Abstract
Background
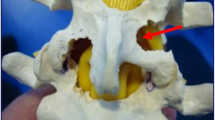
Ideal surgical treatment for thoracic disc herniation (TDH) is controversial due to variations in patient presentation, pathology, and possible surgical approach. Althougth discectomy may lead to improvements in neurologic function, it can be complicated by approach related morbidity. Various posterior surgical approaches have been developed to treate TDH, but the gold standard remains transthoracic decompression. Certain patients have comorbidities and herniation that are not optimally treated with an anterior approach. A transfacet pedicle approach was first described in 1995, but outcomes and complications have not been well described. The aim of this work was to evaluate the clinical effect and complications in a consecutive series of patients with symptomatic thoracic disc herniations undergoing thoracic discectomy using a modified transfacet approach.
Materials and Methods
33 patients with thoracic disc herniation were included in this study. Duration of the disease was from 12 days to 36 months, with less than 1 month in 13 patients. Of these, 15 patients were diagnosed with simple thoracic disc herniation, 6 were associated with ossified posterior longitudinal ligament, and 12 with ossified or hypertrophied yellow ligament. A total of 45 discs were involved. All the herniated discs and the ossified posterior longitudinal ligaments were excised using a modified transfacet approach. Laminectomy and replantation were performed for patients with ossified or hypertrophied yellow ligament. The screw–rod system was used on both sides in 14 patients and on one side in l9 patients.
Results
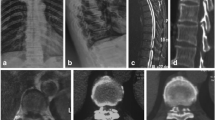
29 patients were followed up for an average of 37 months (range 12-63 months) and 4 patients were lost to followup. Evaluation was based on Epstein and Schwall criteria.5 15 were classified as excellent and 10 as good, accounting for 86.21% (25/29); 2 patients were classified as improved and 2 as poor. All the patients recovered neurologically after surgery. A total of 25 patients had significantly improved motor function from 3 to 6 months after surgery and 10 patients had slow recovery 6 months after surgery.. Of the three patients with postoperative complications, two had exacerbated preexisting defects and one had implant failure. Postoperative computed tomography or magnetic resonance imaging showed that all patients had well fused replanted lamina and completely decompressed canal.
Conclusion
Thoracic discectomy using a modified transfacet approach can significantly improve the clinical outcomes.
Similar content being viewed by others
References
Arce CA, Dohrmann GJ. Thoracic disc herniantion. Surg Neurol 1985;3:383–92.
Carson J, Gumpert J, Jefferson A. Diagnosis and treatment of thoracic intervertebral disc protrusions. J Neurol Neurosurg Psychiatry 1971;34:68–77.
Oppenheim JS, Rothman AS, Sachdev VP. Thoracic herniated discs: Review of the literature and 12 cases. Mt Sinai J Med 1993;60:321–6.
Arseni C, Nash F. Thoracic intervertebral disc protrusion: A clinical study. J Neurosurg 1960;17:418–30.
Stetkarova I, Chrobok J, Ehler E, Kofler M. Segmengtal abdominal wall paresis caused by lateral low thoracic disc herniation. Spine (Phila Pa 1976) 2007;32:E635–9.
Baranto A, Börjesson M, Danielsson B, Hellström M, Swärd L. Acute chest pain in a top soccer player due to thoracic disc herniation. Spine 2009;34:359–62.
Mitra SR, Gurjar SG, Mitra KR. Degenerative disease of the thoracic spine in central India. Spine Cord 2009;34:333–7.
Okada Y, Shimizu K, Ido K, Kotani S. Multiple thoracic disc herniations: Case report and review of the literature. Spinal Cord 1997;35:183–6.
Mulier S, Debois V. Thoracic disc herniations: Transthoracic, lateral, or posterolateral approach? A review. Surg Neurol 1998;49:606–8.
Stillerman CB, Chen TC, Day JD, Couldwell WT, Weiss MH. The transfacet pedicle-sparing approach for thoracic disc removal: Cadaveric morphometric analysis and preliminary clinical experience. J Neurosurg 1995;83:971–6.
Piccirilli M, Tarantino R, Anichini G, Delfini R. Multiple disc herniations in a type II diabetic patient: Case report and review of the literature. J Neurosurg Sci 2008;52:83–5.
Boriani S, Biagini R, De Iure F, Rocella P, Veronesi V, Dalbuono S, et al. Two-level thoracic disc herniation. Spine (PhilaPa 1976) 1994;19:2461–6.
Ohnishi K, Miyamoto K, Kanamori Y, Kodama H, Hosoe H, Shimizu K. Anterior decompression and fusion for multiple thoracic disc herniation. J Bone Joint Surg Br 2005;87:356–60.
Chen CF, Chang MC, Liu CL, Chen TH. Acute noncontiguous multiple-level thoracic disc herniations with myelopathy: A case report. Spine (Phila Pa 1976) 2004;29:E157–60.
Sekhar LN, Jannetta PJ. Thoracic disc herniation: Operative approaches and results. Neurosurgery 1983;12:303–5.
Lau D, Song Y, Guan Z, Sullivan S, La Marca F, Park P. Perioperative characteristics, complications and outcomes of single-level versus multilevel thoracic corpectomies via modified costotransversectomy approach. Spine (Phila Pa 1976) 2013;38:523–30.
Takahata M, Ito M, Abumi K, Kotani Y, Sudo H, Minami A. Clinical results and complications of circumferential spinal cord decompression through a single posterior approach for thoracic myelopathy caused by ossification of posterior longitudinal ligament. Spine (Phila Pa 1976) 2008;33:1199–208.
Uribe JS, Smith WD, Pimenta L, Härtl R, Dakwar E, Modhia UM, et al. Minimally invasive lateral approach for symptomatic thoracic disc herniation: Initial multicenter clinical experience. J Neurosurg Spine 2012;16:264–79.
Ayhan S, Nelson C, Gok B, Petteys RJ, Wolinsky JP, Witham TF, et al. Transthoracic surgical treatment for centrally located thoracic disc herniations presenting with myelopathy: A 5-year institutional experience. J Spinal Disord Tech 2010;23:79–88.
Patterson RH Jr, Arbit E. A surgical approach through the pedicle to protruded thoracic discs. J Neurosurg 1978;8:768–72.
Singounas EG, Kypriades EM, Kellerman AJ, Garvan N. Thoracic disc herniation: Analysis of 14 cases and review of the literature. Acta Neurochir (Wien) 1992;116:49–52.
Wang YT, Chen ZH, Li M, Zhen YP. Lumbar spinal canal expansion angioplasty: Clinical applications of replantation of disected lamina and spinous process graft. Chin J Orthop 1995;15:644–7.
Zheng YP, Liu XY, Du W, Yuan SM. Treatment of thoracic ligamentum flavum ossification using total laminectomy replantation and spinal expand angioplasty. Chin J Orthop 2004;2402:728–32.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, X., Liu, X. & Zheng, Y. Surgical treatment of thoracic disc herniations using a modified transfacet approach. IJOO 48, 158–162 (2014). https://doi.org/10.4103/0019-5413.128756
Published:
Issue Date:
DOI: https://doi.org/10.4103/0019-5413.128756