Abstract
Background:
Chronic obstructive pulmonary disease (COPD) is one of the most common causes of mortality and a major contributor to morbidity. Longitudinal clinical practice data yielding information on the characteristics of the disease, its natural course, and management are limited.
Aims:
To investigate and describe the COPD population from a nationwide perspective during an 11-year period (1999–2009) with a focus on management, co-morbidity, and mortality.
Methods:
This observational retrospective epidemiological study linked electronic medical records data from patients with COPD in primary care to mandatory Swedish hospital, drug and Cause of Death registry data from 1999 to 2009 (PATHOS).
Results:
A total of 21,361 patients with a COPD diagnosis were included (mean age 68.0 years, 53% females). The proportion of patients diagnosed in primary care increased from 59% in 1999 to 81% in 2009 and the mean age at diagnosis decreased from 73 to 66 years. The number of exacerbations decreased from 3.0 to 1.3 and COPD-related hospitalisations decreased from 1.02 to 0.20 per patient per year. Prescriptions of long-acting muscarinic antagonists and fixed combinations of inhaled corticosteroid/long-acting β2-agonist inhalers increased from 0% to 36% and 37%, respectively. The most common co-morbidities were hypertension, heart failure, ischaemic heart disease, and diabetes. Overall life expectancy was 8.3±6.8 years shorter in patients with COPD than in the general population, and all-cause mortality was 3.5 times higher.
Conclusions:
Management of COPD in Sweden has improved during the 11-year study period. Despite this, patients with COPD have a substantially reduced life expectancy than the general population.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a slowly progressive disease characterised by airflow limitation and recurrent periods of worsening/exacerbations, and is estimated to soon be the third most common cause of mortality.1,2 It is recognised that COPD is associated with a high prevalence of co-morbid conditions, implying further negative impact on quality of life and prognosis.3–6 Exacerbations are the most important cause of morbidity in COPD, causing personal suffering and high healthcare costs.7 Once patients with COPD have had to visit an emergency department/ hospitalisation for a worsening/exacerbation, they have a higher risk of re-hospitalisation and mortality.8–10
Over the past decade the development and gradual implementation of evidence-based international and national guidelines for COPD management (e.g. the Global Initiative for Chronic Obstructive Lung Disease [GOLD]2) has increased the attention on COPD as a separate condition and brought awareness of the importance of early diagnosis. Despite this, COPD is still both under-recognised and under-diagnosed.11–13 This, combined with the increasing ageing population and exposure to risk factors such as smoking, leads to a continuously increasing prevalence of the disease.2,14 Data from Western countries show that almost 6% of the population is currently affected by COPD.2,14 In Sweden, the prevalence of COPD in the population over 45 years of age is approximately 8%.11,15
COPD management comprises a number of different approaches such as smoking cessation, physical exercise, vaccinations, patient education, and pharmacological treatment. Despite the availability of COPD management guidelines, optimal patient handling and best practice are still under debate and differ both within and between countries.
In Sweden, the healthcare organisation is primary care based. This is also where the main responsibility for the management of patients with COPD lies.16 As observed in other Western countries, COPD has gradually become more recognised in Sweden over the past 10 years; the awareness of COPD as a public health problem has increased both in the medical community and in the general population. However, actual clinical longitudinal data on the prevalence, disease characteristics, natural course, and management of COPD are scarce or absent.
In an observational retrospective Swedish registry-based study, data from patients with COPD generated during the first decade of the 21st century were examined from a nationwide perspective. The aim was to describe the COPD population, the disease characteristics, and the management of COPD by longitudinal data over 11 years with an emphasis on prevalence, incidence, exacerbations, co-morbidities, and mortality.
Methods
Study design, method, and data sources
This was an observational retrospective registry study linking primary care medical records data to data from national mandatory Swedish registries.17 Data linkage was performed by the Swedish National Board of Health and Welfare and the linked database was managed by the Department of Public Health and Caring Sciences, Uppsala University, Sweden.
In Sweden, primary care is organised into healthcare centres, providing the compulsory first point of contact for a defined registered population and referring patients to secondary care only when there is a need for specialist consultation. In Sweden there are about 1,000 primary healthcare centres. Of these, a total of 76 primary healthcare centres with a catchment area of approximately 800,000 individuals were included in the study. No formal centre stratification was performed, but effort was made to ensure a selection covering a representative sample of the population and COPD healthcare by a mix of rural and urban areas, public and private providers, and centre size.
Electronic primary care medical records data (e.g. date of birth, gender, diagnoses according to the International Classification of Diseases, 10th revision, Clinical Modification codes [ICD-10-CM], number of contacts, lung function measurements, and drug prescriptions) were extracted using an established software system (Pygargus Customized eXtraction Program, CXP; Pygargus AB, Stockholm, Sweden).18 The social security numbers of identified patients were replaced with study identification numbers prior to data processing. Data were also extracted retrospectively from mandatory Swedish national registries. Morbidity and mortality data were collected from the National Patient Register, inpatient hospital care (admission and discharge dates, main and secondary diagnoses), and outpatient hospital care (number of contacts and diagnoses as specified by ICD-10-CM codes) and the Cause of Death register (date and cause of death). Data on drug prescriptions were collected from the Swedish Prescribed Drug Register (prescription date, drug type, dose, and pack size). General population data (e.g. number and gender distribution per each year class) were generated by Statistics Sweden (SCB), Stockholm, Sweden.
The study protocol was reviewed and approved by the regional ethics committee in Uppsala, Sweden (reference number 2010/040) and registered at ClinicalTrials.gov (clinical trial identifier NCT01146392).
Study population
All male and female patients of any age with physician-diagnosed COPD (ICD-10-CM code J44) or a prescription of an inhaled anticholinergic drug (Anatomical Therapeutic Classification [ATC] System class R03BB04/R03BB01; ipratropium bromide or tiotropium bromide) in the primary care medical records were eligible. Following linkage to national register data, patients with a prescription of the above medications in primary care and a COPD diagnosis in secondary care were also included. Patients lacking a COPD diagnosis in either medical records or registries and patients with a COPD diagnosis only present in the Cause of Death register were excluded. No other exclusion criteria were predefined. Patients were followed from 1st January 1999 to 31st December 2009, or until emigration or death. The index date was defined as the first date of COPD diagnosis.
Study measures and statistical methods
Incidence: the number of new cases found in the medical records per year.
Prevalence: the accumulated incidence per year for patients >40 years of age.19 Population data from SCB were used and subdivided by year and gender.
Prescriptions of inhaled drugs used in obstructive pulmonary diseases: defined as inhaled corticosteroids (ICS; ATC code R03BA), long-acting β2-agonists (LABA; R03AC12 and R03AC13), short-acting β2-agonists (SABA; R03AC), long-acting muscarinic antagonists (LAMA; R03BB01), short-acting muscarinic antagonists (SAMA; R03BB04), and fixed ICS/LABA combinations (R03AK06 and R03AK07).
Exacerbation: defined as hospitalisations (ICD-10-CM code J44 as primary diagnosis or J44.0/J44.1 as secondary diagnosis), emergency visits (ICD-10-CM code J44.0/J44.1 in outpatient hospital care), or use of oral steroids (ATC code H02AB) or antibiotics (ATC code J01AA, J01CA) because of respiratory symptoms. Repeated exacerbations occurring within 14 days were calculated as one single event.
Co-morbidity: identified using ICD-10-CM codes: C33–34, lung cancer; E10–15, diabetes; F32–33, depression; I10–I15, hypertension; I21, acute myocardial infarction; I20–I25, ischaemic heart disease; I50, heart failure; I61–I64, stroke; J10–J18, pneumonia; and M80–82, osteoporosis. Co-morbidity data are presented as a percentage of the COPD population alive at two years prior to index, at diagnosis, four and eight years post diagnosis, and at any time in the study. The Deyo-modified Charlson co-morbidity index was used to calculate co-morbidity covering 17 serious disease areas, including COPD, with the value reflecting the number of these co-morbidities.20,21
Mortality: identified according to the Cause of Death register, mortality for years 1999–2009 and cause of death for years 1999–2008 (due to report delay) were calculated. Life expectancy in the COPD population was compared with the total population in Sweden with the same age and gender distribution as the patients with COPD at the index date.
Standardised death rate: calculated using the direct method for age adjustment (i.e. using the age structure for the study population at the date when the patient was diagnosed with COPD).
Lung function data: collected from one county council (22 of the 76 included centres) due to its complete lung function data coverage in an available central database.
Smoking habits: collected from a free text field search in the electronic medical records using the patient's mode value.
Education: Analysed on a 4-level scale by the highest given level of total years of education: ≤9 years, 10–11 years, 12–14 years, or ≥15 years of education. General population data (e.g. number and gender distribution per year class) were generated by SCB.
Statistical methods
The main statistical analyses were descriptive and data are presented using standard summary measures such as mean (standard deviation) and frequency (%). COPD-related events were calculated using Poisson regression. Data management and statistical analyses were performed using SAS Version 9.2 (SAS Institute Inc, Cary, NC, USA).
Results
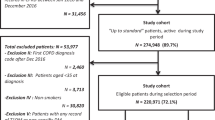
Overall, 27,394 patients with a recorded diagnosis of COPD and/or a prescription of short-acting or long-acting muscarinic antagonists were identified from the electronic medical records. Of these, 6,033 patients did not fulfil the inclusion criteria and were excluded from the analyses (5,949 patients did not have a COPD diagnosis either in their medical records or in the national registers and 84 patients had a recorded COPD diagnosis only in the Cause of Death register). Thus, the study population meeting the inclusion criteria of a recorded COPD diagnosis within the period consisted of 21,361 patients (mean age 68.0 years, 53% females; Table 1) and covered 98,942 patient-years. During the two years prior to COPD diagnosis, 70% of patients had at least one recorded exacerbation, defined as a prescription of oral steroids (34%) and/or antibiotics (54%) due to respiratory symptoms. A total of 36% of the patients had a prescription of inhaled steroids two years prior to diagnosis (Table 1). Furthermore, 19% of the population had a recorded diagnosis of pneumonia and 25% had an asthma diagnosis two years prior to receiving the COPD diagnosis.
During the study period, patients were hospitalised (independent of cause) more than 190,000 times, had 3.5 million primary healthcare centre contacts, and more than 1.34 million prescriptions were issued. By the end of the study period a higher proportion of patients with COPD were detected and diagnosed in primary care compared with the beginning of the study period (81% vs. 59%). Patients were also, on average, seven years younger when they received the COPD diagnosis in 2009 than was the case at the start of the study in 1999 (66 vs. 73 years of age).
Both the incidence and prevalence rates increased during the study period (Figure 1). By 2009, the COPD prevalence was 3.6% for women and 3.2% for men.
The proportion of the population >40 years of age receiving their COPD diagnosis in primary care increased from 0.9% in 1999 to 3.4% in 2009.
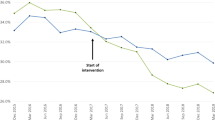
Prescriptions of LAMA (tiotropium bromide) and fixed ICS/LABA combinations increased from 0% to 36% and 37%, respectively, during the study period (Figure 2). Simultaneously, the number of exacerbations after the index date decreased from 3.0 to 1.3 per patient per year (Figure 3). In addition, the number of hospitalisations because of COPD decreased from 1.02 to 0.20 per patient per year (Figure 3), and a similar trend was observed for prescriptions of antibiotics (from 0.54 to 0.39 prescriptions per patient per year) and oral steroids (from 1.40 to 0.70 prescriptions per patient per year), and emergency visits (from 0.08 to 0.02 visits per patient per year) (Figure 3).
All registered co-morbid conditions increased following COPD diagnosis (Table 2). The most commonly reported co-morbidity was hypertension, followed by heart failure, ischaemic heart disease, and diabetes (Table 2). Following the index date, 23% of the patients received an asthma diagnosis. Furthermore, 4.6% of the patients developed lung cancer within eight years of the index date (Table 2); in approximately 0.7% of these patients the lung cancer was diagnosed concomitantly with the COPD diagnosis. Forty-two per cent of patients with COPD had a recorded pneumonia diagnosis (in all, 15,353 recorded diagnoses) after the index date, the majority of which were diagnosed either in a primary care (47%) or in-patient hospital (44%) setting; the remaining 9% were diagnosed in outpatient hospital care. The mean (SD) number of co-morbidities per patient increased from 0.72 (0.72) two years prior to the index date to 1.74 (1.47) at eight years after the initial COPD diagnosis (Table 2). At the date of the COPD diagnosis, the Charlson co-morbidity index had a mean (SD) value of 1.62 (0.97) and 39% of the patients had at least one co-morbidity. With regard to the two most common co-morbidities, 25.2% of patients diagnosed in 1999 had hypertension and 18.1% had heart failure while, in 2009, 44.0% had hypertension and 13.1% had heart failure.
Overall, 7,389 (35%) patients died during the study period; of these, 5,434 patients had an available registered underlying cause of death (data missing due to report delay). The death rate during this period was higher for males than for females (Figure 1). Overall life expectancy (SD) for the COPD study population was 8.3 (6.8) years lower than in the average Swedish population, 9.4 years lower for women and 7.4 years lower for men. All-cause mortality was 3.5 times higher in the study population (age standardised) compared with the death rate in the Swedish population, while the death rate for lung diseases (ICD10; J00–J99) increased by a factor of 15 and death due to heart failure showed a four-fold increased risk in the study population (Table 3).
Complete lung function data were available for patients from one county council, which included 29% of the primary healthcare centres evaluated. One-third of patients were in disease stage 3–4 according to GOLD 2011 guidelines during the study period (Table 4). At diagnosis, the forced expiratory volume in one second (FEV1) percentage of predicted normal was 47% in 1999 and 65% in 2009. The mean post-bronchodilator FEV1 (percentage of predicted) at diagnosis during the whole period was 62% and 57% at the last available measurement, while the post-bronchodilator FEV1/forced vital capacity ratio was 0.64 and 0.60, respectively.
Information on smoking was recorded in the electronic medical records for one-third of the patients (n=7,004). During the two years prior to receiving the COPD diagnosis, 3,968 (57%) patients were recorded as smokers, 3,036 as non-smokers, and 200 patients were recorded as never smokers. The smoking status remained relatively stable during the study period, without any trend for smoking cessation following COPD diagnosis. The remaining 14,357 patients had no smoking status extractable from their medical records during the study period.
The educational level was generally lower in the study population than in an age- and gender-matched equivalent Swedish population. Although a shift towards higher education was observed, the difference in educational level between the populations was more pronounced by the end of the study period than it was in 1999. The lowest level of education (≤9 years at school) decreased in both populations (by 14.0% in the COPD population and 18.2% in the general population), while the proportion of individuals graduating from higher education (≥12 years) increased by 9.7% and 12.8%, respectively.
Discussion
Main findings
The present observational retrospective register study demonstrates that the management of COPD has improved during the 11-year study period from 1999 to 2009. More patients are diagnosed at a younger age, new treatment options have become available, and the numbers of exacerbations and hospitalisations due to COPD have decreased. Despite this, almost three-quarters of the patients were not diagnosed with COPD at the time of experiencing a COPD exacerbation. Life expectancy was more than eight years shorter and the all-cause mortality rate was three times higher in the COPD population compared with the general Swedish population.
Strengths and limitations of this study
This study has several important strengths. The primary care population at the participating centres (selected to ensure a representative sample of centres across Sweden) covered approximately 800,000 individuals, corresponding to approximately 8% of the Swedish population. Data were obtained from the primary care medical records and linked to data from national healthcare registers with high coverage and quality. The registers are mandatory and have no restrictions for inclusion such as age, employment status, concomitant medications, co-morbidities, or healthcare insurances. This study included more than 21,000 patients with COPD, followed for up to 11 years, covering close to 99,000 patient-years. As most patients with COPD in Sweden are managed in the primary care setting, the study covers a majority of the COPD population. By the ability to monitor each patient through his or her treatment journey using the individual's personal identification number, this study provides solid and unique data that is highly generalisable to the COPD population in primary care.
The present study is, however, not without limitations. It is a retrospective observational registry study, in which data retrieval is limited to the variables registered in the databases. Although all patients had physician-diagnosed COPD, the accuracy of the COPD diagnoses and the severity of the disease could not be verified. Only one-third of the primary healthcare centres had extractable spirometry data as there is no common routine for its documentation in the medical records. Furthermore, data on non-pharmaceutical COPD therapies, such as exercise and smoking cessation programmes, were incomplete due to lack of either registration or structured reporting in the medical records. Smoking status could only be extracted from one-third of the medical records. The use of COPD medications is based on prescription claims; patients' actual adherence to treatment is unknown. Exacerbations prior to COPD diagnosis are defined as prescription of oral steroids and/or antibiotics due to respiratory symptoms. This could include prescription of antibiotics without reference to airway obstruction.
Interpretation of findings in relation to previously published work
The prevalence of COPD in Sweden in the primary care setting increased during the study period, reaching average levels of slightly over 3% by 2009 in the population aged >40 years. This proportion is lower than that generally reported in epidemiological studies for a Western population, with an average prevalence close to 6%,2 although considerable variability has been noted both across European countries (0.7–9.7%) and regionally within a given country.22 Recent data from a geographically restricted area in Sweden, presented by Danielsson and co-workers,15 indicate a 6.7% prevalence of COPD stage 2 or higher. The lower percentage seen in the present study is likely to be related to under-diagnosis of mild COPD.11
Patients were diagnosed with COPD at a younger age in 2009 compared with 1999. This seven-year difference in age at diagnosis (66 years in 2009 vs. 73 years at start of data collection in 1999) is most likely a reflection of the increased acknowledgement of COPD as a separate condition among healthcare professionals, but may also partly be the result of higher patient disease awareness. An important contribution to this improvement in COPD detection is the more structured management of COPD in primary care. The increased accessibility to spirometers at healthcare centres over the study period, enabling today's routine use of spirometry in primary care, has enhanced the possibility of correct diagnosis.23–25 The improved care and earlier diagnosis are probably the most important factors explaining the reported decreased exacerbation rate. Despite this, the present study also clearly shows that there is room for improvement as a clear majority of patients (70%) experienced at least one exacerbation prior to receiving their COPD diagnosis.
Several studies have reported on the level of co-morbidity observed in patients with COPD and the association with a higher risk of having co-morbid hypertension, cardiovascular diseases, diabetes, osteoporosis, and other smoking-related conditions.3,26 Cardiovascular disease has been reported to become more prevalent with increasing COPD severity and, apart from affecting overall quality of life, to increase the mortality risk.27 In the present study the most common co-morbid condition was hypertension, followed by heart failure, ischaemic heart disease, and diabetes. During the two years prior to the index date, one-quarter of patients had a registered asthma diagnosis and one-third were on pre-index treatment with ICS, indicating either asthma co-morbidity or a preceding incorrect asthma diagnosis. After the index date, one-quarter of the patients were diagnosed with concomitant asthma. These data are similar to those reported in previous COPD studies where co-diagnosed asthma has been reported in up to 40% of all patients with COPD.5,28
The severity of the disease is further demonstrated by the high mortality seen in previously published reviews.22,29 In addition, a recent paper by Sundh and co-workers30 demonstrated an association between increased mortality risk and lower health status, with a standardised mortality rate approximately 2–6 times higher for patients with COPD compared with the general Swedish population. The mortality rate in our population was 3.5 times higher than in the general Swedish population and the overall life expectancy was shown to be reduced by eight years.
Implications for future research, policy and practice
Most patients with COPD in Sweden are diagnosed and managed in the primary care setting. During the course of the 11-year study period, patients' age decreased at the time of COPD diagnosis and, thus, was more likely to occur at an earlier stage of the disease. These tendencies indicate improved disease awareness. However, while this is a clear indication that there is improvement in COPD diagnosis in primary care, as one-fifth of the patients were diagnosed in secondary care and a considerable number had a recorded exacerbation preceding their initial COPD diagnosis, disease awareness can be improved further.
As patients with COPD also present with a high risk of having co-morbid conditions that affect their disease prognosis, the present study and the findings of Mannino and co-workers26 highlight the importance of a comprehensive view of the patient, focusing on the whole individual rather than COPD as a separate condition. The increased number of co-morbidities over time shows that patients with COPD commonly develop more than one smoking-related disease and, as the most common co-morbidities were all related to some form of cardiovascular disease, emphasises the importance of taking these co-morbidities into consideration when managing patients with COPD.31
Conclusions
The results of this study provide important knowledge that increases the understanding of COPD, the needs of the patient, and the burden on the healthcare system. Disease awareness and management of COPD in primary care improved in Sweden during the study period, indicated by earlier diagnosis and a decrease in exacerbations and COPD-related hospitalisations. The introduction of new treatment options, the younger age, and the less severe disease stage at diagnosis are likely to be important contributors to the reduced number of exacerbations. However, the high mortality in patients with COPD indicates that there is still room for improvement in the management of the disease.
References
World Health Organization. Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach, 2007. Available from: www.who.int/respiratory/copd/
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2011. Available from: http://www.goldcopd.org/
Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL . Patterns of comorbidity in newly diagnosed COPD and asthma in primary care. Chest 2005;128(4):2099–107. http://dx.doi.org/10.1378/chest.128.4.2099
Gudmundsson G, Gislason T, Janson C, et al. Depression, anxiety and health-related quality of life at discharge after hospitalisation for exacerbation of COPD: a multicenter study in the Nordic countries. Respir Med 2006;100(1):87–93. http://dx.doi.org/10.1016/j.rmed.2005.04.003
van der Molen T . Co-morbidities of COPD in primary care: frequency, relation to COPD, and treatment consequences. Prim Care Respir J 2010;19(4):326–34. http://dx.doi.org/10.4104/pcrj.2010.00053
Sundh J, Ställberg B, Lisspers K, Montgomery S, Janson C . Comorbidity, body mass index and quality of life in COPD using the Clinical COPD Questionnaire. J COPD 2011;8(3):173–81. http://dx.doi.org/10.3109/154
Toy EL, Gallagher KF, Stanley EL, Swensen AR, Duh MS . The economic impact of exacerbations of chronic obstructive pulmonary disease and exacerbation definition: a review. J COPD 2010;7(3):214–28. http://dx.doi.org/10.3109/15412555.2010.481697
Chu CM, Chan VL, Lin AW, Wong IW, Leung WS, Lai CK . Readmission rates and life threatening events in COPD survivors treated with non-invasive ventilation for acute hypercapnic respiratory failure. Thorax 2004;59(12):1020–5. http://dx.doi.org/10.1136/thx.2004.024307
Gudmundsson G, Gislason T, Janson C, et al. Risk factors for rehospitalisation in COPD: the role of health status, anxiety and depression. A multicenter study in the Nordic countries. Eur Respir J 2005;26(3):414–19. http://dx.doi.org/10.1183/09031936.05.00078504
Gudmundsson G, Ulrik CS, Gislason T, et al. Long-term survival in patients hospitalized for chronic obstructive pulmonary disease: a prospective observational study in the Nordic countries. Int J COPD 2012;7:571–6. http://dx.doi.org/10.2147/COPD.S34466.
Lindberg A, Bjerg A, Rönmark E, Larsson LG, Lundbäck B . Prevalence and underdiagnosis of COPD by disease severity and the attributable fraction of smoking. Report from the Obstructive Lung Disease in Northern Sweden Studies. Respir Med 2006;100(2):264–72. http://dx.doi.org/10.1016/j.rmed.2005.04.029
Bednarek M, Maciejewski J, Wozniak M, Kuca P, Zielinski J . Prevalence, severity and underdiagnosis of COPD in the primary care setting. Thorax 2008;63(5):402–07. http://dx.doi.org/10.1136/thx.2007.085456
Sundblad BM, Larsson K, Nathell L . Low awareness of COPD among physicians. Clin Respir J 2008;2(1):11–16. http://dx.doi.org/10.1111/j.1752-699X.2007.00020.x
Gershon A, Croxford R, To T, et al. Trends in chronic obstructive pulmonary disease prevalence, incidence, and mortality in Ontario, Canada, 1996 to 2007: a population-based study. Arch Intern Med 2010;170(6):560–5. http://dx.doi.org/10.1001/archinternmed.2010.17
Danielsson P, Ólafsdóttir IS, Benediktsdóttir B, Gíslason T, Janson C . The prevalence of COPD in Uppsala, Sweden — The Burden of Obstructive Lung Disease (BOLD) study: cross-sectional population-based study. Clin Respir J 2012;6(2):120–7. http://dx.doi.org/10.1111/j.1752-699X.2011.00257.x
National Board of Health and Welfare. Socialstyrelsens riktlinjer för vård av astma och kroniskt obstruktiv lungsjukdom (KOL). Faktadokument och beslutsstöd för prioriteringar. 2004. Available from: www.socialstyrelsen.se
Larsson K, Janson C, Lisspers K, et al. Combination of budesonide/formoterol more effective than fluticasone/salmeterol in preventing exacerbations in chronic obstructive pulmonary disease: the PATHOS study. J Intern Med 2013;273(6):584–94. http://dx.doi.org/10.1111/joim.12067
Martinell M, Stålhammar J, Hallqvist J . Automated data extraction — a feasible way to construct patient registers of primary care utilization. Ups J Med Sci 2012;117(1):52–6. http://dx.doi.org/10.3109/03009734.2011.653015
Gingter C, Wilm S, Abholz HH . Is COPD a rare disease? Prevalence and identification rates in smokers aged 40 years and over within general practice in Germany. Fam Pract 2009;26(1):3–9. http://dx.doi.org/10.1093/fampra/cmn084
Charlson ME, Pompei P, Ales KL, MacKenzie CR . A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40(5):373–83. http://dx.doi.org/10.1016/0021-9681(87)90171-8
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43(11):1130–9. http://dx.doi.org/10.1097/01.mlr.0000182534.19832.83
Atsou K, Chouaid C, Hejblum G . Variability of the chronic obstructive pulmonary disease key epidemiological data in Europe: systematic review. BMC Med 2011;9:7. http://dx.doi.org/10.1186/1741-7015-9-7
Lisspers K, Ställberg B, Hasselgren M, Johansson G, Svärdsudd K . Organisation of asthma care in primary health care in mid-Sweden. Prim Care Respir J 2005;14(3):147–53. http://dx.doi.org/10.1016/j.pcrj.2005.03.003
Thorn J, Norrhall M, Larsson R, et al. Management of chronic obstructive pulmonary disease (COPD) in primary care: a questionnaire survey in western Sweden. Prim Care Respir J 2008;17(1):26–31. http://dx.doi.org/10.3132/pcrj.2008.00008
Löfdahl CG, Tilling B, Ekström T, Jörgensen L, Johansson G, Larsson K . COPD health care in Sweden — a study in primary and secondary care. Respir Med 2010;104(3):404–11. http://dx.doi.org/10.1016/j.rmed.2009.10.007
Mannino DM, Thorn D, Swensen A, Holguin F . Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J 2008;32(4):962–9. http://dx.doi.org/10.1183/09031936.00012408
Curkendall SM, Lanes S, de Luise C, et al. Chronic obstructive pulmonary disease severity and cardiovascular outcomes. Eur J Epidemiol 2006;21(11):803–13. http://dx.doi.org/10.1007/s10654-006-9066-1
Sidney S, Sorel M, Quesenberry CP Jr, DeLuise C, Lanes S, Eisner MD . COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser Permanente Medical Care Program. Chest 2005;128(4):2068–75. http://dx.doi.org/10.1378/chest.128.4.2068
Rycroft CE, Heyes A, Lanza L, Becker K . Epidemiology of chronic obstructive pulmonary disease: a literature review. Int J COPD 2012;7:457–94. http://dx.doi.org/10.2147/COPD.S32330
Sundh J, Janson C, Lisspers K, Montgomery S, Ställberg B . Clinical COPD Questionnaire score (CCQ) and mortality. Int J COPD 2012;7:833–42. http://dx.doi.org/10.2147/COPD.S38119
Pinnock H, Thomas M, Tsiligianni I, et al. The International Primary Care Respiratory Group's (IPCRG) Research Needs Statement 2010. Prim Care Respir J 2010;19(Suppl 1):S1–20. http://dx.doi.org/10.4104/pcrj.2010.00021
Acknowledgements
Handling editor Niels Chavannes
Statistical review Gopal Netuveli
The study was sponsored by AstraZeneca. English language editing and assistance with figures, funded by AstraZeneca, was provided by Anna Mett of inScience Communications, Springer Healthcare. The authors wish to direct a special appreciation to all the primary healthcare centres who contributed data to the present study.
Author information
Authors and Affiliations
Contributions
All authors participated equally in the study conception, design, and statistical analysis planning. BS was responsible for the manuscript draft and finalisation, and GJ for handling of data and the study database. All authors analysed and interpreted the data, revised the manuscript, had access to complete study data, and had authority over manuscript preparation, approval of final version, and the decision to submit for publication. KHL is guarantor.
Corresponding author
Ethics declarations
Competing interests
BS has received honoraria for educational activities from AstraZeneca, GlaxoSmithKline, Meda, Merck Sharp and Dohme, and has served on an advisory board arranged by AstraZeneca, Novartis, and Boehringer Ingelheim. He is an Associate editor of the PCRJ, but was not involved in the editorial review of, nor the decision to publish, this article. CJ has received honoraria for educational activities from AstraZeneca, GlaxoSmithKline, and Merck Sharp and Dohme. GJ has served on an advisory board arranged by AstraZeneca and Takeda. KL has served on an advisory board and/or served as a speaker and/or participated in education arranged by AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Meda, MSD, Nycomed, Novartis, and Pfizer. KL has also received unrestricted research grants from AstraZeneca, Boehringer Ingelheim, and GlaxoSmithKline. GS and GT are full-time employees of AstraZeneca Nordic. KHL has received speaking fees from AstraZeneca, Boehringer Ingelheim, and Merck Sharp and Dohme.
Rights and permissions
About this article
Cite this article
Ställberg, B., Janson, C., Johansson, G. et al. Management, morbidity and mortality of COPD during an 11-year period: an observational retrospective epidemiological register study in Sweden (PATHOS). Prim Care Respir J 23, 38–45 (2014). https://doi.org/10.4104/pcrj.2013.00106
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.4104/pcrj.2013.00106
This article is cited by
-
Diagnostic spirometry in COPD is increasing, a comparison of two Swedish cohorts
npj Primary Care Respiratory Medicine (2023)
-
COPD – do the right thing
BMC Family Practice (2021)
-
Patient outcomes following GPs’ educations about COPD: a cluster randomized controlled trial
npj Primary Care Respiratory Medicine (2020)
-
Hot and cold weather based on the spatial synoptic classification and cause-specific mortality in Sweden: a time-stratified case-crossover study
International Journal of Biometeorology (2020)
-
Long-term dietary fiber intake and risk of chronic obstructive pulmonary disease: a prospective cohort study of women
European Journal of Nutrition (2020)