Engineering Research Conference, Cancun, Mexico, 6−9 June 2010. [Google Scholar]
- Parupelli, S.k.; Aljohani, A.; Khanal, S.; Bhattarai, N.; Desai, S. Direct Jet Printing and Characterization of Calcium Alginate Microcapsules for Biomedical Applications. In Proceedings of the 2019 IISE Annual Conference, Orlando, FL, USA, 18–21 May 2019. [Google Scholar]
- Cahill, E.M.; O’Cearbhaill, E.D. Toward Biofunctional Microneedles for Stimulus Responsive Drug Delivery. Bioconjugate Chem. 2015, 26, 1289–1296. [Google Scholar] [CrossRef]
- Sharma, D. Microneedles: An Approach in Transdermal Drug Delivery: A Review. PharmaTutor 2018, 6, 7–15. [Google Scholar] [CrossRef] [Green Version]
- Badilescu, S.; Packirisamy, M. BioMEMS: Science and Engineering Perspectives; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- O’Mahony, C. Structural characterization and in-vivo reliability evaluation of silicon microneedles. Biomed. Microdevices 2014, 16, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Niinomi, M.; Nakai, M. Titanium-Based Biomaterials for Preventing Stress Shielding between Implant Devices and Bone. Int. J. Biomater. 2011, 2011, 836587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro-Riviere, N.A. Toxicology of the Skin; CRC Press: New York, NY, USA, 2010. [Google Scholar]
- Verbaan, F.; Bal, S.; Berg, D.-J.V.D.; Groenink, W.; Verpoorten, H.; Lüttge, R.; Bouwstra, J. Assembled microneedle arrays enhance the transport of compounds varying over a large range of molecular weight across human dermatomed skin. J. Control. Release 2007, 117, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Pignatello, R. Biomaterials: Applications for Nanomedicine; BoD–Books on Demand: Norderstedt, Germany, 2011. [Google Scholar]
- Indermun, S.; Luttge, R.; Choonara, Y.; Kumar, P.; du Toit, L.; Modi, G.; Pillay, V. Current advances in the fabrication of microneedles for transdermal delivery. J. Control. Release 2014, 185, 130–138. [Google Scholar] [CrossRef]
- Bystrova, S.; Luttge, R. Micromolding for ceramic microneedle arrays. Microelectron. Eng. 2011, 88, 1681–1684. [Google Scholar] [CrossRef]
- Jeggy, C. Micro-Injection Moulding: From Process to Modelling; Presses Univ. de Louvain: Louvain-la-Neuve, Belgium, 2004. [Google Scholar]
- Yuan, W.; Hong, X.; Wu, Z.; Chen, L.; Liu, Z.; Wu, F.; Wei, L.L. Dissolving and biodegradable microneedle technologies for transdermal sustained delivery of drug and vaccine. Drug Des. Dev. Ther. 2013, 7, 945–952. [Google Scholar] [CrossRef] [Green Version]
- Adarkwa, E.; Desai, S. Scalable Droplet Based Manufacturing Using In-Flight Laser Evaporation. J. Nanoeng. Nanomanuf. 2016, 6, 87–92. [Google Scholar] [CrossRef]
- Yang, M.; Xu, Z.; Desai, S.; Kumar, D.; Sankar, J. Fabrication of Micro Single Chamber Solid Oxide Fuel Cell Using Photolithography and Pulsed Laser Deposition. J. Fuel Cell Sci. Technol. 2015, 12, 021004. [Google Scholar] [CrossRef]
- Desai, S.; Esho, T.; Kaware, R. Experimental investigation of controlled microdroplet evaporation toward scalable micro/nanomanufacturing. IIE Trans. 2012, 44, 155–162. [Google Scholar] [CrossRef]
- Desai, S. Methods and Apparatus for Manufacturing Micro- and/or Nano-Scale Features. U.S. Patents US20130314472A1, 28 November 2013. [Google Scholar]
- Esho, T.; Desai, S. Laser based microdroplet evaporation towards scalable micro and nano manufacturing. In Proceedings of the 2012 Industrial and Systems Engineering Research Conference, Orlando, FL, USA, 19–23 May 2012; pp. 1750–1757. [Google Scholar]
- Parupelli, S.K.; Desai, S. Understanding Hybrid Additive Manufacturing of Functional Devices. Am. J. Eng. Appl. Sci. 2017, 10, 264–271. [Google Scholar] [CrossRef] [Green Version]
- McKenzie, J.; Desai, S. Investigating Sintering Mechanisms for Additive Manufacturing of Conductive Traces. Am. J. Eng. Appl. Sci. 2018, 11, 652–662. [Google Scholar] [CrossRef]
- Esho, T.; Desai, S.; Craps, M. Direct writing of enriched single walled carbon nanotubes towards thin film transistors (TFTs). In Proceedings of the 2011 Industrial Engineering Research Conference, Reno, NV, USA, 21–25 May 2011. [Google Scholar]
- Desai, S.; De, P.; Gomes, F. Design for Nano/Micro Manufacturing: A Holistic Approach Towards Achieving Manufacturing Excellence. J. Udyog Pragati 2015, 39, 18–25. [Google Scholar]
- Desai, S.; Craps, M.; Esho, T. Direct writing of nanomaterials for flexible thin-film transistors (fTFTs). Int. J. Adv. Manuf. Technol. 2012, 64, 537–543. [Google Scholar] [CrossRef]
- Ahmed, M.; El-Naggar, M.E.; Aldalbahi, A.; El-Newehy, M.H.; Menazea, A. Methylene blue degradation under visible light of metallic nanoparticles scattered into graphene oxide using laser ablation technique in aqueous solutions. J. Mol. Liq. 2020, 315, 113794. [Google Scholar] [CrossRef]
- Ismail, A.M.; El-Newehy, M.H.; El-Naggar, M.E.; Moydeen, A.M.; Menazea, A.A. Enhancement the Electrical Conductivity of the Synthesized Polyvinylidene Fluoride/Polyvinyl Chloride Composite Doped with Palladium Nanoparticles via Laser Ablation; Elsevier: Amsterdam, The Netherlands, 2020; Volume 9, pp. 11178–11188. [Google Scholar]
- Menazea, A.; El-Newehy, M.H.; Thamer, B.M.; El-Naggar, M.E. Preparation of antibacterial film-based biopolymer embedded with vanadium oxide nanoparticles using one-pot laser ablation. J. Mol. Struct. 2021, 1225, 129163. [Google Scholar] [CrossRef]
- Tu, K.T.; Chung, C.K. Fabrication of biodegradable polymer microneedle array via CO2 laser ablation. In Proceedings of the 10th IEEE International Conference on Nano/Micro Engineered and Molecular Systems, Xi’an, China, 7–11 April 2015; pp. 494–497. [Google Scholar]
- Nejad, H.R.; Sadeqi, A.; Kiaee, G.; Sonkusale, S. Low-cost and cleanroom-free fabrication of microneedles. Microsyst. Nanoeng. 2018, 4, 17073. [Google Scholar] [CrossRef]
- Aoyagi, S.; Izumi, H.; Isono, Y.; Fukuda, M.; Ogawa, H. Laser fabrication of high aspect ratio thin holes on biodegradable polymer and its application to a microneedle. Sensors Actuators A Phys. 2007, 139, 293–302. [Google Scholar] [CrossRef]
- Chen, Y.-T.; Ma, K.-J.; Tseng, A.A.; Chen, P.-H. Projection ablation of glass-based single and arrayed microstructures using excimer laser. Opt. Laser Technol. 2005, 37, 271–280. [Google Scholar] [CrossRef]
- Zheng, H.; Lam, Y.; Sundarraman, C.; Tran, D. Influence of substrate cooling on femtosecond laser machined hole depth and diameter. Appl. Phys. A 2007, 89, 559–563. [Google Scholar] [CrossRef]
- Lutton, R.; Larrañeta, E.; Kearney, M.-C.; Boyd, P.; Woolfson, A.; Donnelly, R.F. A novel scalable manufacturing process for the production of hydrogel-forming microneedle arrays. Int. J. Pharm. 2015, 494, 417–429. [Google Scholar] [CrossRef] [Green Version]
- Zaied, M.; Miraoui, I. Analysis of heat affected zone obtained by CO2 laser cutting of low carbon steel (S235). In AIP Conference Proceedings; American Institute of Physics: College Park, MD, USA, 2013. [Google Scholar]
- Sato, Y.; Tsukamoto, M.; Nariyama, T.; Nakai, K.; Matsuoka, F.; Takahashi, K.; Masuno, S.; Ohkubo, T.; Nakano, H. Analysis of laser ablation dynamics of CFRP in order to reduce heat affected zone. In Proceedings of the SPIE Photonics West, San Francisco, CA, USA, 1–6 February 2014; Volume 8967. [Google Scholar]
- Brookhaven National Laboratory. Femtosecond Laser Micromachining. In Ultrafast Nonlinear Optics; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Donnelly, R.F.; Raghu, T.; Singh, R.; Woolfson, D. Microneedle-based drug delivery systems: Microfabrication, drug delivery, and safety. Drug Deliv. 2010, 17, 187–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaikwad, A.; Desai, S. Understanding Material Deformation in Nanoimprint of Gold using Molecular Dynamics Simulations. Am. J. Eng. Appl. Sci. 2018, 11, 837–844. [Google Scholar] [CrossRef] [Green Version]
- Gaikwad, A.; Odujole, J.; Desai, S. Atomistic investigation of process parameter variations on material deformation behavior in nanoimprint lithography of gold. Precis. Eng. 2020, 64, 7–19. [Google Scholar] [CrossRef]
- Odujole, J.I.; Desai, S. Molecular dynamics investigation of material deformation behavior of PMMA in nanoimprint lithography. AIP Adv. 2020, 10, 095102. [Google Scholar] [CrossRef]
- Odujole, J.; Desai, S. Atomistic Investigation of Material Deformation Behavior of Polystyrene in Nanoimprint Lithography. Surfaces 2020, 3, 649–663. [Google Scholar] [CrossRef]
- Gaikwad, A.; Clarke, J. Molecular Dynamics Study of the Quenching Effect on Direct Nanoimprint of Gold. In Proceedings of the 2019 IISE Annual Conference; National Science Foundation: Alexandria, VA, USA, 2019. [Google Scholar]
- Odujole, J.; Desai, S. Molecular Dynamics Simulation of Poly Acrylic Acid as a Resist Material for Thermal Nanoimprint Lithography Processes. In Proceedings of the Industrial Engineers Research Conference 2020, New Orleans, LA, USA, 1 October 2020. [Google Scholar]
- Gaikwad, A.; Desai, S. Molecular Dynamics Investigation of the Deformation Mechanism of Gold with Variations in Mold Profiles during Nanoimprinting. Materials 2021, 14, 2548. [Google Scholar] [CrossRef]
- Madou, M.J. Fundamentals of Microfabrication: The Science of Miniaturization; CRC Press: Boca Raton, FL, USA, 2002. [Google Scholar]
- Khuen, H.W.; Lay, L.L.; Schaper, C. On control of resist film uniformity in the microlithography process. IFAC Proc. Vol. 2002, 35, 19–24. [Google Scholar] [CrossRef] [Green Version]
- Plummer, J.D.; Deal, M.D.; Griffin, P.B. Silicon VLSI Technology: Fundamentals, Practice and Modeling; Pearson Education: India, 2009. [Google Scholar]
- Tran, K.T.; Nguyen, T.D. Lithography-based methods to manufacture biomaterials at small scales. J. Sci. Adv. Mater. Devices 2017, 2, 1–14. [Google Scholar] [CrossRef]
- Lee, K.; Lee, H.C.; Lee, D.-S.; Jung, H. Drawing Lithography: Three-Dimensional Fabrication of an Ultrahigh-Aspect-Ratio Microneedle. Adv. Mater. 2010, 22, 483–486. [Google Scholar] [CrossRef]
- Griffiths, C.A. Micro Injection Moulding: Tooling and Process Factors; Cardiff University: Cardiff, UK, 2008. [Google Scholar]
- Kim, M.J.; Park, S.C.; Rizal, B.; Guanes, G.; Baek, S.-K.; Park, J.-H.; Betz, A.R.; Choi, S.-O. Fabrication of Circular Obelisk-Type Multilayer Microneedles Using Micro-Milling and Spray Deposition. Front. Bioeng. Biotechnol. 2018, 6, 54. [Google Scholar] [CrossRef] [Green Version]
- Armani, D.; Liu, C.; Alum, N. Re-configu le fluid circuits by PDMS Elastomer Micromachinig. In Proceedings of the IEEE International Conference on Micro Electro Mechanical Systems, Orlando, FL, USA, 21 January 1999; pp. 222–227. [Google Scholar]
- Park, J.-H.; Allen, M.G.; Prausnitz, M.R. Biodegradable polymer microneedles Fabrication, mechanics andtransdermal drug delivery. J. Control. Release 2005, 104, 51–66. [Google Scholar] [CrossRef]
- Lhernould, M.S.; Deleers, M.; Delchambre, A. Hollow polymer microneedles array resistance and insertion tests. Int. J. Pharm. 2015, 480, 152–157. [Google Scholar] [CrossRef]
- Sammoura, F.; Kang, J.; Heo, Y.-M.; Jung, T.; Lin, L. Polymeric microneedle fabrication using a microinjection molding technique. Microsyst. Technol. 2006, 13, 517–522. [Google Scholar] [CrossRef]
- Juster, H.; van der Aar, B.; de Brouwer, H. A review on microfabrication of thermoplastic polymer-based microneedle arrays. Polym. Eng. Sci. 2019, 59, 877–890. [Google Scholar] [CrossRef] [Green Version]
- Parupelli, S.K.; Desai, S. A Comprehensive Review of Additive Manufacturing (3D Printing): Processes, Applications and Future Potential. Am. J. Appl. Sci. 2019, 16, 244–272. [Google Scholar] [CrossRef]
- Aldawood, F.K.; Desai, S.; Chang, S. Additive Manufacturing of Compensator Devices for Radiation Therapy. In Proceedings of the 2012 IISE Annual Conference, Virtual Conference, 1–3 November 2020. [Google Scholar]
- Desai, S.; Bidanda, B. Reverse Engineering: A Review & Evaluation of Contact Based Systems. In Rapid Prototyping; Kluwer Academic Publishers: New York, NY, USA, 2006; pp. 107–131. [Google Scholar]
- Adarkwa, E.; Desai, S.; Ohodnicki, J.; Roy, A.; Lee, B.; Kumta, P.N. Amorphous calcium phosphate blended polymer coatings for biomedical implants. In Proceedings of the 2014 Industrial and Systems Engineering Research Conference, Montréal, QC, Canada, 31 May–3 June 2014; pp. 132–138. [Google Scholar]
- Adarkwa, E.; Kotoka, R.; Desai, S. 3D printing of polymeric Coatings on AZ31 Mg alloy Substrate for Corrosion Protection of biomedical implants. Med. Devices Sensors 2021. [Google Scholar] [CrossRef]
- Altubaishe, B.; Clarke, J.; McWilliams, C.; Desai, S. Comparative Analysis of Risk Management Strategies for Additive Manufacturing Supply Chains. Am. J. Appl. Sci. 2019, 16, 273–282. [Google Scholar] [CrossRef] [Green Version]
- Aldawood, F.K.; Chang, S.X.; Desai, S. Design and manufacture of a high precision personalized electron bolus device for radiation therapy. Med. Devices Sensors 2020, 3. [Google Scholar] [CrossRef]
- Haeberle, G.; Desai, S. Investigating Rapid Thermoform Tooling Via Additive Manufacturing (3d Printing). Am. J. Appl. Sci. 2019, 16, 238–243. [Google Scholar] [CrossRef]
- Mckenzie, J.; Parupelli, S.; Martin, D.; Desai, S. Additive Manufacturing of Multiphase Materials for Electronics. In Proceedings of the 2017 Industrial and Systems Engineering Conference, Pittsburgh, PA, USA, 20–23 May 2017. [Google Scholar]
- Desai, S.; Yang, M.; Xu, Z.; Sankar, J. Direct Write Manufacturing of Solid Oxide Fuel Cells for Green Energy. J. Environ. Res. Dev. 2014, 8, 477. [Google Scholar]
- Parupelli, S.K.; Desai, S. Hybrid additive manufacturing (3D printing) and characterization of functionally gradient materials via in situ laser curing. Int. J. Adv. Manuf. Technol. 2020, 110, 543–556. [Google Scholar] [CrossRef]
- Bidanda, B.; Desai, S. Strategic planning models for prototyping and product development centres. Int. J. Prod. Dev. 2004, 1, 133. [Google Scholar] [CrossRef]
- Pere, C.P.P.; Economidou, S.N.; Lall, G.; Ziraud, C.; Boateng, J.S.; Alexander, B.D.; Lamprou, D.; Douroumis, D. 3D printed microneedles for insulin skin delivery. Int. J. Pharm. 2018, 544, 425–432. [Google Scholar] [CrossRef] [Green Version]
- Khanna, P.; Silva, H.; Bhansali, S. Variation in microneedle geometry to increase shear strength. Procedia Eng. 2010, 5, 977–980. [Google Scholar] [CrossRef]
- Lutton, R.E.M.; Moore, J.; Larrañeta, E.; Ligett, S.; Woolfson, A.D.; Donnelly, R.F. Microneedle characterisation: The need for universal acceptance criteria and GMP specifications when moving towards commercialisation. Drug Deliv. Transl. Res. 2015, 5, 313–331. [Google Scholar] [CrossRef] [Green Version]
- Gittard, S.D.; Chen, B.; Xu, H.; Ovsianikov, A.; Chichkov, B.; Monteiro-Riviere, N.; Narayan, R.J. The effects of geometry on skin penetration and failure of polymer microneedles. J. Adhes. Sci. Technol. 2013, 27, 227–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donnelly, R.F.; Majithiya, R.; Singh, R.R.T.; Morrow, D.I.J.; Garland, M.J.; Demir, Y.K.; Migalska, K.; Ryan, E.; Gillen, D.; Scott, C.J.; et al. Design, Optimization and Characterisation of Polymeric Microneedle Arrays Prepared by a Novel Laser-Based Micromoulding Technique. Pharm. Res. 2011, 28, 41–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, S.P.; Landis, B.J.; Adams, Z.H.; Allen, M.G.; Prausnitz, M.R. Insertion of microneedles into skin: Measurement and prediction of insertion force and needle fracture force. J. Biomech. 2004, 37, 1155–1163. [Google Scholar] [CrossRef] [PubMed]
- Khanna, P.; Luongo, K.; Strom, J.A.; Bhansali, S. Axial and shear fracture strength evaluation of silicon microneedles. Microsyst. Technol. 2010, 16, 973–978. [Google Scholar] [CrossRef]
- Maelíosa, R.F.D.; McCrudden, T.C.; Alkilani, A.Z.; McCrudden, C.M.; McAlister, E.; McCarthy, H.O.; Woolfson, A.D. Design and physicochemical characterisation of novel dissolvingpolymeric microneedle arrays for transdermal delivery of high dose, low molecular weight drugs. J. Control. Release 2014, 180, 71–80. [Google Scholar]
- Park, J.-H.; Prausnitz, M.R. Analysis of mechanical failure of polymer microneedles by axial force. J. Korean Phys. Soc. 2010, 56, 1223–1227. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Yoon, Y.-K.; Choi, S.-O.; Prausnitz, M.R.; Allen, M.G. Tapered Conical Polymer Microneedles Fabricated Using an Integrated Lens Technique for Transdermal Drug Delivery. IEEE Trans. Biomed. Eng. 2007, 54, 903–913. [Google Scholar] [CrossRef]
- Lahiji, S.F.; Dangol, M.; Jung, H. A patchless dissolving microneedle delivery system enabling rapid and efficient transdermal drug delivery. Sci. Rep. 2015, 5, 7914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.; Yang, H.; Kim, S.; Lee, C.; Jung, H. The Troy Microneedle: A Rapidly Separating, Dissolving Microneedle Formed by Cyclic Contact and Drying on the Pillar (CCDP). PLoS ONE 2015, 10, e0136513. [Google Scholar] [CrossRef]
- Lee, J.W.; Park, J.H.; Prausnitz, M.R. Dissolving Microneedles for Transdermal Drug Delivery. Biomaterials 2008, 29, 2113–2124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jun, H.; Ahn, M.-H.; Choi, I.-J.; Baek, S.-K.; Park, J.-H.; Choi, S.-O. Immediate separation of microneedle tips from base array during skin insertion for instantaneous drug delivery. RSC Adv. 2018, 8, 17786–17796. [Google Scholar] [CrossRef] [Green Version]
- Khan, S.; Minhas, M.U.; Tekko, I.A.; Donnelly, R.; Thakur, R.R.S. Evaluation of microneedles-assisted in situ depot forming poloxamer gels for sustained transdermal drug delivery. Drug Deliv. Transl. Res. 2019, 9, 764–782. [Google Scholar] [CrossRef] [Green Version]
- Ripolin, A.; Quinn, J.; Larrañeta, E.; Vicente-Perez, E.M.; Barry, J.; Donnelly, R.F. Successful application of large microneedle patches by human volunteers. Int. J. Pharm. 2017, 521, 92–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.W.; Choi, S.-O.; Felner, E.I.; Prausnitz, M.R. Dissolving Microneedle Patch for Transdermal Delivery of Human Growth Hormone. Small 2011, 7, 531–539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dangol, M.; Kim, S.; Li, C.G.; Lahiji, S.F.; Jang, M.; Ma, Y.; Huh, I.; Jung, H. Anti-obesity effect of a novel caffeine-loaded dissolving microneedle patchin high-fat diet-induced obese C57BL:6J mice. J. Control. Release 2017, 265, 41–47. [Google Scholar] [CrossRef]
- Tas, C.; Mansoor, S.; Kalluri, H.; Zarnitsyn, V.G.; Choi, S.-O.; Banga, A.K.; Prausnitz, M.R. Delivery of salmon calcitonin using a microneedle patch. Int. J. Pharm. 2012, 423, 257–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matriano, J.A.; Cormier, M.; Johnson, J.; Young, W.A.; Buttery, M.; Nyam, K.; Daddona, P.E. Macroflux® Microprojection Array Patch Technology: A New and Efficient Approach for Intracutaneous Immunization. Pharm. Res. 2002, 19, 63–70. [Google Scholar] [CrossRef]
- Donnelly, R.F.; Morrow, D.I.J.; McCarron, P.; Woolfson, A.D.; Morrissey, A.; Juzenas, P.; Juzeniene, A.; Iani, V.; McCarthy, H.; Moan, J. Microneedle Arrays Permit Enhanced Intradermal Delivery of a Preformed Photosensitizer. Photochem. Photobiol. 2009, 85, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Stahl, J.; Wohlert, M.; Kietzmann, M. Microneedle pretreatment enhances the percutaneous permeation of hydrophilic compounds with high melting points. BMC Pharmacol. Toxicol. 2012, 13, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nayak, S.; Suryawanshi, S.; Bhaskar, V. Microneedle Technology for Transdermal Drug Delivery: Applications and Combination With Other Enhancing Techniques. J. Drug Deliv. Ther. 2016, 6, 65–83. [Google Scholar] [CrossRef]
- Stoeber, B.; Liepmann, D. Fluid injection through out-of-plane microneedles. In Proceedings of the 1st Annual International IEEE-EMBS Special Topic Conference on Microtechnologies in Medicine and Biology. Proceedings, Lyon, France, 12–14 October 2000; pp. 224–228. [Google Scholar]
- Chen, J.; Wise, K.D.; Hetke, J.F.; Bledsoe, S.C. A multichannel neural probe for selective chemical delivery at the cellular level. IEEE Trans. Biomed. Eng. 1997, 44, 760–769. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.; Sahm, L.J.; Moore, A. The success of microneedle-mediated vaccine delivery into skin. Hum. Vaccines Immunother. 2016, 12, 2975–2983. [Google Scholar] [CrossRef] [Green Version]
- Matsuo, K.; Hirobe, S.; Yokota, Y.; Ayabe, Y.; Seto, M.; Quan, Y.S.; Kamiyama, F.; Tougan, T.; Horii, T.; Mukai, Y.; et al. Transcutaneous immunization using a dissolving microneedle array protects against tetanus, diphtheria, malaria, and influenza. J. Control. Release 2012, 160, 495–501. [Google Scholar] [CrossRef]
- Yang, J.; Liu, X.; Fu, Y.; Song, Y. Recent advances of microneedles for biomedicalapplications- drug delivery and beyond.pdf. Acta Pharm. Sin. B 2019, 9, 469–483. [Google Scholar] [CrossRef]
- Poirier, D.; Renaud, F.; Dewar, V.; Strodiot, L.; Wauters, F.; Janimak, J.; Shimada, T.; Nomura, T.; Kabata, K.; Kuruma, K.; et al. Hepatitis B surface antigen incorporated in dissolvable microneedle array patch is antigenic and thermostable. Biomaterials 2017, 145, 256–265. [Google Scholar] [CrossRef]
- Pattani, A.; McKay, P.; Garland, M.J.; Curran, R.M.; Migalska, K.; Cassidy, C.M.; Malcolm, K.; Shattock, R.J.; McCarthy, H.; Donnelly, R.F. Microneedle mediated intradermal delivery of adjuvanted recombinant HIV-1 CN54gp140 effectively primes mucosal boost inoculations. J. Control. Release 2012, 162, 529–537. [Google Scholar] [CrossRef] [Green Version]
- Edens, C.; Dybdahl-Sissoko, N.C.; Weldon, W.C.; Oberste, M.S.; Prausnitz, M.R. Inactivated polio vaccination using a microneedle patch is immunogenic in the rhesus macaque. Vaccine 2015, 33, 4683–4690. [Google Scholar] [CrossRef] [Green Version]
- Hiraishi, Y.; Nandakumar, S.; Choi, S.-O.; Lee, J.W.; Kim, Y.-C.; Posey, J.E.; Sable, S.B.; Prausnitz, M.R. Bacillus Calmette-Guérin vaccination using a microneedle patch. Vaccine 2011, 29, 2626–2636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gill, H.S.; Söderholm, J.; Prausnitz, M.R.; Sällberg, M. Cutaneous vaccination using microneedles coated with hepatitis C DNA vaccine. Gene Ther. 2010, 17, 811–814. [Google Scholar] [CrossRef]
- Zhu, Q.; Zarnitsyn, V.G.; Ye, L.; Wen, Z.; Gao, Y.; Pan, L.; Skountzou, I.; Gill, H.S.; Prausnitz, M.R.; Yang, C.; et al. Immunization by vaccine-coated microneedle arrays protects against lethal influenza virus challenge. Proc. Natl. Acad. Sci. USA 2009, 106, 7968–79739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mikszta, J.A.; Dekker, J.P.; Harvey, N.G.; Dean, C.H.; Brittingham, J.M.; Huang, J.; Sullivan, V.J.; Dyas, B.; Roy, C.; Ulrich, R.G. Microneedle-Based Intradermal Delivery of the Anthrax Recombinant Protective Antigen Vaccine. Infect. Immun. 2006, 74, 6806–6810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, J.; D'Souza, A.J.; Alarcon, J.B.; Mikszta, J.A.; Ford, B.M.; Ferriter, M.S.; Evans, M.; Stewart, T.; Amemiya, K.; Ulrich, R.G.; et al. Protective Immunity in Mice Achieved with Dry Powder Formulation and Alternative Delivery of Plague F1-V Vaccine. Clin. Vaccine Immunol. 2009, 16, 719–725. [Google Scholar] [CrossRef] [Green Version]
- Van Damme, P.; Oosterhuis-Kafeja, F.; van der Wielen, M.; Almagor, Y.; Sharon, O.; Levin, Y. Safety and efficacy of a novel microneedle device for dose sparing intradermal influenza vaccination in healthy adults. Vaccine 2009, 27, 454–459. [Google Scholar] [CrossRef]
- Zhu, J.; Zhou, X.; Libanori, A.; Sun, W. Microneedle-based bioassays. Nanoscale Adv. 2020, 2, 4295–4304. [Google Scholar] [CrossRef]
- Chang, H.; Zheng, M.; Yu, X.; Than, A.; Seeni, R.Z.; Kang, R.; Tian, J.; Khanh, D.P.; Liu, L.; Chen, P.; et al. A Swellable Microneedle Patch to Rapidly Extract Skin Interstitial Fluid for Timely Metabolic Analysis. Adv. Mater. 2017, 29, 1–8. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Han, M.-R.; Kim, Y.-H.; Shin, S.-W.; Nam, S.-Y.; Park, J.-H. Tip-loaded dissolving microneedles for transdermal delivery of donepezil hydrochloride for treatment of Alzheimer’s disease. Eur. J. Pharm. Biopharm. 2016, 105, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.M.; Cornwell, M.; Prausnitz, M.R. Minimally Invasive Extraction of Dermal Interstitial Fluid for Glucose Monitoring Using Microneedles. Diabetes Technol. Ther. 2005, 7, 131–141. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, C.; Pini, F.; Vereschagina, L.; Blake, A.; O’Brien, J.; Webster, C.; Galvin, P.; McCarthy, K.G. Skin insertion mechanisms of microneedle-based dry electrodes for physiological signal monitoring. In Proceedings of the 2013 IEEE Biomedical Circuits and Systems Conference (BioCAS), Rotterdam, The Netherlands, 31 October–2 November 2013; pp. 69–72. [Google Scholar]
- Mohan, A.V.; Windmiller, J.R.; Mishra, R.K.; Wang, J. Continuous minimally-invasive alcohol monitoring using microneedle sensor arrays. Biosens. Bioelectron. 2017, 91, 574–579. [Google Scholar] [CrossRef] [Green Version]
- Sharma, S.; Hatware, K.; Bhadane, P.; Sindhikar, S.; Mishra, D.K. Recent advances in microneedle composites for biomedical applications: Advanced drug delivery technologies. Mater. Sci. Eng. C 2019, 103, 109717. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.-H.; Ha, S.K.; Choi, I.; Kim, K.S.; Park, J.; Choi, N.; Kim, B.; Sung, J.H. Fabrication of degradable carboxymethyl cellulose (CMC) microneedle with laser writing and replica molding process for enhancement of transdermal drug delivery. Biotechnol. Bioprocess Eng. 2016, 21, 110–118. [Google Scholar] [CrossRef]
- Kumar, A.; Naguib, Y.; Shi, Y.-C.; Cui, Z. A method to improve the efficacy of topical eflornithine hydrochloride cream. Drug Deliv. 2016, 23, 1495–1501. [Google Scholar] [CrossRef] [PubMed]
- Mysore, V.; Chandrashekar, B.; Yepuri, V. Alopecia areata-successful outcome with microneedling and triamcinolone acetonide. J. Cutan. Aesthetic Surg. 2014, 7, 63–64. [Google Scholar] [CrossRef] [PubMed]
- Majid, I. Microneedling therapy in atrophic facial scars: An objective assessment. J. Cutan. Aesthetic Surg. 2009, 2, 26–30. [Google Scholar] [CrossRef]
- El-Domyati, M.; Barakat, M.; Awad, S.; Medhat, W.; El-Fakahany, H.; Farag, H. Microneedling therapy for atrophic acne scars an objective evaluation. J. Clin. Aesthet. Dermatol. 2015, 8, 36–42. [Google Scholar] [PubMed]
- Aust, M.C.; Knobloch, K.; Reimers, K.; Redeker, J.; Ipaktchi, R.; Altintas, M.A.; Gohritz, A.; Schwaiger, N.; Vogt, P.M. Percutaneous collagen induction therapy: An alternative treatment for burn scars. Burns 2010, 36, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Dhurat, R.; Sukesh, M.; Avhad, G.; Dandale, A.; Pal, A.; Pund, P. A randomized evaluator blinded study of effect of microneedling in androgenetic alopecia: A pilot study. Int. J. Trichol. 2013, 5, 6–11. [Google Scholar] [CrossRef] [Green Version]
- Economidou, S.N.; Douroumis, D. 3D printing as a transformative tool for microneedle systems: Recent advances, manufacturing considerations and market potential. Adv. Drug Deliv. Rev. 2021, 173, 60–69. [Google Scholar] [CrossRef]
- Bhatnagar, S.; Gadeela, P.R.; Thathireddy, P.; Venuganti, V.V.K. Microneedle-based drug delivery: Materials of construction. J. Chem. Sci. 2019, 131, 90. [Google Scholar] [CrossRef] [Green Version]
- Tu, K.T.; Chung, C.K. Rapid prototyping of biodegradable microneedle arrays by integrating CO2laser processing and polymer molding. J. Micromech. Microeng. 2016, 26, 65015. [Google Scholar] [CrossRef]
- Akter, T.; Desai, S. Developing a predictive model for nanoimprint lithography using artificial neural networks. Mater. Des. 2018, 160, 836–848. [Google Scholar] [CrossRef]
- Elhoone, H.; Zhang, T.; Anwar, M.; Desai, S. Cyber-based design for additive manufacturing using artificial neural networks for Industry 4.0. Int. J. Prod. Res. 2019, 58, 2841–2861. [Google Scholar] [CrossRef]
- Almakaeel, H.; Albalawi, A.; Desai, S. Artificial neural network based framework for cyber nano manufacturing. Manuf. Lett. 2018, 15, 151–154. [Google Scholar] [CrossRef]
- Desai, S.; Dean, C.; Desai, Y. Cyber-enabled concurrent material and process selection in a flexible design for manufacture paradigm. Int. J. Adv. Manuf. Technol. 2018, 97, 1719–1731. [Google Scholar] [CrossRef]
- Desai, S.; Bidanda, B.; Lovell, M.R. Material and process selection in product design using decision-making technique (AHP). Eur. J. Ind. Eng. 2012, 6, 322–346. [Google Scholar] [CrossRef]
- Desai, S.; Dean, C. Concurrent material and process selection in a flexible design for manufacture paradigm. In Proceedings of the 2007 Industrial Engineering Research Conference, Nashville, TN, USA, 19–23 May 2007; p. 764. [Google Scholar]
- Cordeiro, J.; Desai, S. Process Parameter Studies of Molecular Dynamics Models to Control Substrate Wettability. In Proceedings of the ASME 2015 International Manufacturing Science and Engineering Conference, Charlotte, NC, USA, 8–12 June 2015. [Google Scholar]
- Aljohani, A.; Desai, S. 3D Printing of Porous Scaffolds for Medical Applications. Am. J. Eng. Appl. Sci. 2018, 11, 1076–1085. [Google Scholar] [CrossRef]
- Cordeiro, J.; Desai, S. Exploring Nano Scale Design Space with Molecular Dynamics Simulations. In Proceedings of the 2015 Industrial and Systems Engineering Research Conference, Nashville, TN, USA, 30 May–2 June 2015; pp. 856–861. [Google Scholar]
- Cordeiro, J.; Desai, S. The Leidenfrost Effect at the Nanoscale. J. Micro Nano Manuf. 2016, 4, 041001. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, J.; Desai, S. The Effect of Water Droplet Size, Temperature and Impingement Velocity on Gold Wettability at the Nanoscale. J. Micro Nano Manuf. 2017, 5, 031008. [Google Scholar]
- Marquetti, I.; Rodrigues, J.; Desai, S.S. Ecological Impact of Green Computing Using Graphical Processing Units in Molecular Dynamics Simulations. Int. J. Green Comput. 2018, 9, 35–48. [Google Scholar] [CrossRef]
- Marquetti, I.; Desai, S. Molecular modeling the adsorption behavior of bone morphogenetic protein-2 on hydrophobic and hydrophilic substrates. Chem. Phys. Lett. 2018, 706, 285–294. [Google Scholar] [CrossRef]
- Marquetti, I.; Desai, S. Adsorption Behavior of Bone Morphogenetic Protein-2 on a Graphite Substrate for Biomedical Applications. Am. J. Eng. Appl. Sci. 2018, 11, 1037–1044. [Google Scholar] [CrossRef] [Green Version]
- Desai, S.; Perkins, J.; Harrison, B.S.; Sankar, J. Understanding release kinetics of biopolymer drug delivery microcapsules for biomedical applications. Mater. Sci. Eng. B Solid-State Mater. Adv. Technol. 2010, 168, 127–131. [Google Scholar] [CrossRef]
- Li, Q.Y.; Zhang, J.N.; Chen, B.Z.; Wang, Q.L.; Guo, X.D. A solid polymer microneedle patch pretreatment enhances the permeation of drug molecules into the skin. RSC Adv. 2017, 7, 15408–15415. [Google Scholar] [CrossRef] [Green Version]
- Al-Japairai, K.A.S.; Mahmood, S.; Almurisi, S.H.; Venugopal, J.R.; Hilles, A.R.; Azmana, M.; Raman, S. Current trends in polymer microneedle for transdermal drug delivery. Int. J. Pharm. 2020, 587, 119673. [Google Scholar] [CrossRef]
- Ogunsanya, M.; Isichei, J.; Parupelli, S.K.; Desai, S.; Cai, Y. In-situ Droplet Monitoring of Inkjet 3D Printing Process using Image Analysis and Machine Learning Models. Procedia Manuf. 2021, 53, 427–434. [Google Scholar] [CrossRef]
- Tofail, S.A.M.; Koumoulos, E.P.; Bandyopadhyay, A.; Bose, S.; O’Donoghue, L.; Charitidis, C. Additive manufacturing: Scientific and technological challenges, market uptake and opportunities. Mater. Today 2018, 21, 22–37. [Google Scholar] [CrossRef]
- Desai, S.; Lovell, M. CFD analysis of a continuous inkjet print head for direct write fabrication. In Proceedings of the ASME 2007 International Mechanical Engineering Congress and Exposition, Seattle, WA, USA, 11–15 November 2007; Volume 13. pp. 209–213. [Google Scholar]
- Desai, S.; Desai, S.; Lovell, M. Statistical Optimization of Process Variables in A Continuous Inkjet Process—A Case Study. Int. J. Ind. Eng. Theory Appl. Pract. 2008, 15, 104–112. [Google Scholar]
- Desai, S.; Lovell, M. Computational fluid dynamics analysis of a direct write manufacturing process. Int. J. Nanomanuf. 2009, 3, 171. [Google Scholar] [CrossRef]
- Desai, S.; Lovell, M. Modeling fluid–structure interaction in a direct write manufacturing process. J. Mater. Process. Technol. 2012, 212, 2031–2040. [Google Scholar] [CrossRef]
- Desai, S.; Lovell, M. Multiphysics modeling of A piezoelectric Bimorph disc in A Direct Write Fabrication Process. In Proceedings of the ASME 2005 International Mechanical Engineering Congress and Exposition, Orlando, FL, USA, 5–11 November 2005; Volume 100, pp. 437–442. [Google Scholar]
- Desai, S.; Lovell, M.; Cordle, J. Coupled field analysis of a piezoelectric bimorph disc in a direct write process. Compos. Part B Eng. 2007, 38, 824–832. [Google Scholar] [CrossRef]
- Chappell, C.; Desai, S.; Sankar, J. Computational Modeling of a Drop-on-Demand (DOD) Inkjet System for Understanding Microdroplet Behavior. ASME Early Career Tech. J. 2008, 6, 350–359. [Google Scholar]
- Rodrigues, J.; Desai, S. The nanoscale Leidenfrost effect. Nanoscale 2019, 11, 12139–12151. [Google Scholar] [CrossRef]
- Marquetti, I.; Desai, S. Molecular Modeling of Bone Morphogenetic Protein for Tissue Engineering Applications. In Proceedings of the 2018 IISE Annual Conference, Orlando, FL, USA, 19–22 May 2018. [Google Scholar]
- Chen, W.; Cai, B.; Geng, Z.; Chen, F.; Wang, Z.; Wang, L.; Chen, X. Reducing False Negatives in COVID-19 Testing by Using Microneedle-Based Oropharyngeal Swabs. Matter 2020, 3, 1589–1600. [Google Scholar] [CrossRef] [PubMed]



















| Manufacturing Method | Description | Advantages | Disadvantages | References |
|---|---|---|---|---|
| Laser Ablation | Uses a focused optical light beam to fabricate a MN array on a substrate. | Less time consuming. | Might cause a crack or fatigue resistance on the substrate (MN array). High cost. Not suitable for large production. | [109,118,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140] |
| Lithography | Transfers the master pattern of the geometric shapes onto the surface of a substrate. | Produces MN from a variety of material. Very precise geometries Smooth vertical sidewall. | Time consuming. | [53,118,134,141,142,143,144,145,146,147,148,149,150,151,152,153] |
| Micro-molding | Replicates a master mold and casts the mold with a solution. | Used for mass production. Cost effective. | Controls the depth of penetration. Drug load capacity. Mechanical behavior. | [14,154,155,156,157] |
| Injection molding | Injecting molten plastic materials into a mold. | Mass production. | High initial cost (machine equipment cost). Complex processes. | [67,80,107,158,159] |
| Additive manufacturing | Printing the MNs layer by layer. | Customizable Design. | Requires a high-quality 3D printer. Offer limited accuracy. | [60,63,160,161,162,163,164,165,166,167,168,169,170,171,172] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aldawood, F.K.; Andar, A.; Desai, S. A Comprehensive Review of Microneedles: Types, Materials, Processes, Characterizations and Applications. Polymers 2021, 13, 2815. https://doi.org/10.3390/polym13162815
Aldawood FK, Andar A, Desai S. A Comprehensive Review of Microneedles: Types, Materials, Processes, Characterizations and Applications. Polymers. 2021; 13(16):2815. https://doi.org/10.3390/polym13162815
Chicago/Turabian StyleAldawood, Faisal Khaled, Abhay Andar, and Salil Desai. 2021. "A Comprehensive Review of Microneedles: Types, Materials, Processes, Characterizations and Applications" Polymers 13, no. 16: 2815. https://doi.org/10.3390/polym13162815