Abstract
Objective
High-frequency oscillatory ventilation (HFOV) may reduce ventilator-induced lung injury in experimental neonatal respiratory distress. However, these data permit no conclusions for large animals or adult patients with acute respiratory distress syndrome (ARDS), because in neonates higher frequencies and lower amplitudes can be used, resulting in lower tidal volumes (VT) and airway pressures. The aim of this study was to compare gas exchange, lung histopathology and inflammatory cytokine expression during lung-protective pressure-controlled ventilation (PCV) and HFOV in a long-term large-animal model of ARDS.
Design
Prospective, randomized, controlled pilot study.
Setting
University animal laboratory.
Subjects
Sixteen female pigs (55.3 ± 3.9 kg).
Interventions
After induction of ARDS by repeated lavage, the animals were randomly assigned to PCV (VT = 6 ml/kg) and HFOV (6 Hz). After lung injury, a standardised lung recruitment was performed in both groups, and ventilation was continued for 24 h. Measurements and results: After lung recruitment sustained improvements in the oxygenation index were observed in both groups. The mean airway pressure (mPaw) was significantly lower in the HFOV group during the experiment ( p < 0.01). Histologically, lung inflammation was significantly ameliorated in the HFOV group ( p < 0.05). The messenger RNA expression of IL-1-β in lung tissue was significantly lower in the HFOV-treated animals ( p < 0.01).
Conclusions
These data suggest that HFOV compared with conventional lung-protective ventilation can reduce lung inflammation in a large-animal 24-h model of ARDS. Furthermore, it was shown that lung recruitment leads to sustained improvements in gas exchange with a significantly lower mPaw when HFOV is used.
Similar content being viewed by others
Introduction
Mechanical ventilation (MV) is the most important therapy in patients with acute respiratory distress syndrome (ARDS). However, MV of ARDS patients may cause or perpetuate lung injury, particularly if alveolar overdistension, repetitive collapse and reopening of damaged alveolar lung units occur [1, 2]. This concept has been termed ventilator-induced lung injury (VILI). Various lung-protective strategies to minimize VILI have been developed. One strategy uses conventional MV (CV) with lower tidal volumes (VT; 6 ml/kg predicted body weight) to limit volutrauma, while maintaining the lung open with sufficient positive end-expiratory pressure (PEEP) to prevent atelectrauma [3, 4]. In ARDS patients ventilated with a conventional lung-protective strategy, lower levels of inflammatory mediators and an absolute mortality reduction of 9% were found [5, 6].
Theoretically, high-frequency oscillatory ventilation (HFOV) is an optimal lung-protective strategy. The application of an extremely small VT, combined with a high mean airway pressure (mPaw), allows maintenance of alveolar recruitment while avoiding low end-expiratory pressure and high peak airway pressures [7, 8]. In small-animal models of respiratory distress, HFOV can improve gas exchange, cause more uniform lung recruitment and reduce VILI compared with CV [9–12]. However, in premature infants with neonatal respiratory distress syndrome (nRDS) the benefit of HFOV compared with CV, especially when CV is used with high respiratory rates (> 60/min) and minimal VT, seems to be limited [13, 14].
Although there are promising data from small-animal models indicating that HFOV might reduce VILI, these study results cannot be directly transferred to large animals or adult patients with ARDS. In nRDS, higher oscillatory frequencies and lower pressure amplitudes can be used, resulting in smaller tidal volumes and lower peak airway pressures [15]. In adults, HFOV can be safely applied and is associated with initial improvement of gas exchange, but with a complication rate similar to CV [16]. However, it is unclear whether HFOV reduces VILI in ARDS. The aim of this pilot study was to compare lung-protective pressure-controlled ventilation (PCV) with HFOV in terms of gas exchange, histological signs of lung injury and messenger RNA (mRNA) expression of inflammatory cytokines.
Material and methods
Animal preparation
The study was approved by the appropriate governmental institution and performed according to the guidelines of the National Institutes of Health. Sixteen female pigs (55.3 ± 3.9 kg) were included. Anaesthesia and instrumentation were as previously described [17]. Briefly, animals were intubated with a cuffed 8.5-mm ID endotracheal tube with an additional side lumen (Rueschelit®; Ruesch, Kernen, Germany). Anaesthesia and muscle relaxation were maintained with continuous infusion of 5–10 mg/kg/h thiopental, 0.01 mg/kg/h fentanyl and 0.1 mg/kg/h pancuronium throughout the experiment. The left carotid artery was cannulated to measure mean arterial pressure (MAP) and arterial blood gases (ABL 505®; Radiometer, Bronshoj, Denmark). For continuous registration of mean pulmonary artery pressure (MPAP) and mixed venous blood gases, a pulmonary artery catheter was inserted via a jugular sheath into a pulmonary artery and connected to a cardiac output computer (Explorer®; Edwards Lifescience, Irvine, CA, USA).
PCV was performed with a Servo® 900C ventilator (Siemens-Elema AB, Solna, Sweden) starting with a PEEP of 5 cmH2O, a VT of 6 ml/kg, a respiratory rate (RR) of 30/min and an inspiratory to expiratory ratio (I:E) of 1:1. The inspiratory oxygen fraction (FiO2) remained at 1.0. The core temperature was maintained at 38.0 ± 0.5 °C during the experiment by using a heating pad. A continuous infusion of 4–5 ml/kg/h balanced electrolyte solution was administered for adequate hydration during the experiment, and all animals received one dose of cefotaxime (100 mg/kg).
Experimental protocol
The study protocol of the experiment is outlined in Fig. 1. After instrumentation the animals were stabilized for 30 min and baseline measurements (TBaseline) were performed. ARDS was induced by bilateral pulmonary lavages with 30 ml/kg isotonic saline (38 °C), repeated every 10 min until PaO2 decreased to less than 60 torr (8.0 kPa) and remained stable for 60 min (TARDS) with unchanged ventilatory parameters. An average of 20 ± 4 lavages with approximately 30,000 ml saline per animal were necessary for ARDS induction.
Study protocol and time course. PCV, Pressure-controlled ventilation; HFOV, high-frequency oscillatory ventilation; ARDS, acute respiratory distress syndrome; PRM, post recruitment; FiO 2, fraction of inspired oxygen; PEEP, positive end-expiratory pressure; VT, tidal volume; RR, respiratory rate; I:E, inspiratory:expiratory ratio; mPaw, mean pulmonary airway pressure; PaO 2, arterial oxygen partial pressure; PaCO 2, carbon dioxide partial pressure
After stabilisation post-injury measurements (TARDS) were obtained and the animals were randomly assigned to one of the following treatment groups (n = 8/group):
-
1.
PCV: FiO2 = 1.0, PEEP = 5 cmH2O, VT = 6 ml/kg, RR = 30/min, I:E = 1:1
-
2.
HFOV: FiO2 = 1.0, bias flow = 30 l/min, amplitude = 60 cmH2O, frequency = 6 Hz, I:E = 1:1 (Sensor Medics 3100 B, Yorba Linda, CA, USA)
A bolus of 500 ml colloid solution (Voluven 6% HES 130/0.4; Fresenius Kabi, Bad Homburg, Germany) was given and a sustained inflation (SI) was applied by an expiratory hold for 60 s (PEEP 50 cmH2O) in the PCV group. In the HFOV group, the mean airway pressure (mPaw) was increased to 50 cmH2O without oscillation for 60 s. In both groups, the mPaw was then adjusted 3 cmH2O higher than after ARDS induction and increased in steps of 3 cmH2O until PaO2 no longer improved or began to fall. This was regarded as full lung inflation or the beginning of lung overdistension [13, 17, 18]. The mPaw was reduced by 3 cmH2O and post-recruitment measurements were obtained (TPRM). Lung recruitment was performed by altering PEEP during PCV and mPaw directly during HFOV. A 15-min equilibration period was maintained between each modification. The FiO2 was reduced stepwise to 0.4. When FiO2 was stable at 0.4, the mPaw was further decreased in steps of 3 cmH2O every 15 min until the PaO2 was in the target range of 90–110 torr (12.0–14.7 kPa). Oscillatory frequency was kept at 6 Hz. The amplitude (60–80 cmH2O) was altered as needed to keep the PaCO2 between 35 and 55 torr (4.7–7.37 kPa). The RR (30–40/min) in the animals of the PCV group was adequate to maintain the PaCO2 in thetarget range. Intrinsic PEEP (PEEPi) was measured at each time point by application of an expiratory occlusion manoeuvre (using the Servo ventilator's functionality during PCV versus clamping the endotracheal tube for 10 s and measuring the resulting intratracheal pressure during HFOV). VT was fixed at 6 ml/kg by modifying the peak inspiratory pressure (PIP) during PCV throughout the experiment.
Gas exchange and haemodynamic data were determined hourly and displayed at the following time points: TBaseline, TARDS, TPRM, 6, 12, 18 and 24 h. Intratracheal mPaw and PIP were measured in addition to the ventilator recording at the tubes tip using an air-filled pressure transducer referenced to atmospheric pressure and capable of detecting pressure changes at 6 Hz (PM8050®; Draeger, Luebeck, Germany). To compare the gas exchange between the groups the oxygenation index (OI) was calculated: OI = (FiO2 × mPaw (cmH2O) × 100)/PaO2 (torr) [19].
Histopathology
After 24 h the animals were killed with an overdose of thiopental and embutramid mebezonium iodide (T61®; Intervet, Unterschleissheim, Germany). The right lung was immediately removed, inflated with buffered 10% formalin at a pressure of 30 cmH2O and fixed in a buffered 10% formalin bath for 24 h. Slides from the upper, ventral and dorsal middle and lower lobes were stained with haematoxylin and eosin and examined by a pathologist blinded to the two groups. A four-point, semi-quantitative, severity-based scoring system was used (negative = 0, slight = 1, moderate = 2, severe = 3) [20]. The four main characteristics based on eight individual characteristics were atelectasis, oedema (interstitial oedema, lymphangiectasis, intra-alveolar exudate), inflammation (alveolar and interstitial neutrophil infiltration, interstitial lymphocyte infiltration) and congestive hyperaemia [20]. The scores of each parameter and lobe in the four main characteristics obtained from each investigated group were summarised and then divided by the number of animals and parameters. The four main characteristics were then averaged, resulting in the total lung injury score.
Semi-quantitative RT-PCR
Expression of TNF-α, Il-1-β, Il-6 and Il-10 was measured in the left lower posterior lung lobe using semi-quantitative reverse-transcription polymerase chain reaction (RT-PCR) technique. Total RNA was extracted as specified by the manufacturer (SV Total RNA Isolation System Kits; Promega®, Madison, USA) and measured using an Ultrospec 3000 UV/visible spectrophotometer (Biochrom Ltd., Buckinghamshire, UK), prior to cDNA synthesis (RevertAid® H Minus First Strand cDNA Synthesis Kit; Fermentas, St. Leon-Rot, Germany). The PCR mixture contained 3–5 μl cDNA, 1 μl of each cytokine gene primer (Table 1; forward/reverse primers, 10 pmol/μl each, annealing 58 °C), 12.5 μl PCR MasterMix (Promega®, Madison, USA) and Nuclease-Free Water up to a total volume of 25 μl. Gene expression was related to β-actin. The level of each product, loaded onto 1% agarose gels and stained with ethidium bromide, was semi-quantitatively evaluated using an image analysis system (BioDocAnalysis®-Software; Biometra, Germany). To compare the relative mRNA expression levels in each of the samples, the values are presented as the ratio of the band intensities of the cytokine RT product over the corresponding housekeeping RT product run simultaneously. Samples were run in duplicate.
Statistical analysis
The data were analysed using SigmaStat (Systat Software Inc., Point Richmond, USA) and expressed as mean ± SD. Two-way analysis of variance (ANOVA) for repeated measurements was used for analyses of gas exchange, respiratory parameters and haemodynamics. Student–Newman–Keuls post-hoc test was used for comparison of significant ANOVA results within and between the groups. Because histopathological and mRNA data were not distributed normally, nonparametric tests were performed, and data are shown as median with 25%/75% quartiles. Mann–Whitney rank sum test was used for comparison of the study groups. p-values of less than 0.05 were considered significant.
Results
There were no differences between groups in age and weight. Gas exchange and haemodynamic parameters did not differ between the groups before lung injury. After saline lavage, all animals developed severe respiratory failure (Table 2; p < 0.01). Two animals died due to pulmonary artery air embolism and were excluded from the analysis (one in each group). Detailed data regarding gas exchange, respiratory parameters and haemodynamics are presented in Tables 2 and 3.
Gas exchange and respiratory parameters
After recruitment, OI significantly improved in both groups and remained significantly improved over the 24-h study period compared with TARDS (Fig. 2a; p < 0.01). OI was significantly decreased during HFOV compared with PCV after 6 and 18 h (Fig. 2a; 6 h: p < 0.01, 18 h: p < 0.05). Intratracheal mPaw and PIP were significantly lower in the HFOV group compared with TARDS and the PCV group during the 24 h (Fig. 2b and Table 2; p < 0.01). In the PCV group, intratracheal mPaw and PIP were equal to the respirator recordings. PEEPi was always less than 1 cmH2O in both groups.
Oxygenation index and mean airway pressure over the 24-h study period. a Oxygenation index (OI). After recruitment and during the 24-h study course the OI was significantly improved compared with T ARDS in both groups (**p < 0.01). OI was significantly decreased in the HFOV group compared with the PCV group after 6 and 18 h (6 h: **p < 0.01; 18 h: *p < 0.05). b Mean airway pressure. The intratracheally measured mPaw was significantly reduced in the HFOV group compared with T ARDS and the PCV group during the 24 h (**p < 0.01, § § p < 0.01). PCV, Pressure controlled ventilation; HFOV, high-frequency oscillatory ventilation; SM, Sensor Medics oscillator; ARDS, acute respiratory distress syndrome; PRM, post recruitment. Data are presented as mean ± standard deviation
Haemodynamic variables
MAP, MPAP and CO were significantly higher after TARDS compared with TBaseline values and decreased significantly over the study period compared with TARDS in both groups (Table 3; p < 0.01). MPAP was significantly lower in the HFOV group after 6 h (Table 3; p < 0.01).
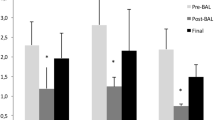
Histopathology
Figure 3 shows the semi-quantitative lung injury score. Animals treated with HFOV exhibited significantly fewer signs of inflammation than PCV animals at the end of the 24-h ventilation period (Fig. 3; p < 0.05). The total lung injury score was not different in both groups.
Semi-quantitative lung injury scores after 24 h. In animals receiving high-frequency oscillatory ventilation (HFOV) there was a significantly lower lung inflammation score than with pressure-controlled ventilation (PCV; § p < 0.05). Four main characteristics: atelectasis, oedema (based on interstitial oedema, lymphangiectasis, intra-alveolar exudate), inflammation (based on alveolar and interstitial neutrophil infiltration, interstitial lymphocyte infiltration) and congestive hyperaemia. Data are presented as median with interquartile range (25/75 percentiles)
Semi-quantitative RT-PCR
Amplification of template cDNA with primers specific for TNF-α, Il-1-β, Il-6 and Il-10 coding sequences resulted in products corresponding to the predicted size, namely, 199 bp (TNF-α), 256 bp (Il-1-β), 25 bp (Il-6) and 10 bp (Il-10). Representative bands are shown in Fig. 4. Normalized to β-actin, mRNA expression of IL-1-β was significantly reduced (Fig. 5; p < 0.01). No statistically significant differences in mRNA concentration of TNF-α, IL-6 and Il-10 could be detected.
RT-PCR analysis of mRNA for TNF-α, IL-1-β, IL-6 and IL-10 in the left lower posterior lung lobe after 24 h. Representative bands for TNF-α, IL-1-β, IL-6, IL-10 and β-actin. PCV, Pressure-controlled ventilation; HFOV, high-frequency oscillatory ventilation; TNF, tumour necrosis factor; IL, interleukin; M, marker
RT-PCR analysis of mRNA for TNF-α, IL-1-β, IL-6 and IL-10 in the left lower posterior lung lobe after 24 h. Normalized densitometric ratios of TNF-α, IL-1-β, IL-6 and IL-10 transcripts to β-actin. MRNA expression of IL-1-β was significantly reduced and expression of IL-6 tended to be lower in the HFOV group (§ p < 0.01). PCV, Pressure-controlled ventilation; HFOV, high-frequency oscillatory ventilation; TNF, tumour necrosis factor; IL, interleukin. Data are presented as median with interquartile range (25/75 percentiles)
Discussion
The major finding of this pilot study is that HFOV reduces histological signs of lung inflammation and lower mRNA expression of IL-1-β in lung tissue after 24 h of ventilation compared with PCV with low VT. Moreover, after lung recruitment sustained improvement in oxygenation was detectable in both groups, but intratracheal mPaw was significantly reduced in the HFOV compared with the PCV group.
Several small-animal studies demonstrated VILI reduction with HFOV compared with conventional lung-protective ventilation, but there is a paucity of information regarding outcome of HFOV in large-animal models [9, 10, 21]. The limitations of transferring these data to adult patients are that previous studies used different oscillatory frequencies, higher amplitudes and different endotracheal tube diameters [22–25].
The goal of this study was to compare gas exchange, lung histopathology and inflammatory cytokine expression resulting from two different lung-protective ventilation strategies. The PCV group was ventilated using low VT, and in the HFOV group the oscillatory frequency was set at 6 Hz with an amplitude of 60–80 cmH2O according to adult HFOV trials [16]. Lung volume was optimized by using increases in PaO2 as a crude surrogate for alveolar recruitment and avoidance of hyperinflation [12]. The recruitment was performed using an initial SI followed by a stepwise increase of mPaw as previously described [17, 18]. This manoeuvre resulted in a significant improvement of oxygenation in both study groups. After recruitment the FiO2 was decreased and the mPaw was titrated in a decremental fashion according to the oxygenation response in both groups [18]. In contrast to previous clinical ARDS studies using HFOV aiming at a SaO2 of 88–93%, we kept PaO2 between 90 and 110 torr and SaO2 > 97%, thereby assuming a more aerated lung [8, 23, 24].
HFOV and CV, used with an “open-lung” strategy (OLC), can improve gas exchange and reduce VILI [26, 27]. It is mandatory to maintain adequate lung volume after recruitment during HFOV [12]. Tidal recruitment and insufficient levels of PEEP during CV only temporarily improve oxygenation [28]. We found a significant and sustained improvement in gas exchange and OI in both groups after recruitment during the entire 24-h study period, supporting an “open lung” approach. It was shown that hypercapnia can attenuate whereas hypocapnia may worsen lung injury [29, 30]. Therefore, mild hypercapnia was tolerated.
To our knowledge, this is the first report of a large-animal ARDS study demonstrating that animals subjected to HFOV develop significantly less histological lung inflammation than those ventilated with conventional lung-protective ventilation. Our results are in accordance with previous studies of HFOV in small animals: Imai et al. and Yoder et al. demonstrated a significant improvement in the histopathologic appearance of the lung [9, 21]. Until now, there is only one large-animal study, in which HFOV and CV was provided in a lung-protective manner including an OLC [31]. In the 4-h study period, a trend toward greater lung injury in pilot histological data during PCV than with HFOV was found. The authors concluded that possibly the study time was too short to show any significant differences between two protective ventilatory strategies. Using a similar ventilatory strategy, we found no signs of atelectasis in both groups, assuming that the PEEP level in the PCV group and the mPaw in the HFOV group were sufficient to keep lungs open. The significant reduction in histological lung inflammation during HFOV might be an indicator for further lung protection. However, these results are in contrast to previous small-animal studies comparing CV and HFOV using standardised volume recruitment techniques [27, 32]. They found comparable gas exchange and pathologic outcomes during CV with lung recruitment and during HFOV. It was concluded that lung recruitment and maintenance of lung volumes is more important than the mode of ventilation [32]. Similarly, in surfactant-depleted piglets, using the same recruitment strategy and target PaO2 values as in our study, no differences in lung injury between CV and HFOV were found [18]. In all studies, the mPaw during HFOV was similar or higher than during CV. In our study, mPaw recorded at the respirator was identical in both groups. As the intrapulmonary pressure tends to be lower than the continuous distension pressure (CDP) set with the HFOV respirator, intratracheally measured mPaw was significantly lower in the HFOV animals [33]. This mPaw was sufficient to achieve gas exchange equivalent to that with PCV with moderately high PEEP levels. It could have caused less mechanical stress, thereby reducing histological signs of lung inflammation. However, it remains difficult to assess optimal CDP during HFOV [34]. Furthermore, the maximum study period of the mentioned investigations was only 6 h. It is possible that differences in lung injury between two ventilatory strategies that are basically lung protective need more time to become detectable if histological methods are used.
Mechanical stress, induced by mechanical ventilation during treatment of lung injury, can upregulate cytokine production in the lungs, thus resulting in an inflammatory reaction aggravating ARDS [6, 21, 35]. In our study, the mRNA expression of IL-1-β was significantly reduced in the lung tissue of HFOV-ventilated animals. Our results are in line with previous results showing reduced mRNA expression of the pro-inflammatory cytokines IL-1-β, IL-6 and IL-8, and elevated mRNA expression of the anti-inflammatory IL-10 in small animals ventilated with HFOV [10, 35]. These cytokine reductions were noted despite similar mPaw during HFOV and CV, and—as in our study—the effective mPaw being lower during HFOV [10, 35].
In adult patients alveolar flooding but not surfactant deficiency is the predominant mechanism in ARDS development. It is known that surfactant-depleted collapsed lungs respond better to PEEP application and lung recruitment than lungs with alveolar flooding [36]. After recruitment, we were able to maintain adequate oxygenation with mild airway pressures in both groups. This weakens the transferability of our data to clinical practice. Furthermore, several variables describing lung injury were tested, and statistically significant results in single tests should be interpreted with care.
Conclusions
The present pilot study shows for the first time in a large-animal model of ARDS that HFOV may reduce lung inflammation more than conventional lung-protective ventilation. This was demonstrated histologically by amelioration of lung inflammation and lower mRNA expression of IL-1-β in lung tissue after 24 h. Furthermore, it was shown that lung recruitment leads to sustained improvements in gas exchange both in conventional lung-protective ventilation and in HFOV. However, during HFOV a significantly lower mPaw is needed. Further studies focussing on the inflammatory reaction in lung tissue are needed to confirm the results of this pilot study.
References
Pinhu L, Whitehead T, Evans T, Griffiths M (2003) Ventilator-associated lung injury. Lancet 361(9354):332–340
Tremblay LN, Miatto D, Hamid Q, Govindarajan A, Slutsky AS (2002) Injurious ventilation induces widespread pulmonary epithelial expression of tumor necrosis factor-alpha and interleukin-6 messenger RNA. Crit Care Med 30:1693–1700
Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
Slutsky AS (1999) Lung injury caused by mechanical ventilation. Chest 116(Suppl 1):9s–15s
[No authors listed] (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 342:1301–1308
Ranieri VM, Giunta F, Suter PM, Slutsky AS (2000) Mechanical ventilation as a mediator of multisystem organ failure in acute respiratory distress syndrome. JAMA 284:43–44
Ferguson ND, Stewart TE (2001) The use of high-frequency oscillatory ventilation in adults with acute lung injury. Respir Care Clin North Am 7:647–661
Froese AB (1997) High-frequency oscillatory ventilation for adult respiratory distress syndrome: let's get it right this time! Crit Care Med 25:906–908
Imai Y, Nakagawa S, Ito Y, Kawano T, Slutsky AS, Miyasaka K (2001) Comparison of lung protection strategies using conventional and high-frequency oscillatory ventilation. J Appl Physiol 91:1836–1844
von der Hardt K, Kandler MA, Fink L, Schoof E, Dotsch J, Brandenstein O, Bohle RM, Rascher W (2004) High frequency oscillatory ventilation suppresses inflammatory response in lung tissue and microdissected alveolar macrophages in surfactant depleted piglets. Pediatr Res 55:339–346
deLemos RA, Coalson JJ, Meredith KS, Gerstmann DR, Null DM Jr (1989) A comparison of ventilation strategies for the use of high-frequency oscillatory ventilation in the treatment of hyaline membrane disease. Acta Anaesthesiol Scand (Suppl) 90:102–107
McCulloch PR, Forkert PG, Froese AB (1988) Lung volume maintenance prevents lung injury during high frequency oscillatory ventilation in surfactant-deficient rabbits. Am Rev Respir Dis 137:1185–1192
Courtney SE, Durand DJ, Asselin JM, Hudak ML, Aschner JL, Shoemaker CT (2002) High-frequency oscillatory ventilation versus conventional mechanical ventilation for very-low-birth-weight infants. N Engl J Med 347:643–652
Thome UH, Carlo WA, Pohlandt F (2005) Ventilation strategies and outcome in randomised trials of high frequency ventilation. Arch Dis Child Fetal Neonatal Ed 90:F466–F473
Sedeek KA, Takeuchi M, Suchodolski K, Kacmarek RM (2003) Determinants of tidal volume during high-frequency oscillation. Crit Care Med 31:227–231
Downar J, Mehta S (2006) Bench-to-bedside review: high-frequency oscillatory ventilation in adults with acute respiratory distress syndrome. Crit Care 10:240
Muellenbach RM, Kredel M, Zollhoefer B, Wunder C, Roewer N, Brederlau J (2006) Sustained inflation and incremental mean airway pressure trial during conventional and high-frequency oscillatory ventilation in a large porcine model of acute respiratory distress syndrome. BMC Anesthesiol 6:8
Krishnan RK, Meyers PA, Worwa C, Goertz R, Schauer G, Mammel MC (2004) Standardized lung recruitment during high frequency and conventional ventilation: similar pathophysiologic and inflammatory responses in an animal model of respiratory distress syndrome. Intensive Care Med 30:1195–1203
Hallman M, Merritt TA, Jarvenpaa AL, Boynton B, Mannino F, Gluck L, Moore T, Edwards D (1985) Exogenous human surfactant for treatment of severe respiratory distress syndrome: a randomized prospective clinical trial. J Pediatr 106:963–969
Merz U, Kellinghaus M, Hausler M, Pakrawan N, Klosterhalfen B, Hornchen H (2000) Partial liquid ventilation with surfactant: effects on gas exchange and lung pathology in surfactant-depleted piglets. Intensive Care Med 26:109–116
Yoder BA, Siler-Khodr T, Winter VT, Coalson JJ (2000) High-frequency oscillatory ventilation: effects on lung function, mechanics, and airway cytokines in the immature baboon model for neonatal chronic lung disease. Am J Respir Crit Care Med 162:1867–1876
Clark RH (2000) High-frequency oscillatory ventilation in pediatric respiratory failure: a multicenter experience. Crit Care Med 28:3941–3942
Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG, Carlin B, Lowson S, Granton J (2002) High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. Am J Respir Crit Care Med 166:801–808
Ferguson ND, Chiche JD, Kacmarek RM, Hallett DC, Mehta S, Findlay GP, Granton JT, Slutsky AS, Stewart TE (2005) Combining high-frequency oscillatory ventilation and recruitment maneuvers in adults with early acute respiratory distress syndrome: the Treatment with Oscillation and an Open Lung Strategy (TOOLS) Trial Pilot Study. Crit Care Med 33:479–486
Gerstmann DR, Minton SD, Stoddard RA, Meredith KS, Monaco F, Bertrand JM, Battisti O, Langhendries JP, Francois A, Clark RH (1996) The Provo Multicenter Early High-Frequency Oscillatory Ventilation Trial: improved pulmonary and clinical outcome in respiratory distress syndrome. Pediatrics 98:1044–1057
Rimensberger PC, Pache JC, McKerlie C, Frndova H, Cox PN (2000) Lung recruitment and lung volume maintenance: a strategy for improving oxygenation and preventing lung injury during both conventional mechanical ventilation and high-frequency oscillation. Intensive Care Med 26:745–755
van Kaam AH, de Jaegere A, Haitsma JJ, Van Aalderen WM, Kok JH, Lachmann B (2003) Positive pressure ventilation with the open lung concept optimizes gas exchange and reduces ventilator-induced lung injury in newborn piglets. Pediatr Res 53:245–253
Froese AB, McCulloch PR, Sugiura M, Vaclavik S, Possmayer F, Moller F (1993) Optimizing alveolar expansion prolongs the effectiveness of exogenous surfactant therapy in the adult rabbit. Am Rev Respir Dis 148:569–577
Broccard AF, Hotchkiss JR, Vannay C, Markert M, Sauty A, Feihl F, Schaller MD (2001) Protective effects of hypercapnic acidosis on ventilator-induced lung injury. Am J Respir Crit Care Med 164:802–806
Laffey JG, Engelberts D, Kavanagh BP (2000) Injurious effects of hypocapnic alkalosis in the isolated lung. Am J Respir Crit Care Med 162:399–405
Sedeek KA, Takeuchi M, Suchodolski K, Vargas SO, Shimaoka M, Schnitzer JJ, Kacmarek RM (2003) Open-lung protective ventilation with pressure control ventilation, high-frequency oscillation, and intratracheal pulmonary ventilation results in similar gas exchange, hemodynamics, and lung mechanics. Anesthesiology 99:1102–1111
Gommers D, Hartog A, Schnabel R, de Jaegere A, Lachmann B (1999) High-frequency oscillatory ventilation is not superior to conventional mechanical ventilation in surfactant-treated rabbits with lung injury. Eur Respir J 14:738–744
Gerstmann DR, Fouke JM, Winter DC, Taylor AF, deLemos RA (1990) Proximal, tracheal, and alveolar pressures during high-frequency oscillatory ventilation in a normal rabbit model. Pediatr Res 28:367–373
Andrews P, Azoulay E, Antonelli M, Brochard L, Brun-Buisson C, Dobb G, Fagon JY, Gerlach H, Groeneveld J, Mancebo J, Metnitz P, Nava S, Pugin J, Pinsky M, Radermacher P, Richard C, Tasker R (2006) Year in review in Intensive Care Medicine, 2005. III. Nutrition, pediatric and neonatal critical care, and experimental. Intensive Care Med 32:490–500
Imai Y, Kawano T, Miyasaka K, Takata M, Imai T, Okuyama K (1994) Inflammatory chemical mediators during conventional ventilation and during high frequency oscillatory ventilation. Am J Respir Crit Care Med 150:1550–1554
Kloot TE, Blanch L, Melynne Youngblood A, Weinert C, Adams AB, Marini JJ, Shapiro RS, Nahum A (2000) Recruitment maneuvers in three experimental models of acute lung injury. Effect on lung volume and gas exchange. Am J Respir Crit Care Med 161:1485–1494
Acknowledgements
The authors thank Alois Reichert for technical support, Brigitte Paul and Juergen Schoell for logistics, Margret Wechner for laboratory assistance, Justus Mueller for pathological advice, and Karin Ulrichs, PhD for organisational support. This work was supported by departmental funding from the Department of Anaesthesiology, University of Wuerzburg, Wuerzburg, Germany.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-007-0706-z.
Rights and permissions
About this article
Cite this article
Muellenbach, R.M., Kredel, M., Said, H.M. et al. High-frequency oscillatory ventilation reduces lung inflammation: a large-animal 24-h model of respiratory distress. Intensive Care Med 33, 1423–1433 (2007). https://doi.org/10.1007/s00134-007-0708-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0708-x