Abstract
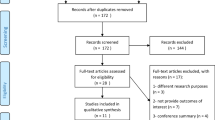
Herniation of nucleus pulposus leading to leg pain is the commonest indication for lumbar spine surgery. However, there is no consensus when to stop conservative treatment and when to consider for surgery. A systematic review of literature was done to find a consensus on the issue of when should surgery be performed for herniation of nucleus pulposus in lumbar spine was conducted. Electronic database searches of Medline, Embase and Pubmed Central were performed to find articles relating to optimum time to operate in patients with herniation of nucleus pulposus in lumbar spine, published between January 1975 and 10 December 2012. The studies were independently screened by two reviewers. Disagreements between reviewers were settled at a consensus meeting. A scoring system based on research design, number of patients at final followup, percentage of patients at final followup, duration of followup, journal impact factor and annual citation index was devised to give weightage to Categorize (A, B or C) each of the articles. Twenty one studies fulfilled the criteria. Six studies were of retrospective design, 13 studies were of Prospective design and two studies were randomized controlled trials. The studies were categorized as: Two articles in category A (highest level of evidence), 12 articles in category B (moderate level of evidence) while seven articles in Category C (poor level of evidence). Category A studies conclude that duration of sciatica prior to surgery made no difference to the outcome of surgery in patients with herniation of nucleus pulposus in the lumbar spine. Ten out of 12 studies in Category B revealed that longer duration of sciatica before surgery leads to poor results while 2 studies conclude that duration of sciatica makes no difference to outcome. In category C, five studies conclude that longer duration of sciatica before surgery leads to poor outcome while two studies find no difference in outcome with regards to duration of sciatica. A qualitative and quantitative analysis was performed which favoured the consensus that longer duration of sciatica leads to poorer outcome. A systematic and critical review of literature revealed that long duration of preoperative leg pain lead to poor outcome for herniation of nucleus pulposus. Only a broad time frame (2–12 months) could be derived from the review of literature due to lack of high quality studies and variable and contrasting results of the existing studies. While surgery performed within six months was most commonly found to lead to good outcome of surgery, further studies are needed to prove this more conclusively. At this stage it is felt that time alone should not be the basis of recommending surgery and multiple other variables should be considered in a shared decision making process between the surgeon and the patient.
Similar content being viewed by others
References
Frymoyer JW. Back pain and sciatica. N Engl J Med 1988;318:291–300.
Frymoyer JW. Lumbar disk disease: Epidemiology. Instr Course Lect 1992;41:217–23.
Stafford MA, Peng P, Hill DA. Sciatica: A review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth 2007;99:461–73.
Weber H, Holme I, Amlie E. The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of piroxicam. Spine (Phila Pa 1976) 1993;18:1433–8.
Saal JA, Saal JS. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. An outcome study. Spine (Phila Pa 1976) 1989;14:431–7.
Hasue M, Fujiwara M. Epidemiologic and clinical studies of long term prognosis of low-back pain and sciatica. Spine (Phila Pa 1976) 1979;4:150–5.
Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine (Phila Pa 1976) 1994;19:1201–6.
Weinstein J. Dartmouth Atlas of Musculoskeletal Health Care. Chicago IL: American Hospital Association Press; 2000.
Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K. The natural history of herniated nucleus pulposus with radiculopathy. Spine (Phila Pa 1976) 1996;21:225–9.
Splendiani A, Puglielli E, De Amicis R, Barile A, Masciocchi C, Gallucci M. Spontaneous resolution of lumbar disk herniation: Predictive signs for prognostic evaluation. Neuroradiology 2004;46:916–22.
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, et al. Surgical vs nonoperative treatment for lumbar disk herniation: The Spine Patient Outcomes Research Trial (SPORT): A randomized trial. JAMA 2006;296:2441–50.
Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine (Phila Pa 1976) 2005;30:927–35.
Barrios C, Ahmed M, Arrotegui JI, Björnsson A. Clinical factors predicting outcome after surgery for herniated lumbar disc: An epidemiological multivariate analysis. J Spinal Disord 1990;3:205–9.
Blazhevski B, Filipche V, Cvetanovski V, Simonovska N. Predictive value of the duration of sciatica for lumbar discectomy. Prilozi 2008;29:325–35.
Fisher C, Noonan V, Bishop P, Boyd M, Fairholm D, Wing P, et al. Outcome evaluation of the operative management of lumbar disc herniation causing sciatica. J Neurosurg 2004;100:317–24.
Folman Y, Shabat S, Catz A, Gepstein R. Late results of surgery for herniated lumbar disk as related to duration of preoperative symptoms and type of herniation. Surg Neurol 2008;70:398–401.
Gaetani P, Aimar E, Panella L, Debernardi A, Tancioni F, Rodriguez y Baena R. Surgery for herniated lumbar disc disease: Factors influencing outcome measures. An analysis of 403 cases. Funct Neurol 2004;19:43–9.
Safari GH, Nayebaghaie H, Azhari SJ, Shabehpour M. Prognostic value of preoperative sciatalgia in lumbar disc surgery. Arch Iranian Med 2005;8:300–3.
Hurme M, Alaranta H. Factors predicting the result of surgery for lumbar intervertebral disc herniation. Spine (Phila Pa 1976) 1987;12:933–8.
Jönsson B. Patient-related factors predicting the outcome of decompressive surgery. Acta Orthop Scand Suppl 1993;251:69–70.
Junge A, Dvorak J, Ahrens S. Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine (Phila Pa 1976) 1995;20:460–8.
Moranjkić M, Ercegovic Z, Hodzic M, Brikic H. Outcome prediction in lumbar disc herniation surgery. Acta Med Sal 2010;39:75–80.
Ng LC, Sell P. Predictive value of the duration of sciatica for lumbar discectomy. A prospective cohort study. J Bone Joint Surg Br 2004;86:546–9.
Nygaard OP, Kloster R, Solberg T. Duration of leg pain as a predictor of outcome after surgery for lumbar disc herniation: A prospective cohort study with 1-year followup. J Neurosurg 2000;92:131–4.
Nygaard OP, Romner B, Trumpy JH. Duration of symptoms as a predictor of outcome after lumbar disc surgery. Acta Neurochir (Wien) 1994;128:53–6.
Pearson A, Lurie J, Tosteson T, Zhao W, Abdu W, Weinstein J. Who should have surgery for spinal stenosis? Treatment effect predictors in SPORT. Spine (Phila Pa 1976) 2012;37:1792–802.
Quigley MR, Bost J, Maroon JC, Elrifai A, Panahandeh M. Outcome after microdiscectomy: Results of a prospective single institutional study. Surg Neurol 1998;49:263–7.
Rihn JA, Hilibrand AS, Radcliff K, Kurd M, Lurie J, Blood E, et al. Duration of symptoms resulting from lumbar disc herniation: Effect on treatment outcomes: Analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am 2011;93:1906–14.
Rothoerl RD, Woertgen C, Brawanski A. When should conservative treatment for lumbar disc herniation be ceased and surgery considered? Neurosurg Rev 2002;25:162–5.
Silverplats K, Lind B, Zoëga B, Halldin K, Rutberg L, Gellerstedt M, et al. Clinical factors of importance for outcome after lumbar disc herniation surgery: Long term followup. Eur Spine J 2010;19:1459–67.
Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976) 1983;8:131–40.
Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med 2007;356:2245–56.
Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW, Leiden-The Hague Spine Intervention Prognostic Study Group. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: Two year results of a randomised controlled trial. BMJ 2008;336:1355–8.
Vroomen PC, de Krom MC, Knottnerus JA. Predicting the outcome of sciatica at short-term followup. Br J Gen Pract 2002;52:119–23.
Sutheerayongprasert C, Paiboonsirijit S, Kuansongtham V, Anuraklekha S, Hiranyasthiti N, Neti S. Factors predicting failure of conservative treatment in lumbar-disc herniation. J Med Assoc Thai 2012;95:674–80.
Peul WC, Arts MP, Brand R, Koes BW. Timing of surgery for sciatica: Subgroup analysis alongside a randomized trial. Eur Spine J 2009;18:538–45.
Osterman H, Seitsalo S, Karppinen J, Malmivaara A. Effectiveness of microdiscectomy for lumbar disc herniation: A randomized controlled trial with 2 years of followup. Spine (Phila Pa 1976) 2006;31:2409–14.
Salenius P, Laurent LE. Results of operative treatment of lumbar disc herniation. A survey of 886 patients. Acta Orthop Scand 1977;48:630–4.
Dvorak J, Gauchat MH, Valach L. The outcome of surgery for lumbar disc herniation. I. A 4-17 years’ followup with emphasis on somatic aspects. Spine (Phila Pa 1976) 1988;13:1418–22.
Akagi R, Aoki Y, Ikeda Y, Nakajima F, Ohtori S, Takahashi K, et al. Comparison of early and late surgical intervention for lumbar disc herniation: Is earlier better? J Orthop Sci 2010;15:294–8.
Coderre TJ, Katz J, Vaccarino AL, Melzack R. Contribution of central neuroplasticity to pathological pain: Review of clinical and experimental evidence. Pain 1993;52:259–85.
Torebjörk HE, Lundberg LE, LaMotte RH. Central changes in processing of mechanoreceptive input in capsaicin-induced secondary hyperalgesia in humans. J Physiol 1992;448:765–80.
Cameron AA, Cliffer KD, Dougherty PM, Willis WD, Carlton SM. Changes in lectin, GAP-43 and neuropeptide staining in the rat superficial dorsal horn following experimental peripheral neuropathy. Neurosci Lett 1991;131:249–52.
Sugimoto T, Bennett GJ, Kajander KC. Transsynaptic degeneration in the superficial dorsal horn after sciatic nerve injury: Effects of a chronic constriction injury, transection, and strychnine. Pain 1990;42:205–13.
Mao J, Price DD, Coghill RC, Mayer DJ, Hayes RL. Spatial patterns of spinal cord [14C]-2-deoxyglucose metabolic activity in a rat model of painful peripheral mononeuropathy. Pain 1992;50:89–100.
Gorecki J, Hirayama T, Dostrovsky JO, Tasker RR, Lenz FA. Thalamic stimulation and recording in patients with deafferentation and central pain. Stereotact Funct Neurosurg 1989;52:219–26.
Hirayama T, Dostrovsky JO, Gorecki J, Tasker RR, Lenz FA. Recordings of abnormal activity in patients with deafferentation and central pain. Stereotact Funct Neurosurg 1989;52:120–6.
Lenz FA, Kwan HC, Dostrovsky JO, Tasker RR. Characteristics of the bursting pattern of action potentials that occurs in the thalamus of patients with central pain. Brain Res 1989;496:357–60.
Rinaldi PC, Young RF, Albe-Fessard D, Chodakiewitz J. Spontaneous neuronal hyperactivity in the medial and intralaminar thalamic nuclei of patients with deafferentation pain. J Neurosurg 1991;74:415–21.
Jancalek R, Dubovy P. An experimental animal model of spinal root compression syndrome: An analysis of morphological changes of myelinated axons during compression radiculopathy and after decompression. Exp Brain Res 2007;179:111–9.
Brisby H, Balagué F, Schafer D, Sheikhzadeh A, Lekman A, Nordin M, et al. Glycosphingolipid antibodies in serum in patients with sciatica. Spine (Phila Pa 1976) 2002;27:380–6.
Chen C, Cavanaugh JM, Ozaktay AC, Kallakuri S, King AI. Effects of phospholipase A2 on lumbar nerve root structure and function. Spine (Phila Pa 1976) 1997;22:1057–64.
Franson RC, Saal JS, Saal JA. Human disc phospholipase A2 is inflammatory. Spine (Phila Pa 1976) 1992;17:S129–32.
Olmarker K, Blomquist J, Strömberg J, Nannmark U, Thomsen P, Rydevik B. Inflammatogenic properties of nucleus pulposus. Spine (Phila Pa 1976) 1995;20:665–9.
Saal JS, Franson RC, Dobrow R, Saal JA, White AH, Goldthwaite N. High levels of inflammatory phospholipase A2 activity in lumbar disc herniations. Spine (Phila Pa 1976) 1990;15:674–8.
Brisby H, Olmarker K, Rosengren L, Cederlund CG, Rydevik B. Markers of nerve tissue injury in the cerebrospinal fluid in patients with lumbar disc herniation and sciatica. Spine (Phila Pa 1976) 1999;24:742–6.
Brisby H, Byröd G, Olmarker K, Miller VM, Aoki Y, Rydevik B. Nitric oxide as a mediator of nucleus pulposus-induced effects on spinal nerve roots. J Orthop Res 2000;18:815–20.
Takahashi H, Suguro T, Okazima Y, Motegi M, Okada Y, Kakiuchi T. Inflammatory cytokines in the herniated disc of the lumbar spine. Spine (Phila Pa 1976) 1996;21:218–24.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sabnis, A.B., Diwan, A.D. The timing of surgery in lumbar disc prolapse: A systematic review. IJOO 48, 127–135 (2014). https://doi.org/10.4103/0019-5413.128740
Published:
Issue Date:
DOI: https://doi.org/10.4103/0019-5413.128740